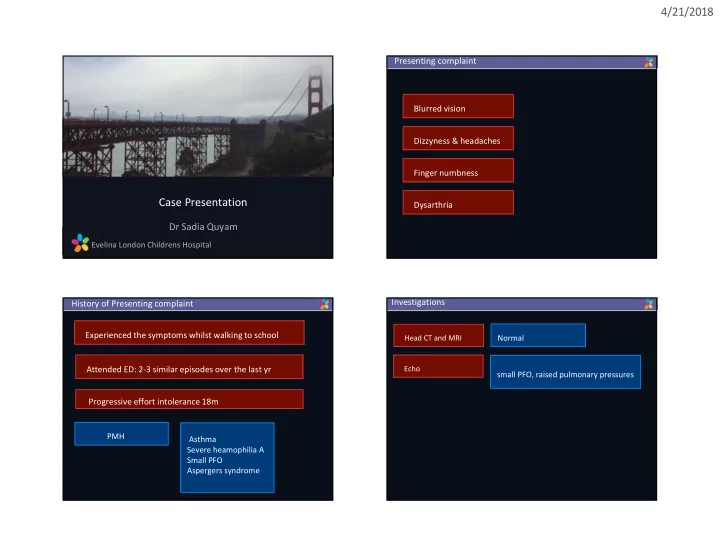
4/21/2018 Presenting complaint Blurred vision Dizzyness & headaches Finger numbness Case Presentation Dysarthria Dr Sadia Quyam Evelina London Childrens Hospital Investigations History of Presenting complaint Experienced the symptoms whilst walking to school Head CT and MRI Normal Attended ED: 2-3 similar episodes over the last yr Echo small PFO, raised pulmonary pressures Progressive effort intolerance 18m PMH Asthma Severe heamophilia A Small PFO Aspergers syndrome 1
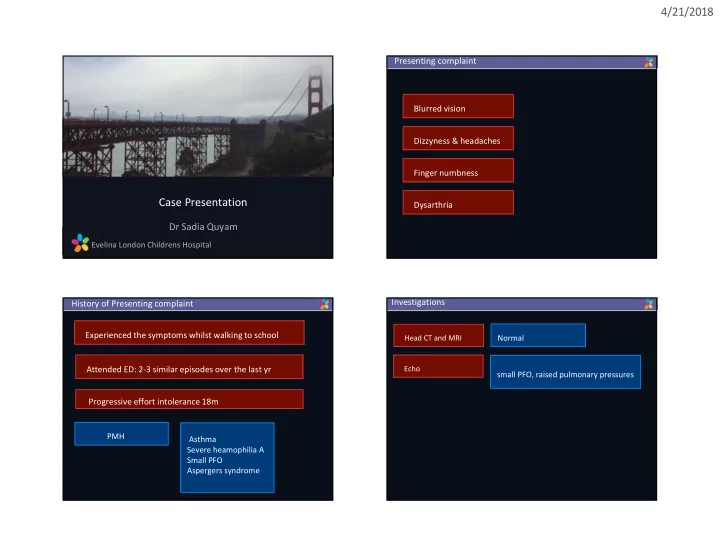
4/21/2018 Investigations Investigations Hb 141 g/dl. VO2 assumed 146mls/min/m2. FiO2 0.21, TPG 45mmHg Qpi 3.8 L/min/m2 PVRI 11.8 WU.m2 FiO2 1.0 TPG 44mmHg Qpi 3.8 L/min/m2 PVRI 13.3 WU.m2 FiO2 1.0 + iNO 20ppm TPG 43mmHg Qpi 3.4 L/min/m2 PVRI 12.6WU.m2 Summary MRI angio 11 year old boy with severe haemophilia A treated with recombinant factor VIII via porto-cath. Well controlled with only one bleeding complication in history. Progressive effort limitation for 18 months (WHO III) Presented acutely with neurological symptoms consistent with TIA, haemorrhage excluded on neuro-imaging. During the acute assessment he was found to have a murmur and subsequent echo showed evidence of severe PH, confirmed on catheterisation. Further work up included a CT which was reported locally and did not Repeat Echo showed central venous catheter deep in the RA reveal a cause for his PH - referred to National PH service prolapsing through the TCV 2
4/21/2018 Review MRI angio CT initially reported as normally twice but on further and in the context f the history felt to be abnormal Relative paucity of the vasculature noted in the RLL. The regional variation in calibre signifies thromboembolic disease, es Conclusion: Severe pulmonary hypertension, no features of PVOD Concern that CTEPH is a cause. The PFO may explain the cerebral events. Review MRI angio Although felt to be operable, significant challenge and risk of doing so in a child with heamophillia 3
4/21/2018 PEA Cath 4
Recommend
More recommend