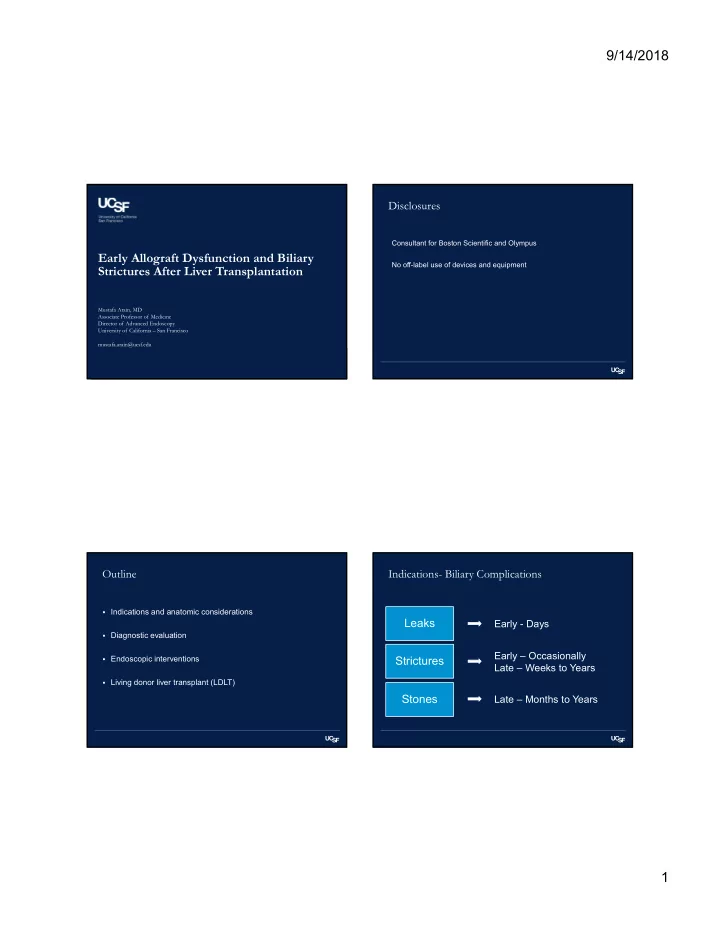
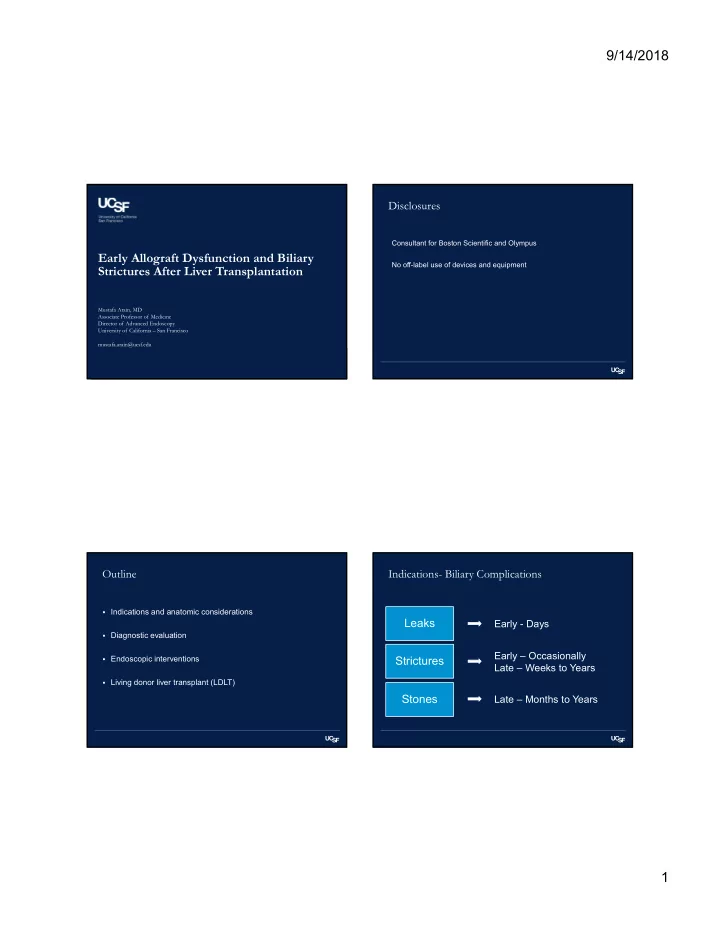
9/14/2018 Disclosures Consultant for Boston Scientific and Olympus Early Allograft Dysfunction and Biliary No off-label use of devices and equipment Strictures After Liver Transplantation Mustafa Arain, MD Associate Professor of Medicine Director of Advanced Endoscopy University of California – San Francisco mustafa.arain@ucsf.edu Outline Indications- Biliary Complications Indications and anatomic considerations Leaks Early - Days Diagnostic evaluation Early – Occasionally Endoscopic interventions Strictures Late – Weeks to Years Living donor liver transplant (LDLT) Stones Late – Months to Years 1
9/14/2018 ERCP for elevated LFTs and suspected Anatomic Considerations anastomotic stricture Ductal anatomy Air in the ? Stricture biliary tree Type of surgery – type of liver donation Understanding of segmental and sectoral anatomy Patient with a Roux-en-Y Hepatico-jejunosotomy Ductal Anatomy Ductal Anatomy Roux-en-Y hepatico- Choledocho- dochal jejunostomy anastomosis - Enteroscopy assisted - Aka duct to duct (DD) ERCP anastomosis Donor duct - Need to reach jejuno- - Most common Anastomosis jejunal anastomosis and - Easy endoscopic access (with stricture) then advance the scope - Availability of a wide up the biliary limb selection of accessories and - Limited accessories stents Recipient duct 2
9/14/2018 Donor variation Sectoral Ductal Anatomy Left hepatic duct Complete Partial Liver sector II, III and IV - Deceased donor liver (DD) Living donor transplant (LDLT) Right anterior sector - Right lobe Donor after cardiac death V and VIII - Smaller duct caliber – (DCD) - increased complications vs - Increased risk of biliary DD complications vs DD Right posterior sector Split liver transplant (SLD) - VI and VII - Left or right lobe Imaging Modalities Diagnosis Clinical suspicion early post-operatively Ultrasound Nuclear medicine scan CT Asymptomatic – incidental finding on routine labs/imaging MRCP EUS Symptoms – pain, fever, jaundice, pruritis ERCP PTC Labs Elevated LFTs Signs of infection Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 3
9/14/2018 Imaging Modalities Imaging Modalities Ductal dilation on US, Ultrasound Ultrasound Doppler for vascular Nuclear medicine scan Nuclear medicine scan Biliary leak evaluation abnormalities CT CT MRCP MRCP EUS EUS ERCP ERCP PTC PTC Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 Nuclear Medicine Hepatobiliary Scan 4
9/14/2018 Surgical Drain Nuclear Medicine Hepatobiliary Scan Surgical Drain Surgical Drain 5
