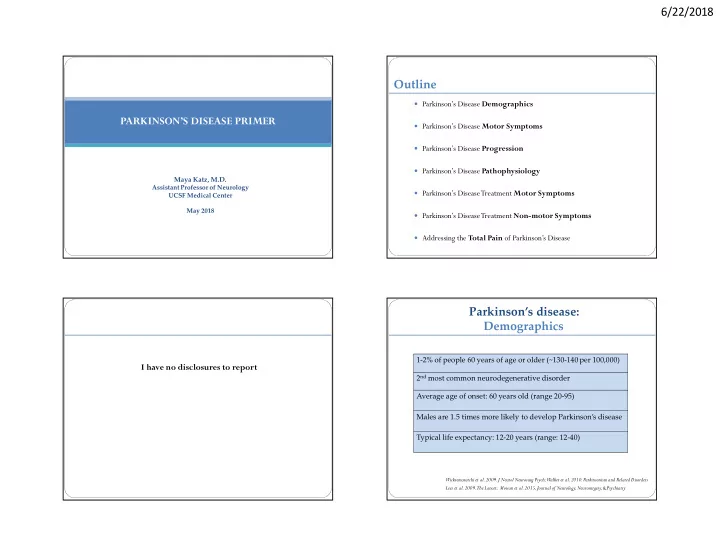
6/22/2018 Outline Parkinson’s Disease Demographics PARKINSON’S DISEASE PRIMER Parkinson’s Disease Motor Symptoms Parkinson’s Disease Progression Parkinson’s Disease Pathophysiology Maya Katz, M.D. Assistant Professor of Neurology Parkinson’s Disease Treatment Motor Symptoms UCSF Medical Center May 2018 Parkinson’s Disease Treatment Non-motor Symptoms Addressing the Total Pain of Parkinson’s Disease Parkinson’s disease: Demographics 1-2% of people 60 years of age or older (~130-140 per 100,000) I have no disclosures to report 2 nd most common neurodegenerative disorder Average age of onset: 60 years old (range 20-95) Males are 1.5 times more likely to develop Parkinson’s disease Typical life expectancy: 12-20 years (range: 12-40) Wickremaratchi et al. 2009. J Neurol Neurosurg Psych; Walker et al. 2010. Parkinsonism and Related Disorders Lees et al. 2009. The Lancet; Moisan et al. 2015, Journal of Neurology, Neurosurgery, & Psychiatry 1
6/22/2018 Cardinal PD Motor Symptoms: Essential Tremor Tremor Cardinal PD Motor Symptoms: Cardinal PD Motor Symptoms: Bradykinesia Gait Impairment 2
6/22/2018 Parkinson’s Disease: Parkinson’s Disease: Motor Fluctuations Motor Fluctuations OFF MEDICATIONS ON MEDICATIONS Parkinson’s Disease Progression: Parkinson’s Disease: Motor Fluctuations Dyskinesias Cenci, 2014, Frontiers Neurology 3
6/22/2018 Parkinson’s Disease Progression: Hoehn & Yahr Staging Cognitive deficits: Prevalence and clinical course Stage 1: ~2 years Stage 3: ~2 years Unilateral involvement Mild to moderate Normal PD-MCI PD Dementia (PDD) bilateral involvement, Postural instability, Stage 2: ~7 years Still independent Mild bilateral PD-MCI: primarily nonamnestic single domain impairment involvement Stage 4: ~2 years Severe disability, Stage 5: ~2 years • ~30% meet criteria for PD-MCI within 3 years after diagnosis Needs an assistive • device to walk or stand ~50% meet criteria for PD-MCI after 5 years Wheelchair bound or bedridden Can only ambulate with another person assisting Zhao et al. 2010, Mov Disord Litvan et al., 2011, Mov Disord; Litvan et al., 2012, Mov Disord; Marras et al. 2013, Mov Disord Parkinson’s disease pathology: Parkinson’s disease pathology: Substantia nigra pars compacta degeneration DaTSCAN DaTSCANs detect presynaptic dopaminergic neuronal loss using SPECT imaging Measures Ioflupane ( 123 I), which is a DAT ligand that binds to presynaptic dopamine Parkinson’s disease Normal transporters in the striatum UCSF Department of Pathology de la Feunte-Fernandez 2012. Neurology; Fang and Martin, 2015, Parkinsonism and Related Disorders; Scarr et al., 2013, Front. Cell. Neurosci. 4
6/22/2018 Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Medications Medications Carbidopa/Levodopa: Carbidopa/Levodopa: Formulations Effects Sinemet IR Short half-life (45-90 minutes) Orally disintegrating tablets (dysphagia) The most effective and generally well-tolerated medicine for PD Not sublingually absorbed, similar time to Parcopa peak concentration compared to sinemet IR. Used in setting of dysphagia. Short half-life (~45 to 90 minutes), needs to be taken frequently as PD progresses ~60 minutes increase in sustained Sinemet CR concentration compared to sinemet IR Ideally should be taken 1 hour before or 2 hours after a protein-rich meal Impaired bioavailability, lower peak dose, time to peak concentration can be up to 120 Main side effects: nausea, lightheadedness, hallucinations, and dyskinesias minutes longer than sinemet IR Rytary ~2 to 2.5 hours increase in sustained concentration compared to sinemet IR Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Medications Medications Carbidopa/Levodopa Carbidopa/Levodopa ER: (Rytary) Dosing Guidelines Initial Dosing Guidelines Start with sinemet 25/100mg IR: ½ tab three times per day Increase to sinemet 25/100mg IR: 1 tab three times per day after 2 weeks Increase to sinemet 25/100mg IR: 1.5 tabs three times per day after 2 weeks Increase to sinemet 25/100mg IR: 2 tabs three times per day after 2 weeks Increase the dose until motor symptoms are significantly improved or there are side effects 5
