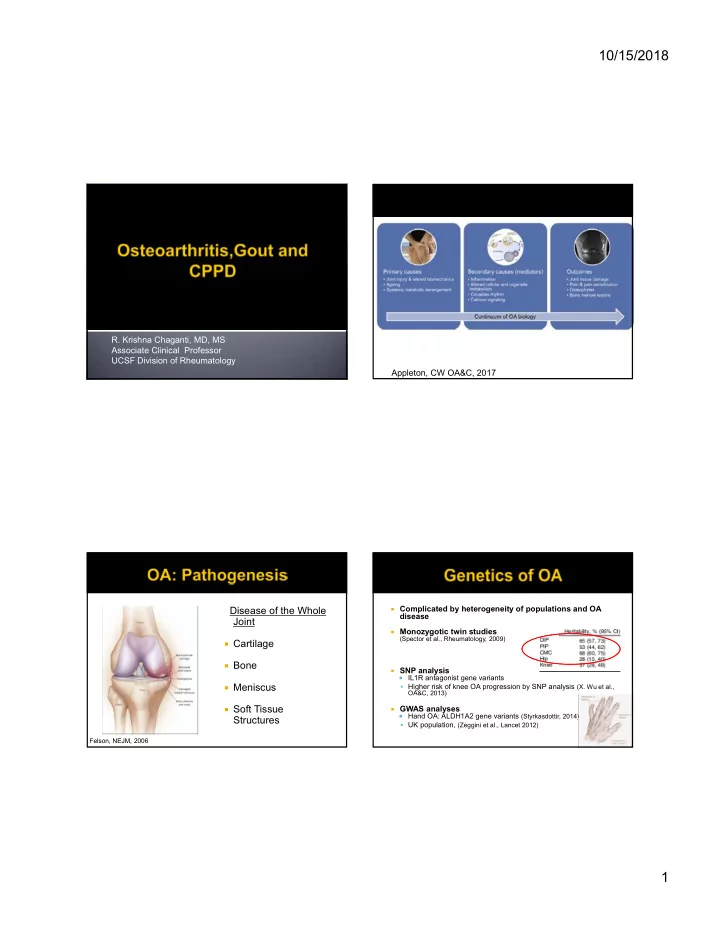
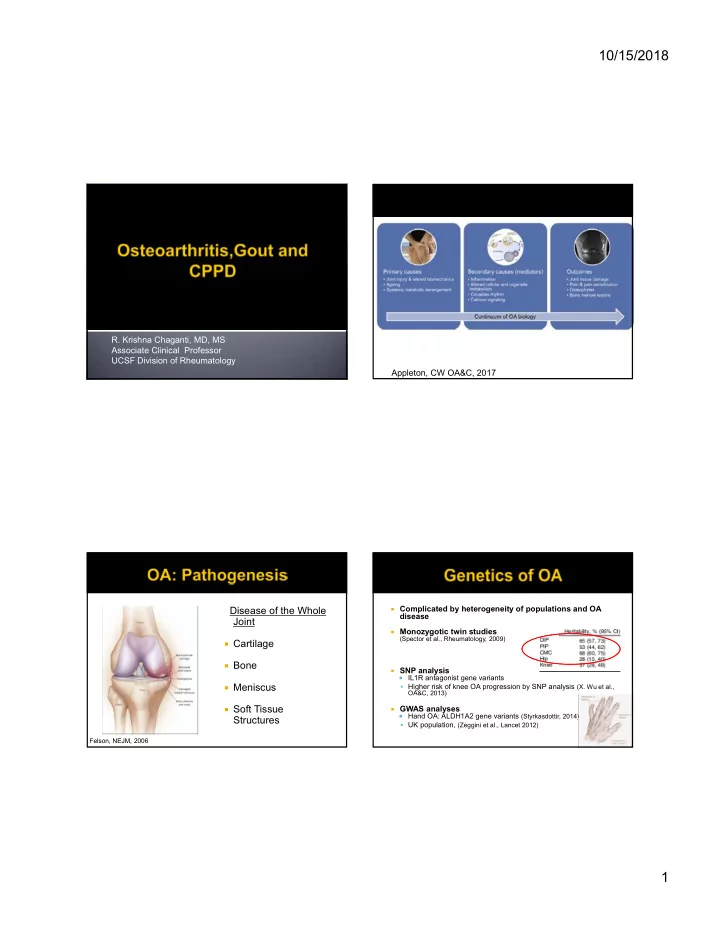
10/15/2018 R. Krishna Chaganti, MD, MS Associate Clinical Professor UCSF Division of Rheumatology Appleton, CW OA&C, 2017 Complicated by heterogeneity of populations and OA Disease of the Whole disease Joint Monozygotic twin studies (Spector et al., Rheumatology, 2009) Cartilage Bone SNP analysis IL1R antagonist gene variants Meniscus Higher risk of knee OA progression by SNP analysis (X. Wu et al., OA&C, 2013) Soft Tissue GWAS analyses Hand OA: ALDH1A2 gene variants (Styrkasdottir, 2014) Structures UK population, (Zeggini et al., Lancet 2012) Felson, NEJM, 2006 1
10/15/2018 Residents of 4 districts of Beijing > 60 years old, randomly recruited from general public Lower prevalence of radiographic hip OA in subjects living in Beijing with age-matched controls (SOF, NHANEs). Higher prevalence of knee OA in older Chinese women than in Framingham cohort (genetics, physical activity?) Lower prevalence of hand OA (CMC, MCP and PIP, DIP) compared to Caucasians (Framingham study) Higher incidence in thumb IP and 2 nd and 3 rd PIP (OR 1.4-1.5) Pattern of OA Osteophytes JSN OA in unusual joints Subchondral Elbow, Glenohumeral joint, MCPs sclerosis Subchondral cysts Joint Structural Defects Joint deformity Congenital or Acquired Standing knee Hereditary Connective Tissue Defects Sunrise views Some with defined gene mutations Metabolic Diseases 2
10/15/2018 • Legg-Calve-Perthes, congenital hip • Trauma dislocation, SCFE • Distant • Surgical (Menisectomy) • Femoroacetabular • Secondary to impingement inflammatory disease (RA) • Hypermobility syndrome • Leg-length discrepancy • Thoracic scoliosis • Knee DJD Avascular necrosis 56 year old woman with hand pain Neuropathic Noticed “bumps” on her fingers for several (Charcot ’ s joint) years Syrinx (glenohumeral) Increased pain and swelling over DIP joints over past year Metabolic: CPPD, Ochronosis, Hemochromatosis, Improved with ibuprofen Wilson’s, Gaucher’s 3
10/15/2018 What is her diagnosis? A) Osteoarthritis B) Psoriatic Arthritis C) Erosive Osteoarthritis (Banks, SE, Clin Rheumatology; 2010) Erosive OA Psoriatic Arthritis Central Erosions Yes Sometimes “ Fluffy ” Periosteal No Yes Bone formation Synovitis Usually Yes Heberden ’ s Yes (not specific) No Nodes Periarticular No Yes erosions AM stiffness, Sometimes Yes nighttime waking Ankylosis Yes Yes PIP involvement Yes Yes (Banks, SE, Clin Rheumatology; 2010) DIP, PIP involvement, central erosive changes 4