9/14/2018 Imaging Modalities Imaging Modalities Ultrasound Ultrasound Nuclear medicine scan Nuclear medicine scan Fluid collections/ abscesses CT CT MRCP MRCP Main diagnostic study EUS EUS ERCP ERCP PTC PTC Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 MRCP ( Magnetic Resonance Cholangiopancreatograpy) MRCP Non-invasive, non-contrast • Limitations Evaluation of entire biliary tree • - Pacemaker/ICD Provides a roadmap of anatomy prior to intervention • - Patient compliance, claustrophobia High sensitivity for determining strictures and stones • - Small stones may be missed Newer contrast media allows dynamic imaging of the biliary system • - May falsely suggest stricture at anastomotic site - Contrast MRI Nephrogenic systemic sclerosis Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Yeh BM et al. Radiographics 2009, Seale MK et al. Radiographics 2009, Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 Boraschi P et al. Clin Transplant 2010, Beltran MM et al. Transplant Proc 2005 6
9/14/2018 MRCP: Anastomotic stricture in LDLT 7
9/14/2018 Imaging Modalities Ultrasound Nuclear medicine scan CT Rarely done early, can be MRCP EUS done to evaluate ERCP biliary/pancreatic diseases PTC Imaging Modalities Biliary Strictures Ultrasound Non-anastomotic strictures Anastomotic Nuclear medicine scan CT Upstream from biliary anastomosis, Short, focal stricture, at the bile MRCP involve intrahepatic ducts/branches duct anastomosis EUS Therapeutic procedures, Deceased Donor: 5-15%, Donor ERCP should NOT be considered Occur in 5-10 % of patients with after cardiac death: 20-33% PTC deceased donor transplantation diagnostic studies Multiple etiologies - Ischemia plays a major role Scarring and fibrosis - Associated with HA stenosis/occlusion, PV occlusion, CMV, PSC, ABO incompatibility, chronic rejection Arain MA et al. Liver Transpl 19:482–498, 2013, Koneru B. Liver Transpl 2006;12:702-704 Duffy JP et al. Ann Surg 2010;252:652-661, Ayoub WS et al. Dig Dis Sci 2010;55: 1540-1546 8
9/14/2018 Biliary Strictures Anastomotic Stricture on MRCP Non-anastomotic strictures Anastomotic Difficult to treat Respond well to endoscopic therapy Require prolonged treatment often 12 months or more with multiple endoscopic procedures Increased morbidity, decreased graft survival Arain MA et al. Liver Transpl 2013, Koneru B. Liver Transpl 2006, Buxbaum JL et al GIE 2011 Duffy JP et al. Ann Surg 2010, Ayoub WS et al. Dig Dis Sci 2010 ERCP Balloon dilation of the stricture 9
