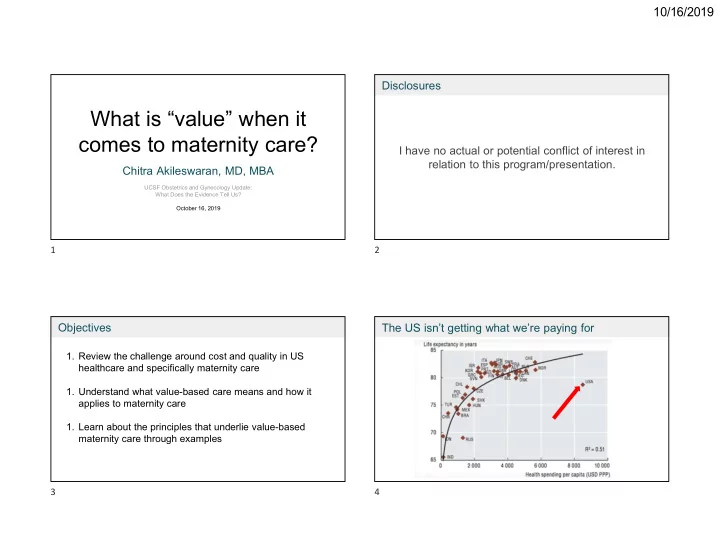
10/16/2019 Disclosures What is “value” when it comes to maternity care? I have no actual or potential conflict of interest in relation to this program/presentation. Chitra Akileswaran, MD, MBA UCSF Obstetrics and Gynecology Update: What Does the Evidence Tell Us? October 16, 2019 1 2 Objectives The US isn’t getting what we’re paying for 1. Review the challenge around cost and quality in US healthcare and specifically maternity care 1. Understand what value-based care means and how it applies to maternity care 1. Learn about the principles that underlie value-based maternity care through examples 3 4 1
10/16/2019 Roots of US healthcare crisis US maternity care rivals the costs of a royal birth Low emphasis Fee-for-service We are caring Who is included on prevention, encourages for an aging, and excluded as more on acute doing as much more chronically part of our treatment as possible ill demographic healthcare system? Access Payment Population Equity 5 6 Quiz #1: Spot the real headline: Affordability is a major issue for families 75% A. American women rate giving birth in the US “five stars” B. Our maternal mortality rate is a national 23% embarrassment 3% C. US lags when it comes to minimizing 0% “Ms. Martin called her local hospital inquiring about the price of maternity care; the finance childbirth complications office at first said it did not know, and then gave . . . . . . . . . . D. Despite OB shortage, US women love e t e . i . , t l m a a e her a range of $4,000 to $45,000. g r t o r a n c o t e r m t m i o their obstetricians l n h o a e s w n h B r w e O n “It was unreal,” Ms. Martin said. “I was like, How t a s e a c m g t i a r p i e l r s m S could you not know this? You’re a hospital.”’ u e U A O D 7 8 2
10/16/2019 Despite high costs of childbirth, US women are dying Our maternity outcomes are getting worse 10 11 Phrases you might have heard The mother-blaming narrative “Moving from volume to value” “Risk-based payment” “Value-based care” 12 13 3
10/16/2019 Quiz #2: What is value-based healthcare? Value is where US healthcare is headed 70% A. Value-based care means we are paid according to whether patients are satisfied B. Value-based care is care provided according to 28% a patient’s values C. Value-based care is a payment model that 1% 1% rewards the best possible outcomes for the least costs incurred . . . . . . . a a . . a e . D. Value-based care doesn’t have a clear e c o m s s d i i e e e e r r r a r a a a c c c c definition d d d e d e e s e s s s a a a a b b b b - - - e e - e e u u u u l l l a a a l V a V V V 14 15 What is value-based healthcare? What is value-based healthcare? Getting paid to do the right thing , Health outcomes + patient not just to do more Outcomes experience Rather than bill for each encounter/procedure, we will be paid per patient or episode. It will be up to us to manage the costs of care. Direct + indirect Cost costs of care Reframe care in terms of how well we solve our patients’ problems at a population level The highest value care achieves the Ex. Patient comes to you with fibroid uterus and debilitating AUB. The outcome best outcomes for the lowest cost she wants is not a hysterectomy - but to have her bleeding controlled. 17 18 4
10/16/2019 How do you use the concept of value today? How fee-for-service differs from paying for value Brand of detergent Price per ounce Fee-for-service Value-based payment Price Arm & Hammer $0.08 You are paid to do more for patients You are paid to produce the best Scent Cheer $0.16 (visits, procedures, etc.) outcomes for patients Packaging Tide $0.13 aesthetic Focuses on sick care Focuses on preventive care Tide Free & Clear $0.23 Environmental Results in fragmented care, duplication, Rewards care coordination, limiting impact Walmart Great Value $0.08 Convenience of and overutilization redundancy - our “INVISIBLE” work purchase Trader Joe’s $0.07 No reason to innovate, use technology to Incentivizes innovative ways to see Method $0.75 reduce in-person care patients to limit costs, i.e. virtual care Costs increase even if quality stagnates Costs should decrease as quality climbs The goal of marketing to make you believe that the value equation (what you get versus what you pay for) is positive - more positive than the alternatives 19 20 Value-based care: Care coordination example Value-based care: Care coordination example Pregnant patient with a history of a severe postpartum hemorrhage with her prior Pregnant patient with a history of a severe postpartum hemorrhage with her prior pregnancy