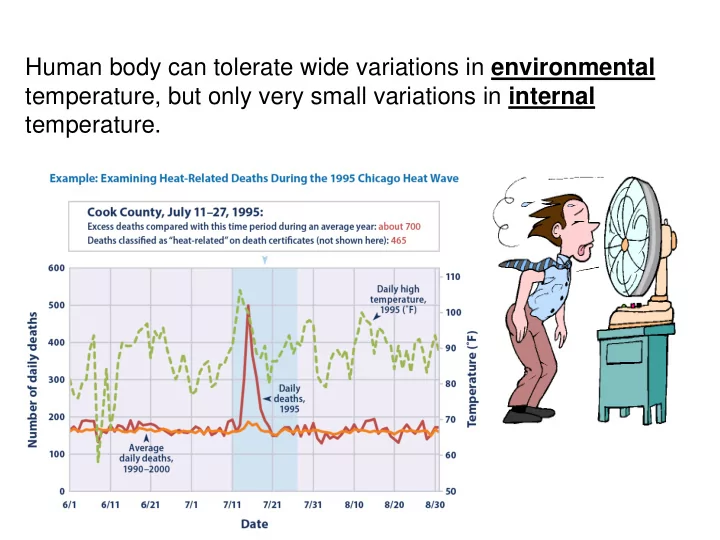
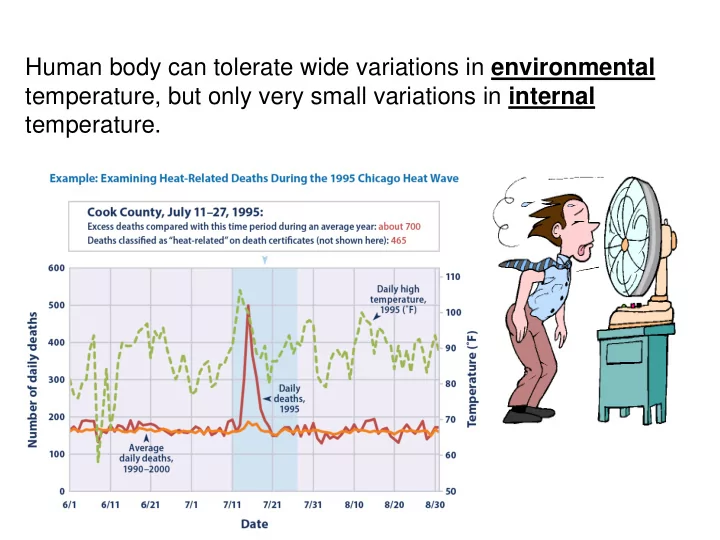
Human body can tolerate wide variations in environmental temperature, but only very small variations in internal temperature. Several of the gentlemen present, as During 1979--1999, a total of 8,015 deaths in the United States were associated with well as myself, went into the room excessive heat exposure . without shirts … when the thermometer Source: National Center for Health Statistics had risen much higher, almost to 260 ° F ( 127 ° C), and found that we could bear that very well, … C. Blagden; Philos Trans Royal Soc (Lond) 65:111-123, 1775.
What are the primary mechanisms for heat dissipation in humans?