9/14/2018 Multiple stents across the stricture High grade Anastomotic Stricture No filling above the stricture initially Wire passage across the stricture 10
9/14/2018 Proximal filling Balloon Dilation Fully covered metal biliary stent 11
9/14/2018 Principles of Stricture Management Sphincterotomy → Balloon dilation → Stent placement Resolution Repeat ERCP q2-3 months and place maximal number of large caliber stents (10 Fr) until stricture resolves Consider fully covered metallic biliary stents for high grade, resistant strictures or as first line therapy - associated with fewer number of procedures* (two recent randomized trials) Graziadei IW et al. Liver Transpl 2006, Rizk RS et al. Gastrointest Endosc 1998, Morelli J et al. Gastrointest Endosc 2003, Costamagna G et al. Gastrointest Endosc 2001, *Cote G et al. JAMA 2016, *Tal AO et al. GIE 2017 ERCP early post-op, low platelets CBD stricture Pancreatic duct Pancreatic duct stent cannulation 12
9/14/2018 Biliary stents Pancreatic stent Balloon dilation of the biliary orifice Difficult Stricture: PTC aided treatment Percutaneous transhepatic balloon dilation 13
9/14/2018 Percutaneous transhepatic balloon dilation Non-anastomotic Strictures Filling of all three sectoral ducts 14
9/14/2018 Balloon dilation: Right posterior hepatic duct Balloon dilation: Right anterior hepatic duct Balloon dilation: left hepatic duct 10 Fr stents in all sectoral ducts 15
9/14/2018 Ischemic Cholangiopathy – 3 mo post Ischemic Cholangiopathy – 3 mo post Ischemic Cholangiopathy – 3 mo post Ischemic Cholangiopathy – 3 mo post 16
9/14/2018 ‘Resolution’ after 8 ERCPs… DCD complicated by HA stenosis MRCP – Ischemic cholangiopathy Central scarring extending into the intrahepatic branches No specific target for endoscopic therapy 17
9/14/2018 Post-transplant Bile Leaks Bile leak – Duct to duct anastomosis Up to 25% of patients Etiology - Anastomotic site leak - Ischemic injury - T-tube insertion (if done) - Surface leak Associated with fluid collections, abscesses Generally, respond to intensive endoscopic therapy - however, high rate of PTC and surgery reported in the literature Arain MA et al. Liver Transpl 19:482–498, 2013, Koneru B. Liver Transpl 2006;12:702-704 Duffy JP et al. Ann Surg 2010;252:652-661, Ayoub WS et al. Dig Dis Sci 2010;55: 1540-1546 18
9/14/2018 Bile leak – Duct to duct anastomosis Bile leak – Duct to duct anastomosis Percutaneous drain CBD Anastomotic leak Pancreatic wire Bile leak – Duct to duct anastomosis Biliary Leak CBD and PD stents 19
Recommend
More recommend