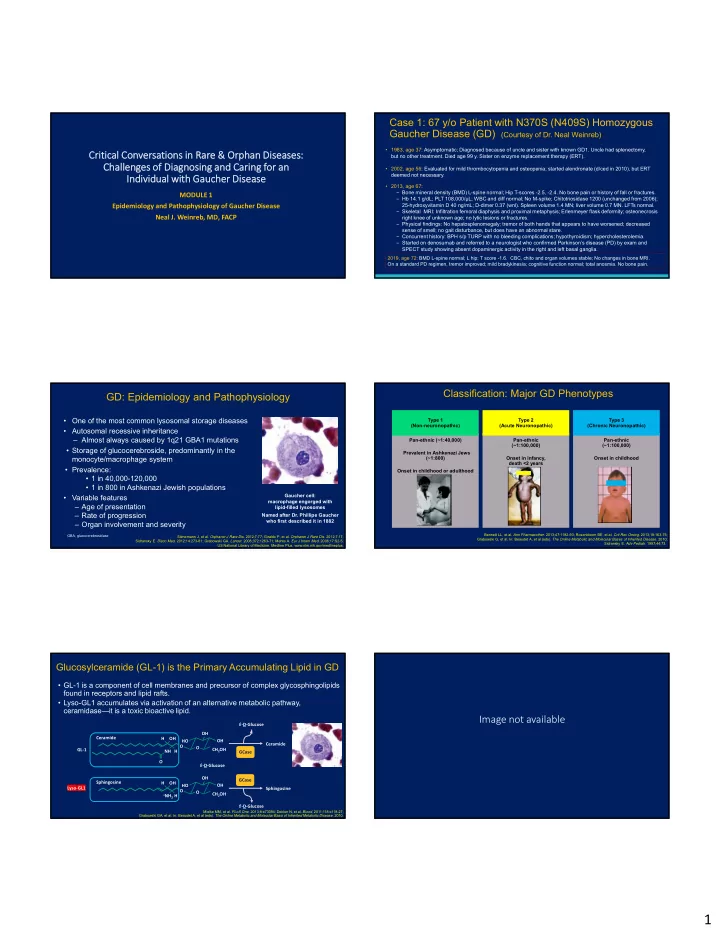
Case 1: 67 y/o Patient with N370S (N409S) Homozygous Gaucher Disease (GD) (Courtesy of Dr. Neal Weinreb) • 1983, age 37: Asymptomatic; Diagnosed because of uncle and sister with known GD1. Uncle had splenectomy, Critical Conversations in Rare & Orphan Diseases: but no other treatment. Died age 99 y. Sister on enzyme replacement therapy (ERT). Challenges of Diagnosing and Caring for an • 2002, age 56: Evaluated for mild thrombocytopenia and osteopenia; started alendronate (d/ced in 2010), but ERT deemed not necessary. Individual with Gaucher Disease • 2013, age 67: – Bone mineral density (BMD) L-spine normal; Hip T-scores -2.5, -2.4. No bone pain or history of fall or fractures. MODULE 1 – Hb 14.1 g/dL; PLT 108,000/µL; WBC and diff normal; No M-spike; Chitotriosidase 1200 (unchanged from 2006); 25-hydroxyvitamin D 40 ng/mL; D-dimer 0.37 (wnl). Spleen volume 1.4 MN; liver volume 0.7 MN. LFTs normal. Epidemiology and Pathophysiology of Gaucher Disease – Skeletal MRI: Infiltration femoral diaphysis and proximal metaphysis; Erlenmeyer flask deformity; osteonecrosis Neal J. Weinreb, MD, FACP right knee of unknown age; no lytic lesions or fractures. – Physical findings: No hepatosplenomegaly; tremor of both hands that appears to have worsened; decreased sense of smell; no gait disturbance, but does have an abnormal stare. – Concurrent history: BPH s/p TURP with no bleeding complications; hypothyroidism; hypercholesterolemia. – Started on denosumab and referred to a neurologist who confirmed Parkinson’s disease (PD) by exam and SPECT study showing absent dopaminergic activity in the right and left basal ganglia. 2019, age 72: BMD L-spine normal; L hip: T score -1.6. CBC, chito and organ volumes stable; No changes in bone MRI. On a standard PD regimen, tremor improved; mild bradykinesia; cognitive function normal; total anosmia. No bone pain. Classification: Major GD Phenotypes GD: Epidemiology and Pathophysiology • One of the most common lysosomal storage diseases Type 1 Type 2 Type 3 (Non-neuronopathic) (Acute Neuronopathic) (Chronic Neuronopathic) • Autosomal recessive inheritance – Almost always caused by 1q21 GBA1 mutations Pan-ethnic (~1:40,000) Pan-ethnic Pan-ethnic (~1:100,000) (~1:100,000) • Storage of glucocerebroside, predominantly in the Prevalent in Ashkenazi Jews monocyte/macrophage system (~1:800) Onset in infancy, Onset in childhood death <2 years • Prevalence: Onset in childhood or adulthood • 1 in 40,000-120,000 • 1 in 800 in Ashkenazi Jewish populations Gaucher cell: • Variable features macrophage engorged with – Age of presentation lipid-filled lysosomes – Rate of progression Named after Dr. Phillipe Gaucher who first described it in 1882 – Organ involvement and severity Bennett LL, et al. Ann Pharmacother . 