AIMS To give you basic knowledge of Advance Advance Care Planning - PDF document
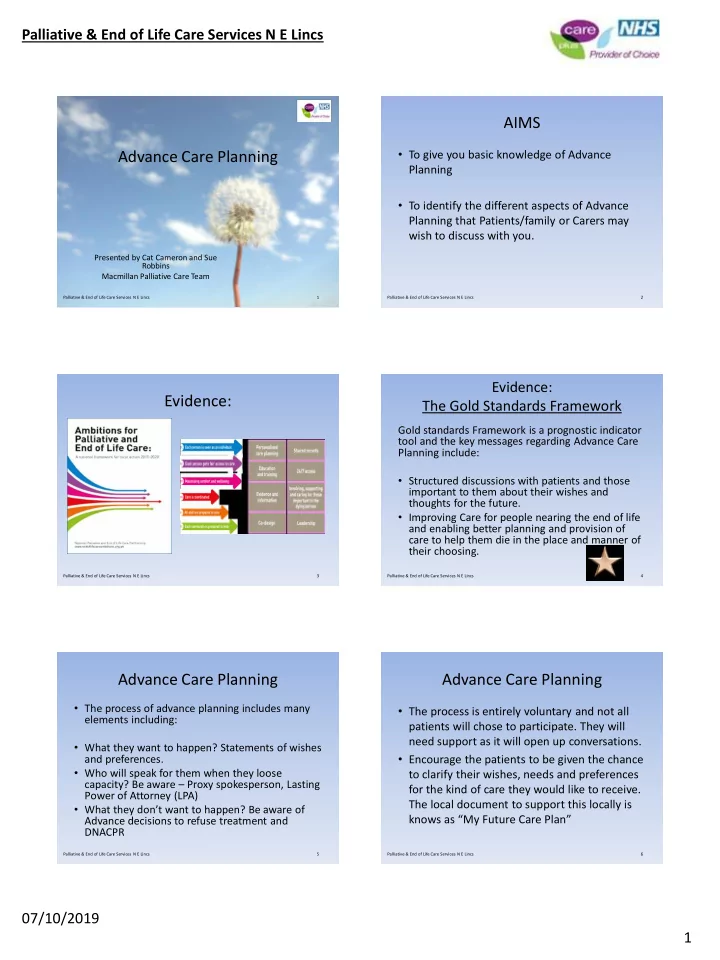
Palliative & End of Life Care Services N E Lincs AIMS To give you basic knowledge of Advance Advance Care Planning Planning To identify the different aspects of Advance Planning that Patients/family or Carers may wish to discuss
Palliative & End of Life Care Services N E Lincs AIMS • To give you basic knowledge of Advance Advance Care Planning Planning • To identify the different aspects of Advance Planning that Patients/family or Carers may wish to discuss with you. Presented by Cat Cameron and Sue Robbins Macmillan Palliative Care Team Palliative & End of Life Care Services N E Lincs Palliative & End of Life Care Services N E Lincs 1 1 Palliative & End of Life Care Services N E Lincs 2 Evidence: Evidence: The Gold Standards Framework Gold standards Framework is a prognostic indicator tool and the key messages regarding Advance Care Planning include: • Structured discussions with patients and those important to them about their wishes and thoughts for the future. • Improving Care for people nearing the end of life and enabling better planning and provision of care to help them die in the place and manner of their choosing. Palliative & End of Life Care Services N E Lincs 3 Palliative & End of Life Care Services N E Lincs 4 Advance Care Planning Advance Care Planning • The process of advance planning includes many • The process is entirely voluntary and not all elements including: patients will chose to participate. They will need support as it will open up conversations. • What they want to happen? Statements of wishes • Encourage the patients to be given the chance and preferences. • Who will speak for them when they loose to clarify their wishes, needs and preferences capacity? Be aware – Proxy spokesperson, Lasting for the kind of care they would like to receive. Power of Attorney (LPA) The local document to support this locally is • What they don’t want to happen? Be aware of knows as “My Future Care Plan” Advance decisions to refuse treatment and DNACPR Palliative & End of Life Care Services N E Lincs 5 Palliative & End of Life Care Services N E Lincs 6 07/10/2019 1
Palliative & End of Life Care Services N E Lincs Local Document Topics include • Preferred place of care/death (PPC/PPD) • DNACPR decisions • Beliefs, values and wishes • Financial affairs in order: Wills etc • Wishes following death :funeral etc. Palliative & End of Life Care Services N E Lincs 7 Palliative & End of Life Care Services N E Lincs 8 Sue Advance Care Planning • A fewer number might wish to describe specific medical interventions they don’t want to happen, through Advanced Decisions to Refuse Treatments (ADRT). • Most will also wish to say who might speak for them- this is important particularly if it is related to the development of future incapacity, but is important for all to express their wishes. Palliative & End of Life Care Services N E Lincs 9 Palliative & End of Life Care Services N E Lincs 10 Cat Case Study 1 Barbara Barbara had a long, brave battle with cancer and Heart failure. She was initially admitted to hospital for feeling generally unwell, but it quickly became evident through assessment and scans that she had significant disease progression and , sadly no further treatment options were available and she was discharged home. Palliative & End of Life Care Services N E Lincs 11 Palliative & End of Life Care Services N E Lincs 12 07/10/2019 2
Palliative & End of Life Care Services N E Lincs Barbara-Case Study 1 Barbara Case Study 1 • You support Barbara to break her bad news to • Barbara was a self confessed glamazon, and her family. Her wishes are to die at home, her biggest fear was dying without her lippy surrounded by her family, her dogs and her on. Her other main concerns was telling her “pretty things”. Her family were family who lived away about the reality of her understandably upset. Following this diagnosis for fear she would be perceived as conversation her family said that they were giving up. She asked if you could support her scared to talk to Barbara about her wishes in in having the conversations with her family case they upset her. This is a prime example of and with telling them she was dying. the burden that families feel when it comes to open and honest communication. Palliative & End of Life Care Services N E Lincs 13 Palliative & End of Life Care Services N E Lincs 14 Barbara- Case Study 1. Barbara Case Study 1 • After seeking