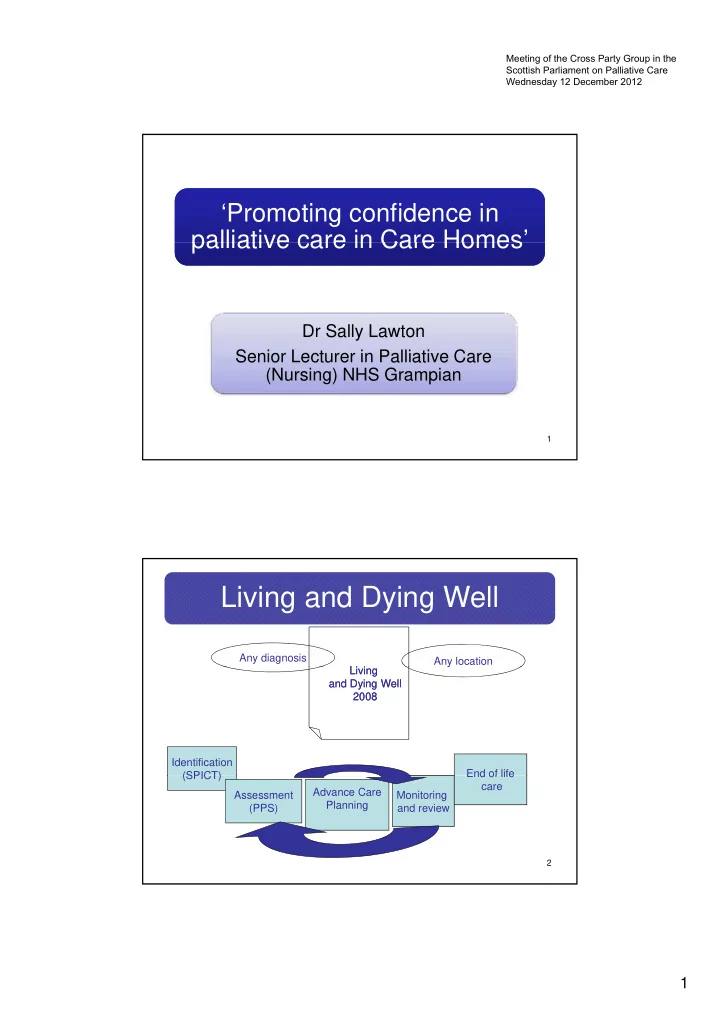
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 ‘Promoting confidence in ‘Promoting confidence in palliative care in Care Homes’ palliative care in Care Homes’ palliative care in Care Homes palliative care in Care Homes Dr Sally Lawton Senior Lecturer in Palliative Care S i L t i P lli ti C (Nursing) NHS Grampian 1 Living and Dying Well Any diagnosis Any location y Living Li i Living Li i and Dying Well and Dying Well 2008 2008 Identification End of life End of life (SPICT) (SPICT) care Advance Care Assessment Monitoring Planning (PPS) and review 2 1
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 How did we build confidence? Recognising the palliative environment Giving staff tools to assess and recognise change Helping staff to liaise more effectively with local Primary Care Teams Giving staff tools to develop advance care plans Discussing end of life care using after death reviews 3 The structure of the Project 4 2
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 5 Palliative environment Palliative Care categories (n=4204) 800 700 600 500 Shire Nursing Shire Residential number city nursing 400 city residential city VSH 300 200 100 0 dementia organ failure frailty mental health issues malignancy Learning Difficulties palliative category 6 3
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 The PPS PPS Ambulation Activity & evidence Self-care Intake Conscious level Level of disease 100% Full Normal activity & work Full Normal Full No evidence of disease 90% Full Normal activity & work Full Normal Full Some evidence of disease 80% Full Normal activity with Full Normal or reduced Full effort Some evidence of disease 70% Reduced Unable Normal job/work Full Normal or reduced Full Significant disease 60% Reduced Normal or reduced Full or confusion Unable hobby/house Occasional assistance work necessary Significant disease 50% Mainly sit/lie Unable to do any work Considerable assistance Normal or reduced Full or confusion Extensive disease required 40% Mainly in bed Unable to do most Mainly assistance Normal or reduced Full or drowsy activity ti it +/- confusion / f i Extensive disease 30% Totally bed bound Unable to do any activity Total care Normal or reduced Full or drowsy Extensive disease +/- confusion 20% Totally bed bound Total care Minimal to sips Unable to do any activity Full or drowsy Extensive disease +/- confusion 10% Totally bed bound Unable to do any activity Total care Mouth care only Drowsy or coma Extensive disease +/- confusion 0% Death - - - - 7 Assessment tool – the PPS PPS Data (n=2742) 900 900 800 700 600 500 Nursing Home Residential Home 400 Very Sheltered Housing 300 200 100 0 PPS 70 or more PPS 60 PPS 50 PPS 40 PPS 30 PPS 20 PPS 10 8 4
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 Nursing care Activities related to the PPS Scores ( by Sally Lawton September 2010 Roxburghe House) • Consider physical, psychological, spiritual and social needs at each level • Create a rapport that enables the patient/family/carer to express their understanding of their situation and explore concerns • Consider environmental factors that will enhance care • Liaise with relevant health/social care agencies as required • skin care that minimizes skin breakdown •food fluid and nutritional intake as appropriate •food, fluid and nutritional intake as appropriate PPS Score >/= 70 (promotion of self care) • continence care that protects the skin Supervise care activities that promote wellbeing using existing local care plans •wound/stoma care that