2013;47:1182-93; Rosenbloom BE, et al. Crit Rev Oncog . 2013;18:163-75; GBA, glucocerebrosidase Stirnemann J, et al. Orphanet J Rare Dis . 2012;7:77; Giraldo P, et al. Orphanet J Rare Dis . 2012;7:17; Grabowski G, et al. In: Beaudet A, et al (eds). The Online Metabolic and Molecular Bases of Inherited Disease . 2010; Sidransky E. Disco Med. 2012;14:273-81; Grabowski GA. Lancet . 2008;372:1263-71; Mehta A. Eur J Intern Med. 2006;17:S2-5; Sidransky E. Adv Pediatr . 1997;44:73. US National Library of Medicine. Medline Plus. www.nlm.nih.gov/medlineplus. Glucosylceramide (GL-1) is the Primary Accumulating Lipid in GD • GL-1 is a component of cell membranes and precursor of complex glycosphingolipids found in receptors and lipid rafts. • Lyso-GL1 accumulates via activation of an alternative metabolic pathway, ceramidase—it is a toxic bioactive lipid. Image not available β ‐D‐Glucose OH Ceramide H OH HO OH Ceramide O O GL‐1 CH 2 OH NH H GCase O β ‐D‐Glucose OH GCase Sphingosine H OH HO OH Lyso‐GL1 Sphingosine O O CH 2 OH + NH 2 H β ‐D‐Glucose Mielke MM, et al. PLoS One . 2013;8:e73094; Dekker N, et al. Blood . 2011;118:e118-27; Grabowski GA, et al. In: Beaudet A, et al (eds). The Online Metabolic and Molecular Basis of Inherited Metabolic Disease . 2010. 1
Lifetime Probability of Cancer by Attained Age in Overall Cancer Risk Increased in GD Gaucher Patients (RR, 1.80; 95% CI, 1.32-2.40) N=2742 Observed Expected RR (95% CI) Prevalence of Gammopathy by Age All cancer* 126 159 0.79 (0.67, 0.94) in 402 Patients With Enzymatically and Genomically Confirmed GD Multiple myeloma 10 1.7 5.9 (2.82, 10.82) 100 • 33-fold increased risk of 90 Breast cancer 15 33.2 0.45 (0.25, 0.75) Percent MM / MGUS / 80 gammopathy in GD type 1 PG-Free Survival 70 Prostate cancer 10 30.4 0.33 (0.16, 0.60) 60 Colorectal cancer 6 15.5 0.39 (0.14, 0.84) 50 MM 40 MGUS Lung cancer 6 19.9 0.30 (0.11, 0.66) PG 30 20 Blood 19 15.6 1.23 (0.73, 1.90) PG, n = 132; MGUS, n = 17; MM, 10 n = 9 0 *Includes non-melanoma skin cancers, ovarian cancer, renal carcinoma, 0 10 20 30 40 50 60 70 80 90 Age, years bladder cancer, hepatocellular cancer, ganglioneuroma, neurosarcoma, • Both homozygous N370S and heterozygous N370S mutation had: angiosarcoma, thyroid carcinoma pancreatic cancer, testicular – An increased lifetime risk of multiple myeloma (RR, 25; 95% CI, 9.17-54.40) rhabdomyosarcoma, carcinoid tumor – An increased risk of hematologic malignancies (RR, 3.45; 95% CI, 1.49-6.79 ) Rosenbloom BE, et al. Blood . 2005;105:4569-72. Taddei TH, et al. Amer J Hematol. 