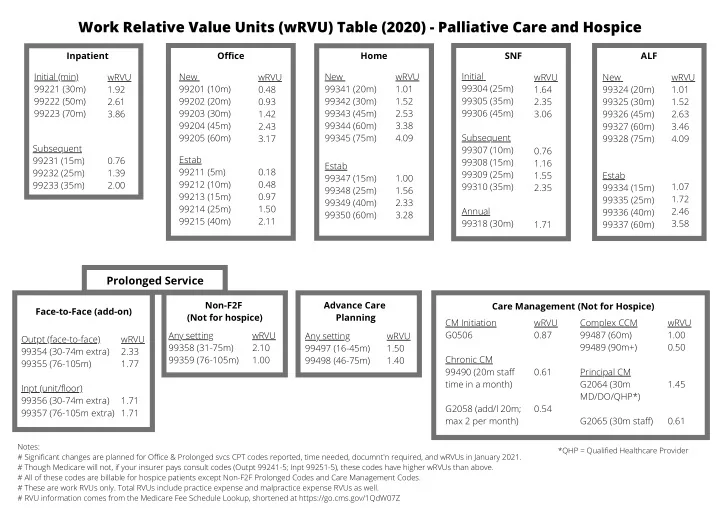
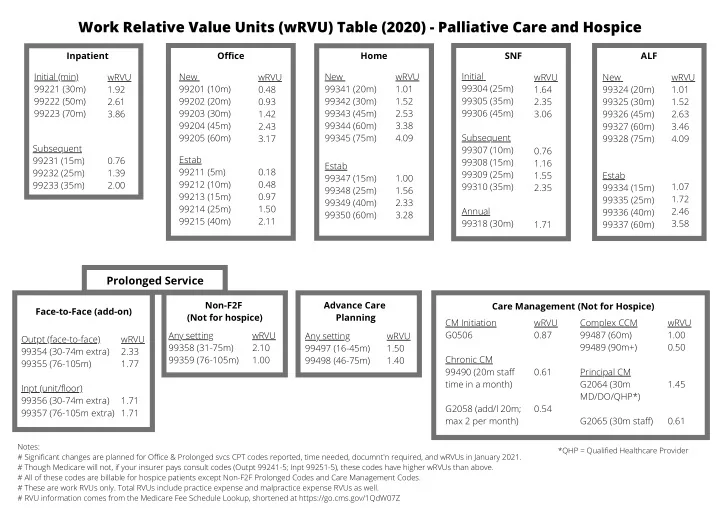
Work Relative Value Units (wRVU) Table (2020) - Palliative Care and Hospice Inpatient Office Home SNF ALF Initial Initial (min) wRVU New wRVU New wRVU wRVU New wRVU 99221 (30m) 99201 (10m) 99341 (20m) 1.01 99304 (25m) 1.92 0.48 1.64 99324 (20m) 1.01 99305 (35m) 99222 (50m) 2.61 99202 (20m) 0.93 99342 (30m) 1.52 2.35 99325 (30m) 1.52 99223 (70m) 99203 (30m) 99343 (45m) 2.53 99306 (45m) 3.86 1.42 3.06 99326 (45m) 2.63 99204 (45m) 2.43 99344 (60m) 3.38 99327 (60m) 3.46 99205 (60m) 99345 (75m) 4.09 Subsequent 3.17 99328 (75m) 4.09 Subsequent 99307 (10m) 0.76 Estab 99231 (15m) 0.76 99308 (15m) 1.16 Estab 99211 (5m) 0.18 99232 (25m) 1.39 99309 (25m) 1.55 Estab 99347 (15m) 1.00 99212 (10m) 0.48 99233 (35m) 2.00 99310 (35m) 1.07 2.35 99334 (15m) 99348 (25m) 1.56 99213 (15m) 0.97 1.72 99335 (25m) 99349 (40m) 2.33 99214 (25m) 1.50 Annual 2.46 99336 (40m) 99350 (60m) 3.28 99215 (40m) 2.11 99318 (30m) 3.58 1.71 99337 (60m) Prolonged Service Non-F2F Advance Care Care Management (Not for Hospice) Face-to-Face (add-on) (Not for hospice) Planning CM Initiation wRVU Complex CCM wRVU Any setting wRVU G0506 0.87 99487 (60m) 1.00 Any setting wRVU Outpt (face-to-face) wRVU 99489 (90m+) 0.50 99358 (31-75m) 2.10 99497 (16-45m) 1.50 99354 (30-74m extra) 2.33 99359 (76-105m) 1.00 Chronic CM 99498 (46-75m) 1.40 99355 (76-105m) 1.77 99490 (20m staff 0.61 Principal CM time in a month) G2064 (30m 1.45 Inpt (unit/floor) MD/DO/QHP*) 99356 (30-74m extra) 1.71 G2058 (add/l 20m; 0.54 99357 (76-105m extra) 1.71 max 2 per month) G2065 (30m staff) 0.61 Notes: *QHP = Qualified Healthcare Provider # Significant changes are planned for Office & Prolonged svcs CPT codes reported, time needed, documnt'n required, and wRVUs in January 2021. # Though Medicare will not, if your insurer pays consult codes (Outpt 99241-5; Inpt 99251-5), these codes have higher wRVUs than above. # All of these codes are billable for hospice patients except Non-F2F Prolonged Codes and Care Management Codes. # These are work RVUs only. Total RVUs include practice expense and malpractice expense RVUs as well. # RVU information comes from the Medicare Fee Schedule Lookup, shortened at https://go.cms.gov/1QdW07Z
Inpatient Billing – from 1995 Medicare Highmark Audit Tool E&M Initial Consult (HIGH): - 4 point HPI - 10 point ROS - PMFSH (all 3) - 8 system Exam - 2 of 3 High-level MDM: - ≥ 4 points Dx - ≥ 4 points Data - High Risk E&M Follow-up Visit(HIGH): - Either 4 point HPI and 2 point ROS - OR 8 system Exam - 2 of 3 High-level MDM: - ≥ 4 points Dx - ≥ 4 points Data - High Risk Risk Time-based billing: “I spent ______ minutes in Admits/Medicare Consult Inpt Consult (Not M’care) Follow-up the care of this patient, >50% in Level 1 – 30 min Level 3 – 55 min Level 1 – 15 min counseling and care coordination.” Level 2 – 50 min Level 4 – 80 min Level 2 – 25 min Prolonged service: include “Time in / Time out” Level 3 – 70 min Level 5 – 110 min Level 3 – 35 min ACP (99497 – 16-45min; +99498 – 46-75min)
JOURNAL OF PALLIATIVE MEDICINE Special Report Volume 19, Number 12, 2016 ª Mary Ann Liebert, Inc. DOI: 10.1089/jpm.2016.0202 Top 10 Tips for Using Advance Care Planning Codes in Palliative Medicine and Beyond 1,2 Jean Acevedo, LHRM, CPC, CHC, CENTC, 3 Christopher A. Jones, MD, 4 and Arif H. Kamal, MD, MBA, MHS 5,6 Janet Bull, MD, MBA, Abstract Although recommended for all persons with serious illness, advance care planning (ACP) has historically been a charitable clinical service. Inadequate or unreliable provisions for reimbursement, among other barriers, have spurred a gap between the evidence demonstrating the importance of timely ACP and recognition by payers for its delivery. 