controls exudate and lessens odour • concordance with prescribed medication •assessing and monitoring symptoms • moving and handling using appropriate equipment • skin care that minimizes skin breakdown PPS Score 40 -60 (assessment, monitoring and review) • oral care to promote a healthy mouth Assess, review and assist as required with care activities that • food, fluid and nutritional intake as appropriate maximise wellbeing using existing local care plans • continence care that protects the skin • wound/stoma care that controls exudate and lessens odour •concordance with prescribed medication •assessing and monitoring symptoms •assisting with moving and handling using appropriate equipment •providing skin care that minimizes skin breakdown •providing oral care that prevents complications associated with dry mouths PPS Score 10 - 30 (High nursing dependency) •assisting with food, fluid and nutritional intake as appropriate Undertake care activities to promote comfort using existing local care •providing continence care that protects the skin plans •providing wound/stoma care that controls exudate and lessens odour •administering prescribed medication •assessing and monitoring symptoms 9 PPS re-assessments Total changes in PPS (n=2061) 1000 900 800 700 600 Nursing Home Aberdeenshire(n=508) bers Residential Home Aberdeenshire (n=183) 500 Nursing Home Aberdeen city (n=1020) num Residential Homes Aberdeen City (n=237) VSH Aberdeen City (n=113) 400 300 200 100 0 PPS static PPS decreasing PPS increasing PPS status 10 5
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 End of life care - Deaths Deaths (n=293) 300 250 200 numbers 150 100 50 0 deaths in the home deaths in hospital unknown death in community hospital 11 Comments/reflections about the deaths – What went well Enabling the resident to fulfil their Enabling the resident to fulfil their preferred place of care Working with the family and Teamwork between providing all care the home and Primary Care Primary Care Effective symptom control and equipment 12 6
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 Comments/reflections about the deaths – problems Patient died in hospital Very sudden decline and death – no indication (8) Ambulance was sent and patient admitted to hospital instead of Care was reactive – no OOH visit DNA CPR Problems with hospital discharge – Naso-gastric Problems with hospital discharge – Naso-gastric tube, inappropriate transportation No review of medication when resident was unable to swallow No medication for agitation 13 Comments/reflections about the deaths – suggestions More knowledge about More knowledge about Improved communication Improved communication palliative care needed by between Care Home, family and Primary Care staff in the Home and Primary Care staff Earlier review and Earlier review and Should have used the PPS Should have used the PPS ACP needed and improve documentation 14 7
Meeting of the Cross Party Group in the Scottish Parliament on Palliative Care Wednesday 12 December 2012 Areas for development On-going need for closer links with Primary Care for some homes Competing priorities! Aim to reduce ‘reactive’ care DNA CPR Staffing issues 15 Conclusion Successful Project – welcome by the 81 Care Homes Staff want to provide care until the end of life Project approach helped to increase confidence Evidence that Homes are adapting practice p g p • Using the PPS • Working with GPs to develop ACPs Project approach being used in Community Hospitals and Department of Medicine for the elderly 16 8
Recommend
More recommend