transfers her care to you at 24 weeks gestation due to relocation. pregnancy transfers her care to you at 24 weeks gestation due to relocation. During your visit with her, you learn that she has seen a hematologist in the past During your visit with her, you learn that she has seen a hematologist in the past and received blood work. She doesn’t know if she still needs to see a hematologist and received blood work. She doesn’t know if she still needs to see a hematologist or what the results of her blood work were. or what the results of her blood work were. Furthermore, she has a history of chronic hypertension for which she no longer Furthermore, she has a history of chronic hypertension for which she no longer takes medications, but doesn’t know what medication she used to be on. takes medications, but doesn’t know what medication she used to be on. She lives far away from your office and has a hard time getting to her visits due to She lives far away from your office and has a hard time getting to her visits due to childcare. childcare. 21 22 5
10/16/2019 Value-based care: Care coordination example ACOG Committee Opinion Which is likely to produce the best clinical outcome for this patient? Types of payment for high-value care A. The patient is responsible for collecting records from her prior 82% OB, hematologist, and primary care doctor and coordinate her Rewards for improving processes: % completion of postpartum visit, use of shared visits. It may mean she misses some visits with you and that you decision aids don’t have complete records. Penalties for unwanted outcomes: preventing B. You coordinate records collection, medication reconciliation, and 16% readmission call her to ensure she can make her upcoming visits before or 3% Payments for shared accountability: bundled after a long day of clinic. Sometimes you forget or don’t have payments for maternity care with providers time. keeping the savings or paying a penalty . . . . . . . . s d . n r t C. You are incentivized to hire someone to help you coordinate o o d p c e e z s r i e v Consumer-directed models: preferred r e i t s t n a care, because you will be reimbursed at a higher rate based on i n e t i c providers/hospitals, tiered formularies n d n e r i i o t e a o r p c a how well your patients achieve certain outcomes for your u u e h o o T Y Y practice, such as visit attendance. 23 25 Value-based maternity care What outcomes do we want to see in maternity care? Health Outcomes Patient Experience Low NTSV c-section rate Less birth-related trauma Maternity outcomes + Limit <39wk births Improved satisfaction patient experience with Few term NICU admits Better preparation for birth and Value-based pregnancy/birth/postpartum High VBAC rate postpartum maternity Good BP control Increased access to providers care Costs of maternity episode Appropriate weight gain Emotional/psychological support Less perinatal mood/anxiety Normal recovery and return to Meet breastfeeding goals life functions 26 27 6
10/16/2019 What costs do we want to limit in maternity care? Value-based care: Maternity care example May 2019: Launched bundled payment program in NJ Costs and TX for prenatal, antepartum hospitalizations, L&D, and postpartum care up to 60 days. Fewer unnecessary prenatal visits Fewer unnecessary ED visits Providers keep the difference if care costs less than the payment. Fewer unnecessary ultrasounds Limit redundant labs and preventive screening Risks Multiple visits for one problem (e.g. nutrition visit separate from OB Goals ● If one clinician bears the risk, how will ● Can we reduce unnecessary visit for GDM) team-based care work? procedures including c-sections? ● How is a “low risk” patient to be ● Can we identify risks early and avoid Fewer unnecessary cesareans defined? Will payment be risk- hospitalizations? adjusted? Fewer postpartum readmissions ● Can we promote quality standards (c- ● How will providers track quality in real- section rate, avoiding early deliveries)? time to ensure payment? 28 29 Some principles of value-based maternity care Value-based maternity care: Ownership Forthcoming study of 11,000 California births Ownership via commercial payor OB office is medical “home” Matched practices with Personalization Labs, basic ultrasound can be highest quality metrics done in-office with lowest costs of care Nurse triage and same-day visits Integration Visited high-value available to avoid urgent care/ED practices to understand Specialist consultations are one-off, common qualities patient returns to OB for care 30 31 7
Recommend
More recommend