2009;84:208-14. Gba1 Mutations (Gaucher Carrier or Patient) Accumulating GL-1 and Lyso-GL1 Trigger Lipid-Specific A significant risk factor for Parkinson’s disease (PD) Immune Response and Chronic Inflammation Hypergammaglobulinemia Anti‐Lipid Antibodies IFN‐ , IL‐22, IL‐17, IL‐2, IL‐21 type II NKT cell Mononuclear Phagocyte/ Antigen- Presenting B cell Cell B‐Cell Proliferation MIP1β, IL‐6, IL‐8 Germinal Center Reaction BCR Lysosomal lipid storage TCR CD1g‐βGL1 or CD1d‐LGL1 complexes Gaucher patients (homozygotes) apparently have an even greater risk for development of PD, but studies of Gaucher patient populations are at an earlier stage. Salio M, et al. Blood . 2015;125:1200-2; Nair S, et al. Blood . 2015;135:1256-71. GL-1 Accumulation Leads to Cellular Dysfunction Points to Remember • Normally, GCase interacts with GL-1 as well as monomers of α-synuclein in lysosomes, facilitating • GD is one of the most common lysosomal storage diseases world-wide and is the breakdown of both at acidic pH. particularly prevalent in Jews whose family origins are traced to northern, eastern and central Europe (Ashkenazim). • Mutated or decreased levels of GCase result in a slowdown of α-synuclein degradation, a gradual build up of GL-1 and formation of α-synuclein oligomers and fibrils. • GD is classified as being either neuronopathic (types 2 and 3) or non- neuronopathic (type 1), but all types can present with severe symptoms early • GL-1 stabilizes the α-synuclein oligomers. These oligomers bind to mutated GCase and further in life. inhibit the enzymatic activity of GCase. • GD is caused by trans-biallelic mutations in the GBA1 gene leading to deficient lysosomal glucocerebrosidase deficiency with storage of glucosylceramide • The GL-1 engorged lysosomes have impaired chaperone-mediated autophagy and (GL-1) and increases in glucosylsphingosine (lyso-GL1). autophagosome fusion. • Accumulating GL-1 and lyso-GL1 trigger lipid-specific immune responses and • This causes increased accumulation of α-synuclein insoluble aggregates in the cytoplasm (Lewy chronic inflammation that can lead to concurrent malignancies such as bodies). These aggregates block trafficking of GCase from the endoplasmic reticulum (ER) to the MGUS/myeloma, lymphoma and hepatocellular carcinoma. Golgi. Mutant GCase is retained in the ER evoking the ER unfolded protein stress response). MGUS, monoclonal gammopathy of unknown significance Stirnemann J, et al. Int J Mol Sci . 2017;18(2). pii: E441. 2
Points to Remember (continued) • GL-1 accumulation in lysosomes and the presence of mutant glucocerebrosidase also promote synuclein oligomer aggregation and neuronal death. • Consequently, despite the label “non-neuronpathic,” patients with GD1 and carrier relatives have an increased risk for Parkinsonism and related synucleopathies. • Both malignancies and Parkinsonism may occur as late manifestations even when patients ostensibly have clinically mild GD phenotypes. 3
Recommend
More recommend