1 For the first time, healthcare is experiencing a dramatic shift in billing codes that support increased care management and care coordination. ACP, chronic care management, and transitional care management codes are examples of this newer recognition of the value of these types of services. ACP discussions are an integral component of comprehensive, high-quality palliative care delivery. The advent of reimbursement mechanisms to recognize these services has an enormous potential to impact palliative care program sustain- ability and growth. In this article, we highlight 10 tips to effectively using the new ACP codes reimbursable under Medicare. The importance of documentation, proper billing, and nuances regarding coding is addressed. Keywords: advance care planning; billing and coding; community-based palliative care; inpatient palliative care; outpatient palliative care; revenue when ACP processes are supported by project or grant Introduction funding only and not routine reimbursement from payers, A core component of high-quality palliative care (PC) regular adoption of ACP is often not realized outside of re- delivery is facilitation of regular advance care planning search settings. As many begrudgingly remember, an attempt (ACP) discussions. The National Hospice and PC Organiza- to include payment for ACP in 2009s Patient Protection and Affordable Care Act was derided as ‘‘death panels’’ 5 and the tion define ACP as ‘‘making decisions about the care you provision was dropped from the final bill. 6 would want to receive if you become unable to speak for yourself.’’ ACP also includes sharing care options for patients After several years of continued requests by healthcare and diagnosed with a serious illness, permitting patients to share patients’ rights groups to pay providers for ACP discussions values and preferences for care with loved ones who will act as with their patients, the Centers for Medicare and Medicaid surrogates, and, sometimes, completing advance directive Services (CMS) reversed course. On October 30, 2015, CMS (AD) paperwork to put those wishes in writing. 2 Importantly, announced a ‘‘proposal that supports patient- and family- ACP constitutes a longitudinal and dynamic process that re- centered care for seniors and other Medicare beneficiaries by enabling them to discuss ACP with their providers.’’ 7 Yet, quires thoughtful, regular, and often time-intensive conversa- tions between patients, their loved ones, and clinicians. payers did not provide robust guidance for how clinicians A major barrier to widespread facilitation of ACP by cli- should implement these changes. In this article, we will nicians has been lack of recognition by payers through ap- present 10 tips to compliantly provide ACP services to propriate reimbursement. Efforts at increasing completion of Medicare patients and offer insight into billing for these AD in the community 3 and skilled nursing facility settings 4 services. While the information we provide is intended for an have had limited success but have not led to widespread, audience of PC practitioners, the information is applicable to sustained increases in AD completion. As would be expected, providers of all specialties. 1 Main Line Health, Radnor, Pennsylvania. 2 Lankenau Medical Center, Wynnewood, Pennsylvania. 3 Acevedo Consulting, Inc., Delray Beach, Florida. 4 Four Seasons Compassion for Life, Flat Rock, North Carolina. 5 Duke Palliative Care, Durham, North Carolina. 6 Duke Cancer Institute, Durham, North Carolina. 1249
Recommend
More recommend