6/22/2018 Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Medications Medications Carbidopa/Levodopa Extenders: Dopamine Agonist: Effects Effects 1 hour increased on-time Rasagaline (Azilect) Compared to carbidopa/levodopa Side effects: drug interactions Lasts longer, half-life: ~6 hours 1 hour increased on-time Lower risk of causing dyskinesias Selegiline (Eldepryl) Side effects: drug interactions, HTN, More mild benefit insomnia, delirium 1 hour increased on-time Entacapone (Comtan) Main side effects: sleep attacks, ICDs, sedation, confusion, hallucinations, Side effects: diarrhea, orange urine cognitive deficits, dry mouth, lightheadedness 2-3 hours increased on-time Tolcapone (Tasmar) Usually not prescribed to people over 70 years of age Side effects: Liver failure Najib 2001, Clinical Therapeutics Jenner, 2002, Neurology Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Medications Medications Levodopa sparing therapy: Levodopa sparing therapy: Effects Effects Mild-moderate reduction in parkinsonism Dopamine agonists Side effects: ICD, sleep attacks, Very mild reduction in parkinsonism, if any MAO-B inhibitors hallucinations, cognitive deficits Side effects: drug interactions, depends on whether rasagaline or selegiline are used Reduces tremor, mild benefit Side effects: nephrolithiasis, somnolence, Zonisamide ataxia, confusion, cognitive deficits Mild reduction in parkinsonism, Reduces tremor and dystonia Amantadine Reduces dyskinesias Trihexyphenidyl Side effects: sedation, delirium, Side effects: confusion, hallucinations, hallucinations, increased risk of dementia, dry mouth, constipation, dry mouth, constipation Najib 2001, Clinical Therapeutics Najib 2001, Clinical Therapeutics 6
6/22/2018 Parkinson’s Disease Motor Symptoms: Risk of Developing Dyskinesias PD Treatments: Anti-dyskinetic medication Amantadine CALM-PD Clinical Trial Dosing Percentage developing Improvement in Only medication that controls tremors, stiffness and slowness, strategy dyskinesia after 2 years movement and function AND also controls dyskinesias scale (UPDRS) Pramipexole 10% 4.5 points Side effects: confusion, hallucinations, rash, dry mouth, constipation Levodopa 30% 9.2 points Could early amantadine prevent the development of dyskinesias? CALM-PD PSG Study Group, 2000, JAMA Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Clinical Trials Non-pharmacological Treatments REHABILITATION OUTPATIENT PHYSICAL THERAPY • Refer to outpatient physical therapy early in the disease course • Parkinson Wellness Recovery (PWR!) • Lee Silverman Voice Training (LSVT) • Balance vest 7
6/22/2018 Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Non-pharmacological Treatments Non-pharmacological Treatments REHABILITATION REHABILITATION HOME SAFETY EVALUATION MEDICARE COVERS ’SKILLED MAINTENANCE’ • • Refer for home safety evaluation: Medicare covers rehab services to maintain or manage a patient’s current condition • skilled nursing when no functional improvement is possible • physical therapy • • occupational therapy Therapy services to maintain a patient’s current condition or slow decline are covered • custodial non-skilled care Parkinson’s Disease Motor Symptoms: Parkinson’s Disease Motor Symptoms: Non-pharmacological Treatments Non-pharmacological Treatments FREEZING OF GAIT FREEZING OF GAIT PHARMACOLOGICAL TREATMENTS NON-PHARMACOLOGICAL TREATMENTS • • May improve with increased levodopa if freezing of gait predominantly occurs May improve with increased levodopa if freezing of gait predominantly occurs Reduce multi-tasking to reduce freezing episodes • in the OFF-MEDICATION state During a freezing episode: come to a complete stop (to abort the malfunctioning automatic gait program causing the freezing episode) • • Medications reported to reduce freezing of gait in select patients: Then try any of the following techniques: • • Rasagiline Try another movement (e.g. raise an arm, touch your head) and then restart walking • • Rotigotine patch Turn in a U-shape • • Amantadine Change direction: step sideways and then go forward • • Droxidopa Weight-shifting from side to side • Methylphenidate • Step over a target (e.g. a laser pointer using U-step walker/cane) • Metronome or musical cueing • Stress-reduction techniques to minimize emotional triggers of freezing episodes • Body awareness techniques to reduce anxiety (e.g. Alexander Technique) 8
Recommend
More recommend