consent, you liaise with • Barbara stated that at a time when she felt Barbara's GP and Community Team and listen she was loosing control with her illness that to Barbara's wishes. DNACPR and anticipatory she actually felt she had also gained control medication are explained and put in place. with having the opportunity to plan and You support Barbara and her family with the discuss her wishes. She commented that this “My Future Care Plan” booklet. Barbara's also would take this burden out of her families family all supported Barbara by all filling one hands and that she didn’t feel alone, she felt in with Barbara at the same time and even supported with her decisions and understood. added in some light humour and this brought the family closer together. Palliative & End of Life Care Services N E Lincs 15 Palliative & End of Life Care Services N E Lincs 16 Barbara Case Study 1 Barbara Case Study 1 • When it became evident that Barbara was Bereavement visit: Barbara's family afterwards said they never really actively dying everything was put in place as understood what the phrase a “good” death meant, Barbara had wished. Her symptoms where until it happened to their loved one. When well managed, she had a face full of make-up someone has terminal cancer or a chronic illness, it can feel like all the power has been stolen away with her lippy on and was surrounded by her from you. In that context, giving someone genuine family, her dogs and her pretty things. choice about how they are cared for and where they spend their last days and hours, can have a huge impact not just on the individual, but also on the people around them. Palliative & End of Life Care Services N E Lincs 17 Palliative & End of Life Care Services N E Lincs 18 07/10/2019 3
Palliative & End of Life Care Services N E Lincs Family members final comments on Loss of capacity and ACP: the bereavement visit. • Advance care planning has the potential to improve end of life care by enabling patients • “Once we knew that our Mums cancer and to discuss and record their future health and heart failure was progressing and was care wishes whilst they have Capacity to do so incurable, no one could stop her dying but and by doing so hopefully this can try and they could – and did- give her a good death. It prevent crisis situations occurring at end of is one of the greatest gifts anyone has ever life. given our family” Palliative & End of Life Care Services N E Lincs 19 Palliative & End of Life Care Services N E Lincs 20 Case Study 2 - Frank Case Study 2 - Frank • Frank is 52yrs and diagnosed with an advanced inoperable brain tumour and was told that he only has weeks to live. His family visit every day. • Sadly for many people, care and support at the The conversation of prognosis and advance care end of life is not something they know they can plan for, instead many people fear pain and planning was never discussed with Frank or his isolation they will experience in their dying days. family when he had capacity. Frank never For example Frank had no idea that pain discussed his wishes with his family. He was management for his headaches was something discharged home from Hospital with no DNACPR he could plan for. This could have been discussed form, no anticipatory medications and no support and put in place if effective communication with from services being offered. Frank and his family had taken place. Palliative & End of Life Care Services N E Lincs 21 Palliative & End of Life Care Services N E Lincs 22 Case Study 2 - Frank Case Study 2 - Frank • No advance planning had taken place with professionals • Frank was discharged home, a few days before • Although the family knew Frank was poorly they Frank died his family hit a crisis. Frank became unconscious and they were unable to cope. His didn’t realise he was end of life and rang 999. family panicked and stated that they felt alone Frank was admitted back to hospital but died in and didn’t know where to turn or what to do. the ambulance before he got there. DNACPR was Franks family where burnt out caring for him, not in place so resuscitation was attempted and they didn’t realise how poorly he was as no one was unsuccessful . Family where distraught and had discussed this with them, no equipment was left with the shock and anger of why this had in the home to support him. been allowed to happen? Palliative & End of Life Care Services N E Lincs 23 Palliative & End of Life Care Services N E Lincs 24 07/10/2019 4
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.