10/15/2018 T DON’T RECOMMEND RECOMMEND Topical capsaicin Intraarticular therapies Topical NSAIDs Opioid Analgesics Oral NSAIDs Tramadol Conditional DIP CMC PIP ! Splints >75 years old -Increases with age, especially postmenopausal women Topical NSAIDs -Women > Men -Heberden ’ s and Bouchard ’ s nodes genetic predisposition more than oral Exercise • ACR and OARSI guideline recommendations Weight Loss • Mainstay: Combination of pharmacologic and non-pharmacologic therapy Walking Tai Chi Accupuncture Hochberg MC, et al., Arthritis Care Res 2012 5
10/15/2018 Corrective Devices Recommendations are similar for Shift the weight-bearing hip osteoarthritis axis towards the center of except no role for the affected varus knee topical agents in hip towards Neutral alignment OA Directly Unload Medial ! Knee Use Acetaminophen first Unloader Braces Duloxetine is a last option Lateral Wedges Hochberg MC, et al. Canes (Contralateral side) Arthritis Care Res 2012, Flexible Shoes PMID 22563589 www.rheumatology.org ‐ May be of benefit Boswellia Most studies Turmeric ‐ Risk is unclear Cat’s claw indicate no Avocado-soybean unsaponifiables (ASU) significant benefit No known diet that halts OA in: Resources: Pain Osher Centers for Integrative Medicine Function NIH National Center for Complementary and Integrative Health Joint Structure Memorial Sloan Kettering herbal references: GAIT Study (Clegg DO et al., NEJM, https://www.mskcc.org/cancer-care/diagnosis- 2006) treatment/symptom-management/integrative-medicine/herbs 6
10/15/2018 Cochrane Meta- analysis Less pain at 1-4 weeks Effect decreases over time No effect after 6 mo. Adverse effects do Self reported pain assessed not seem to be a by Knee Injury and problem • Significant cartilage thickness change in IA Triamcinolone group v. Saline Clinical significance? Peter J, et al. Cochrane Database Syst Rev Henricken M, et al. JAMA Intern Med 2015, 2015. PMID 26490760 PMID 25822572 MacAlindon et al., JAMA, 2017 Viscosupplementation with hyaluronic PRPP (TGF-beta, PDF-GF,VEGF) acid (HA) - a natural constituent of joint fluid - to restore the viscoelasticity of Bone Marrow Matrix synovial fluid Adipose MSC Debatable efficacy based on data Autologous BM Aspirate Chevalier et al., Ann Rheum Dis 2010 Allogeneic MSCs Umbilical cord derived MSCs Meta-analyses also conflicting: 76 trials of Intra-articular injections of HA (IA-HA) for knee OA (Campbell et al, Wide variation in methodology, no large standardized OA &C, 2007) clinical trial data to support use at this time More standardized methodology and outcome Slow acting – benefits appreciated measures needed at 5-13 weeks post injection Few adverse events reported: acute Strong Marketing Drives the Use reaction of inflammation and synovitis Bellamy N, et al. Cochrane Database Syst Rev, 2006 7
10/15/2018 65 yo Korean man with DM and stage 4 CKD presents with 2 days of left foot pain and swelling Pain is severe and he is unable to ambulate No antecedent trauma Labs: WBC 12K, Cr 3.7, BG 200, uric acid 9 Synovial fluid: WBC 50,000 (90% PMNs), gram stain negative 8
