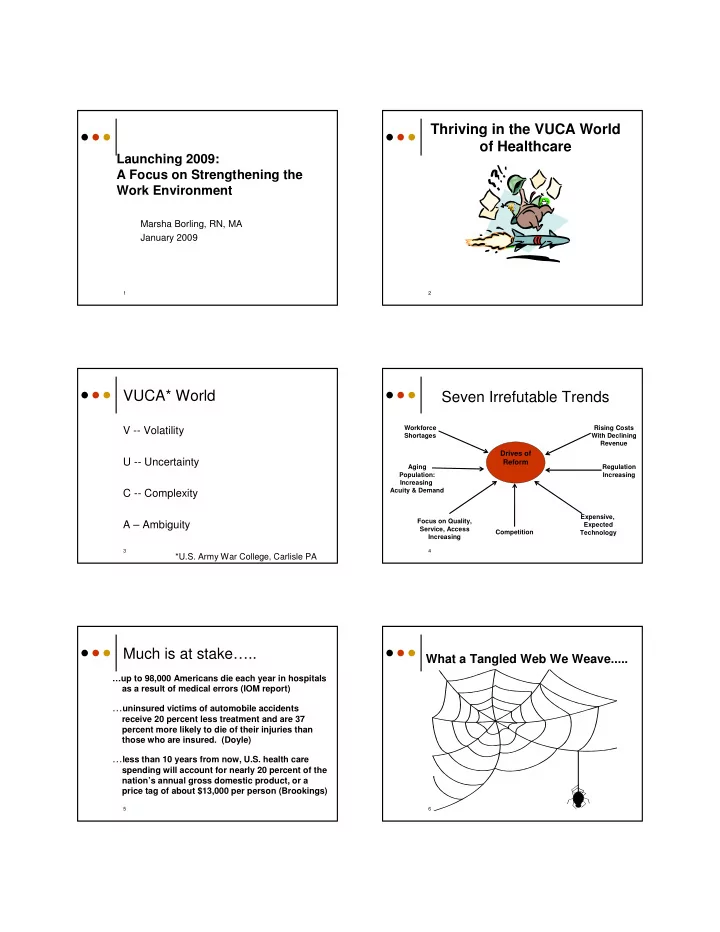
Thriving in the VUCA World of Healthcare Launching 2009: A Focus on Strengthening the Work Environment Marsha Borling, RN, MA January 2009 1 2 VUCA* World Seven Irrefutable Trends Workforce Rising Costs V -- Volatility Shortages With Declining Revenue Drives of U -- Uncertainty Reform Aging Regulation Population: Increasing Increasing Acuity & Demand C -- Complexity Expensive, Focus on Quality, A – Ambiguity Expected Service, Access Competition Technology Increasing 3 4 *U.S. Army War College, Carlisle PA Much is at stake….. What a Tangled Web We Weave..... …up to 98,000 Americans die each year in hospitals as a result of medical errors (IOM report) … uninsured victims of automobile accidents receive 20 percent less treatment and are 37 percent more likely to die of their injuries than those who are insured. (Doyle) … less than 10 years from now, U.S. health care spending will account for nearly 20 percent of the nation’s annual gross domestic product, or a price tag of about $13,000 per person (Brookings) 5 6
Prioritizing time, talent & treasure What have we learned? � Once again, there are no “silver bullets,” much of what needs to be done, we already know � We have leaders, but not enough WORK “IN” WORK “ON” WORK TO leadership THE BUSINESS THE BUSINESS “ADVANCE” delivering current improving current THE BUSINESS services, processes services and processes moving the � Too many #1 priorities = enterprise to new ground mismanagement of TTT 7 8 General Satisfaction What have we learned? Trends in Healthcare � The unions are listening to healthcare employees � Effective change leadership and crucial conversations are not healthcare competencies � Improving the work environment to reduce vulnerability does work 9 10 Relationship between employee Relationship between employee turnover and profitability * VHA, 2001 turnover and patient care * VHA, 2001 11 12
Does having a union create a better work environment? Project Objectives * (satisfaction changes at four hospitals unionized after 2003) Hospital 2002 Scores Current Scores � Identify the essential work environment factors, #1 – employees 3.16 2.84 behaviors and practices that contribute to a less #1 – physicians 3.05 2.91 vulnerable work environment #2 –employees 3.05 2.78 � Compile these factors into a prototype that can be applied in any facility #2 – physicians 2.97 2.77 #3 – employees 3.17 2.78 � Measure organizations against the prototype #3 – physicians 3.01 2.87 #4 – employees 3.07 2.99 #4 – physicians 3.23 3.00 13 14 The Original Cohort Studied Additional assessments completed: Additional assessments completed: Additional assessments completed: Additional assessments completed: � Ten facilities o Facilities: 71 � Identified based on demonstration of positive performance: o One-hour interviews with Senior � Nursing staff turnover rates and middle level leadership: 1,634 o � Nursing staff satisfaction � Physician satisfaction o Two-hour focus group meetings: 540 � Financial performance Total participants: 5,567 o � Patient satisfaction � Quality indicators 15 16 High performing organizations with low vulnerability had common practices in 5 platform areas: � Senior & Mid-level leadership What is your organization effectiveness doing to prepare? � Communication/voice � Nursing staffing ratios and staffing practices � Culture/Employee recognition � Compensation practices 17 18
