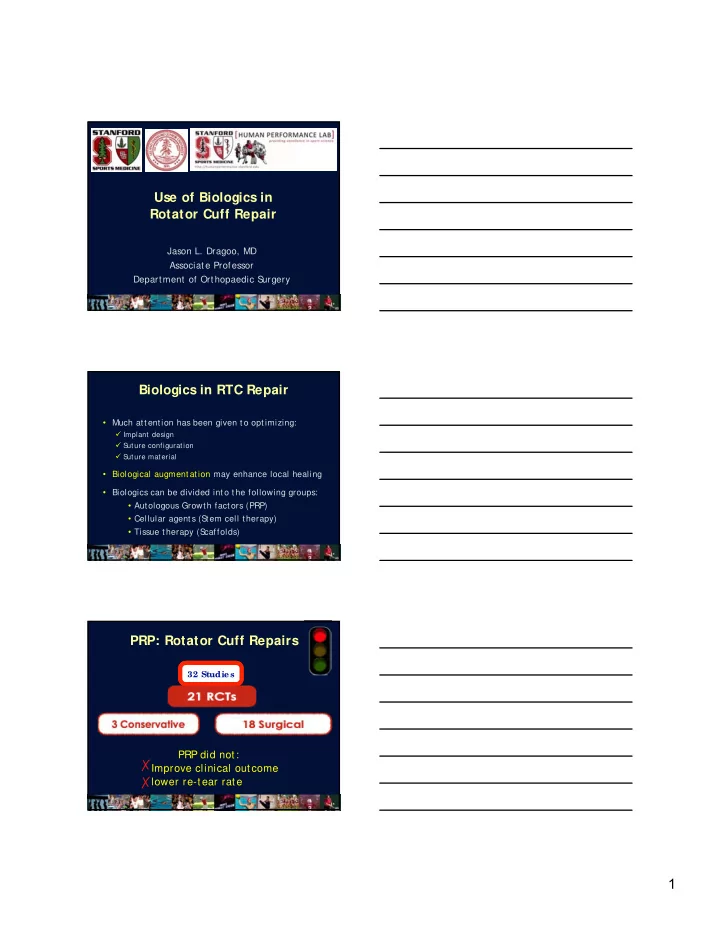
Use of Biologics in Rotator Cuff Repair Jason L. Dragoo, MD Associate Professor Department of Orthopaedic S urgery Biologics in RTC Repair • Much attention has been given to optimizing: Implant design S uture configuration S uture material • Biological augmentation may enhance local healing • Biologics can be divided into the following groups: • Autologous Growth factors (PRP) • Cellular agents (S tem cell therapy) • Tissue therapy (S caffolds) PRP: Rotator Cuff Repairs 32 Studie s PRP did not: ✗ Improve clinical outcome ✗ lower re-tear rate 1
Arthroscopy Dec 2015 • Included all Meta-analyses before 2015 • 7 meta-analyses with 3,193 patients • S ubgroup analysis: some evidence of outcomes: • S maller and medium-sized tears • Double-row fixation techniques • PRP clot inj ected at bone-tendon interface Fundamental Question? • Are cells necessary to improve RTC healing? • Why? • Atrophic cuff tendon • Displaced local MS Cs • Direct repair process Insertion Site Preparation • Methods to improve local environment Bed abrasion Crimson Vail Microfracture • Think Biology! 2
• Patients with tear had lower levels of MS Cs • Patients with local bone marrow edema MS Cs 214 ± 128 Tear= No tear= 564 ± 216 Marrow Stimulation MS 78% Control 55% MS > Control MS > Control Taniguchi et al, JSES 2 0 1 3 S lide Courtesy of Brian Cole Stem Cell Therapy • Only 3 clinical studies have been published • Mesenchymal stem cell (MS Cs) therapy may improve healing by: • S ecreting growth factors • Providing cellularity • Local paracrine activity 3
RTC Repair: S tem Cells • 45 patients BMAC + RCR • 45 matched control RCR • 10 year follow-up • MS Cs drawn from AS IS and placed at tendon interface • 87% healing (BM-MS C) vs. 44 % (Non BM-MS C) • Control group 4x as likely to have “ poor outcome” Where should stem cells be harvested? Proximal Humerus Iliac Crest • 125 patients with tear 75 w/ o cuff tear MS Cs • Marrow aspirated from 214 ± 128 Tear= greater tuberosity No tear= 564 ± 216 • Patients with tear had significantly lower levels of MS Cs 4
Stem Cell Summary • Clinical evidence to support the use of cells to augment RTC repair is promising • More RCTs will be necessary to verify Hernigou’ s findings RTC Scaffolds RTC Scaffolds • Difficult to evaluate • Many types Allograft Xenograft (Bovine) S ynthetic Many uses… 5
RTC Scaffold Uses Augment repair Interposition • • Improve mechanics Lengthen tendon • • Improve biology S uperior capsular reconstruction Scaffold Augmentation Level of Evidence II N=42, Human Allograft 85% * (augmentation) vs 40% repair N=30, Xenograft 27% (augmentation) vs 60% repair Erythema and/ or drainage seen in 3 of 15 cases of augmentation *statistically significant Scaffold Interposition Level of Evidence III N=68 58% * Interposition vs 26% tensioned repair N=48 Re-tear rate: 8% * Interposition vs 42% tensioned repair *statistically significant 6
Scaffolds Summary • May be useful in clinically tough scenarios • Routine use may be questioned due to Cost Lack of consistent literature Unclear biologic benefit Summary • Give biology the same attention as you give implant and repair techniques • Think about the local biological environment and optimize it when possible • This may lead to improved healing rates and clinical outcomes 7
Recommend
More recommend