10/15/2018 What treatment do you recommend? What dose of prednisone do you start? How long do you treat for? A. Naproxen 500 mg PO BID Do you need to taper? B. Colchicine 1.2 mg PO, followed by 0.6 mg every hour x 3 C. Prednisone 40 mg PO daily D. Intra-articular injection of triamcinolone 40 mg into left ankle E. I really don’t like any of these options Your patient is treated with 40 mg of Are there other options for treatment of prednisone tapered by 10 mg every 2-3 acute gout? days with complete relief of his symptoms 100 mg SQ daily x 36 3 days 9
10/15/2018 He returns to your office for follow up. His flare has resolved. His serum uric acid is 10. He wants to know what the likelihood of having another flare is. JRheum Mar 2017, 44 (3) 3 37 38 Associated with increased risk for allopurinol What do you do now? hypersensitivity reaction A. Start allopurinol 300 mg PO daily Risk is 0.1-0.4% in general population OR in one Thai series 348.33 (95% CI 19.15 – 6336.88) B. Start febuxostat 80 mg PO daily Allopurinol is contraindicated in patients who are C. Start allopurinol 50 mg PO daily carriers for this allele D. Obtain further lab testing Most commonly found in patients of Korean, Han Chinese, or Thai descent (6-12%) ACR recommends genetic testing prior to allopurinol use in Korean patients with stage 3 CKD or worse, and all patients of Han Chinese or Thai descent 10
10/15/2018 Because patient is Korean and has stage 4 Increased risk of allopurinol CKD, you check for HLAB*5801, which hypersensitivity reaction returns negative Starting dose of 50 mg/d in patients with You start allopurinol 50 mg/d and colchicine CKD stage 4 or worse 0.6 mg QOD Can uptitrate as needed to achieve uric Labs 2 weeks later: CBC and LFTs are normal, uric acid 8 acid goal Continue to slowly titrate allopurinol over 3 Allopurinol is not nephrotoxic! months to 300 mg/d Febuxostat is now generic Uric acid is 6.4 What do you do now? A. Continue allopurinol 300 mg/d B. Increase allopurinol to 400 mg/d C. Switch patient to febuxostat 40 mg/d D. Stop colchicine 11
10/15/2018 Goal uric acid is <= 6 mg/dl If tophaceous or erosive disease, goal is <= 5 mg/dl ACP Gout CPG 2017: “Evidence was insufficient to conclude whether the benefits of escalating urate-lowering therapy to reach a serum urate target (“treat to target”) outweigh the harms associated with repeated monitoring and medication escalation.” Your patient asks you if there any non- What do you recommend? medical therapies he can try to lower his A. Taking cherry extract uric acid level. B. Decreasing his food intake and increasing his physical activity to lose weight C. Increasing his intake of low-fat dairy products D. Stop drinking sugar-sweetened drinks 12
Recommend
More recommend