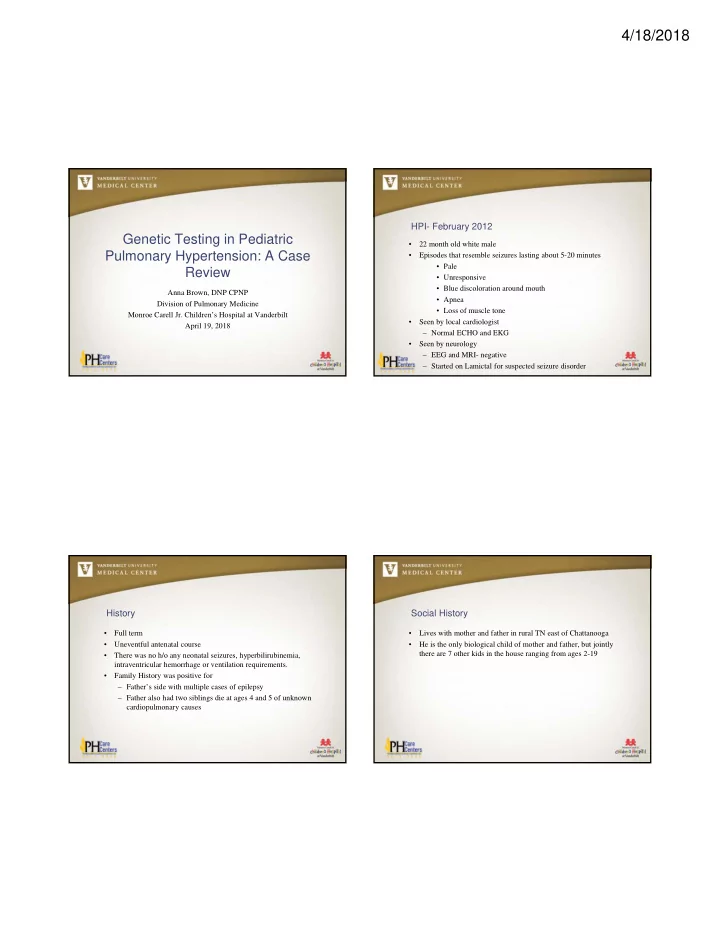
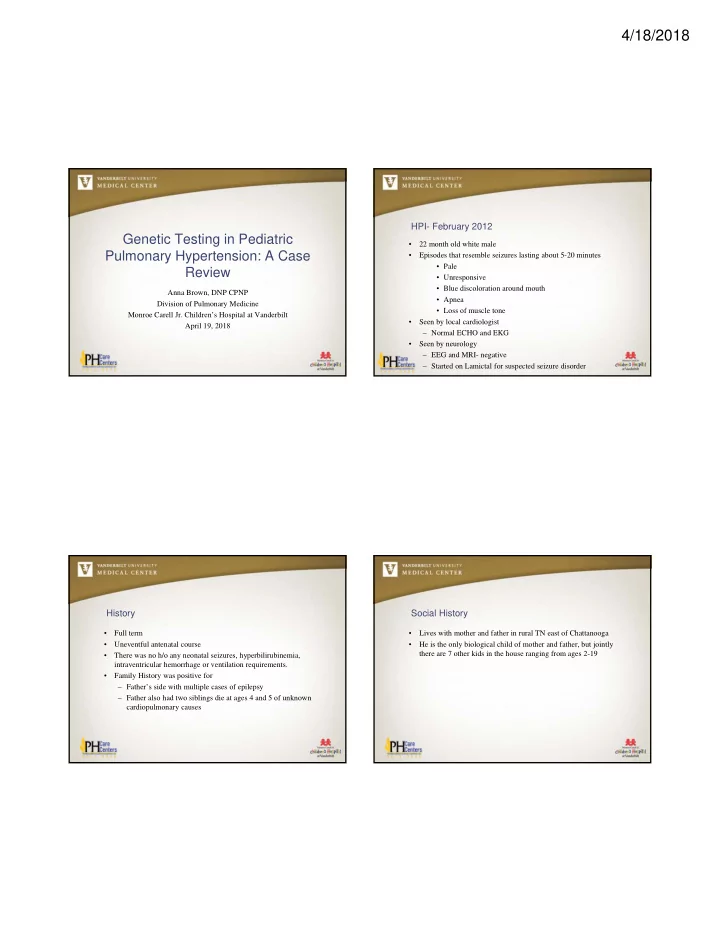
4/18/2018 HPI- February 2012 Genetic Testing in Pediatric • 22 month old white male Pulmonary Hypertension: A Case • Episodes that resemble seizures lasting about 5-20 minutes • Pale Review • Unresponsive • Blue discoloration around mouth Anna Brown, DNP CPNP • Apnea Division of Pulmonary Medicine • Loss of muscle tone Monroe Carell Jr. Children’s Hospital at Vanderbilt • Seen by local cardiologist April 19, 2018 – Normal ECHO and EKG • Seen by neurology – EEG and MRI- negative – Started on Lamictal for suspected seizure disorder History Social History • Full term • Lives with mother and father in rural TN east of Chattanooga • Uneventful antenatal course • He is the only biological child of mother and father, but jointly there are 7 other kids in the house ranging from ages 2-19 • There was no h/o any neonatal seizures, hyperbilirubinemia, intraventricular hemorrhage or ventilation requirements. • Family History was positive for – Father’s side with multiple cases of epilepsy – Father also had two siblings die at ages 4 and 5 of unknown cardiopulmonary causes
4/18/2018 HPI- May 2013 (note- 15 months later) Right Heart Catheterization (RHC) • June 7, 2013 Erlanger Children’s Hospital performed a RHC due to • Continued episodes, becoming more frequent concern for pulmonary hypertension in the setting of syncope and • Followed by Erlanger Children’s Hospital Cardiology every 6-12 cardiomegaly months Systemic Pressure PA Pressure – Repeat ECHO showed RVH, normal structure, normal function Baseline 73/37 (51) 73/34 (53) – CBC normal 100% FiO2 75/38 (52) 68/29 (48) – Chest CT showed enlarged main PA and vascular congestion 100% FiO2 + 40 82/41 (58) 73/31 (62) ppm NO • Diagnoses confirmed on RHC and he was referred to Vanderbilt Children’s Hospital Pediatric Pulmonary Group for management of PH Consult with