Vasoconstrictor Vasodilator Nerve activity Skin Blood Flow 85-95% 5-15% Hypothermia Normothermia Hyperthermia
Other influence (i.e. vasoactive peptides, nitric oxide) Ach Sweat gland
Condition A Skin Blood Flow and/or Sweat Rate Slope Condition B Slope Threshold Threshold Internal Temperature
Cutaneous Vasculature Efferent Afferent Vasodilation Internal Temp Central Nervous Skin Temp Vasoconstriction System Other Variables * Aging * Pathology * Drugs * Skin Injury Sweat Gland
Rowell Approach
Skin Temp (Ts) Blood Temp (Tb) Where is this blood going? Skin Blood Flow Normothermia: 300-500 ml/min Heat Stress: 6,000+ ml/min Rowell, Physiol Rev 1974
Brain blood flow heart rate; or BP Central blood volume Splanchnic and renal Skin blood flow & blood flow and volume volume Sympathetic Activity
Aging and Heat Stress Why are we concerned? Weather related mortality by age in the US (2006-2010) Center of Disease Control
20-25 years 60-74 years Subjects exercised @ 50%VO 2 max in 36 deg C room Kenney et al. 1997
What is the problem reporting data as such? Inoue et al. Eur J Appl Physiol 1998
Think about possible mechanisms responsible for the attenuated skin blood and sweating responses in elderly compared to young subjects – how would you design studies to identify these mechanisms? Peripheral versus Central
Kenney & Fowler J Appl Physiol 1988
Minson et al. J Appl Physiol 1998
Insufficient increases in cardiac output and thus attenuated increases in skin blood flow …. or Restricted skin blood flow responses resulting from less vasodilation and thus less of a need to increase cardiac output How would you address this question?
Gagnon et al. 2017
Gagnon et al. 2017
Brain blood flow heart rate; , BP Central blood volume Splanchnic and renal Skin blood flow & blood flow and volume volume Sympathetic Activity Heat stress, independent of a hemorrhage insult
Schlader, Wilson, Crandall 2016
Pre-LBNP 15 mmHg LBNP 30 mmHg LBNP Normothermia Heat Stress Crandall, Wilson, Marving, Bundgaard-Nielsen, Seifert, Klausen, Andersen, Secher, Hesse J Physiol (2012)
Discus possible mechanisms by which heat stress compromises tolerance to a hemorrhagic challenge – how would you design studies to identify these mechanisms? Autonomic Function Blood Pressure = Baroreceptors Cardiac Output x Systemic Vascular Resistance Cardiac Function Central Blood Volume Cerebral Vasculature Hydration
“Central” Normothermia Blood Volume Skin blood volume Heat Stress “Central” Blood Volume
What if central blood volume is “normalized” relative to pre-heat stress levels 1.0 N=7 Survival Probability 0.8 0.6 0.4 0.2 Normothermia Heat stress 0.0 0 10 20 30 40 50 60 70 80 90 100 LBNP (mm Hg) Keller, Low, Wingo, Brothers, Hasting, Davis, Crandall J Physiol (2009)
“Central” Normothermia Blood Volume Skin blood volume Skin blood volume Heat Stress “Central” Blood Volume
What if central blood volume is “normalized” relative to pre-heat stress levels N=7 1.0 Survival Probability 0.8 0.6 0.4 Heat stress + volume 0.2 Normothermia Heat stress 0.0 0 10 20 30 40 50 60 70 80 90 100 LBNP (mm Hg) Keller, Low, Wingo, Brothers, Hasting, Davis, Crandall J Physiol (2009)
“Central” Normothermia Blood Volume Skin blood volume Skin Heat Stress “Central” Blood Volume Current Protocol: Army is heating hemorrhaging victims
Young Elderly Increases in Core Temperature Increases in Core Temperature Minson et al. J Appl Physiol 1998
Rowell, Human Circulation, 1986
Discus possible mechanisms responsible for the plateau in SKBF during exercise (in contrast to passive heat stress) – how would you design studies to identify if it is ”lack of further vasodilation” or withdrawal of vasoconstriction – and study (studies) to identify the importance of cardiac output.
100 REST Skin blood flow, % of maximal C 50 DYNAMIC EXERCISE B A 37 38 Internal Temperature, °C Gonzalez-Alonso et al J Physiol 2008
Discus mechanisms responsible for the reduction in stroke volume during exercise in the heat – why does it decline during exercise but not rest ? How would you design studies to support/test your hypothesis
Gonzalez-Alonso et al J Appl Physiol 1999 Gonzalez-Alonso et al J Physiol 1998
Dehydration trial Gonzalez-Alonso et al J Physiol 2008
Recommend
More recommend