Pediatric Pulmonary Hypertension Consult with Pediatric Pulmonary Hypertension Team at VCH Team at VCH • June 14, 2013 • Confirmed the diagnosis of Pulmonary Hypertension, likely iPAH, but needed further investigation. • Reviewed clinical course and RHC • Due to location of family, concerned he might be heritable PH • Repeated ECHO • Ordered sleep study- normal Nashville • Started on ERA therapy- Ambrisentan • Added MVI with iron • Discussed activity restriction Grundy County- home of “Family 14” Largest known family with HPAH
4/18/2018 Gender disparity Reduced Penetrance: Vanderbilt and 2-3 Females : 1 male 27% carriers get PAH Females: 42% Familial PAH Males: 14% Larkin AJRCCM 2012 The Initial Loyd/Newman Family: 39 Confirmed PAH (Loyd, Primm, & Newman, 1984) (Updated Dec 2011 ( Pulm Circ )—initial pub by Loyd, Primm, Newman , 1984) BMPR2 mutations in PAH Type of PAH Reported mutation Nashville prevalence Familial PAH > 75% Idiopathic PAH 20% Congenital heart disease 6% Scleroderma Not detected HIV Not detected Hemolytic disease Not reported Hometown of DW Grundy County • Population prevalence: unknown but very rare
4/18/2018 Ordering Genetic Testing in PH References • www.concertgenetics.com Ivy, D. D., Abman, S. H., Barst, R. J., Berger, R. M., Bonnet, D., Fleming, T. R… & Beghetti, M. (2013). Pediatric pulmonary hypertension. Journal of the American College of Cardiology, 62 (25). doi: doi:10.1016/j.jacc.2013.10.028 Loyd, Primm, & Newman. (1984). Am Rev Respir Disease, 129 (1):194-7. Humbert, M., Sitbon, O., & Simonneau, G. (2004). Treatment of pulmonary arterial hypertension. New England Journal of Medicine, 351. doi: 10.1056/NEJMra040291 Zaiman, A., Fijalkowska, I., Hassoun, P. M., & Tuder, R. M. (2005). One hundred years of research in the pathogenesis of pulmonary hypertension. American Journal of Respiratory Cell Molecular Biology, 33 (5). 425-31.
Recommend
More recommend