6 New Year’s Resolutions for Overview of Today’s Sessions Healthcare Organizations � AM Session: � Leadership practices for a healthy work Enable more lantern carriers 1. environment Develop physician leaders 2. � Survival of the mid-level clinical leader Simplify and focus the organization 3. � Coaching clinical leaders Ensure accountability from the Board to 4. � PM Session: the front line � Voice Develop a 5-year workforce plan 5. � Effective staffing practices Renew efforts to strengthen work � Culture of empowerment and 6. environment and reduce vulnerability accountability Baird/Borling Associates, 2009 19 20 Leadership: What’s working Always begin with � Visibility of senior leadership is key, however leadership… needs to be the “right” visibility: � Differing expectations about what visibility means: Do you see us, or do we see you? � Desire for more spontaneous dialogue & connection Followers need three basic qualities � Structured without the appearance of structure from leaders: they want direction, � Visibility of front line leadership imperative: they want trust, and they want hope. � Scope narrower at front line so more “in the trenches” � Mid-level leaders spending less time in meetings, more time managing people and operations � “Hands on” but intentional about how and when --Warren Bennis 21 22 Leadership: What’s working ����� � Style: Situational but predominantly ���������� ������������� ���������� collaborative/facilitative � Micromanagement and autocratic styles used ������ ������ ������ only with cause ������ ��������� ��������� ��������� ����� ��������� ������ �������������� 23 24
Leadership: What’s working Leadership: What’s working � Indoctrination of new leaders includes � Observable leader behaviors align with orientation but relies heavily on coaching, expressed core values role modeling, assimilation from peer group � Leaders are highly visible & demonstrate � Selection of new leaders is defined and unstructured approachability structured � Follow through is consistent, promoting trust � Mid-level leaders have high morale and � Leaders show “human” side and strong peer network for problem solving and demonstrate work/life balance support � Leaders know and call employees by name � Management development is ongoing and � Balanced messaging regarding finance employs a variety of methods 25 26 Conclusions from BBA data: The Survival of the � More than 75% of hospitals assessed Frontline Manager: have key front line manager vacancies A Crisis in the Making � Toughest positions to recruit for: ICU, ED, Pharmacy and Surgical Services managers/directors � The “time to fill” middle management positions is lengthening � 6 key issues are driving dissatisfaction, burnout and turnover among frontline managers 27 28 #2: “The workload is killing me” #1: Role Issues � Uncontrolled bureaucracy: � Meetings � Scope � Paper work � Setting managers up to fail � Redundant reports � High performers rewarded with more � Rework caused by ineffective planning work, poor performers enabled � Lack of real prioritization at the senior � Budget driven decisions leadership level � Sandwich role � Self-imposed powerlessness � Good soldier vs. insurgent � Ineffective management skills � Up from the ranks � Pressure to perform � Fighting the fire vs. uncovering the cause � No think time 29 30
#4: Development of new & ��������������������� upcoming managers lacking � Fear of delegation: � Loss of stature—they’ll get the credit. � Loss of control—they may screw it up. � Inadequate (or missing altogether) � Reluctance to overburden staff—momma management orientation management. � Inadequate (either in amount or type) � Reluctance to seek help (imposter syndrome). ongoing management development � Lack of conscious comportment. � Need for a clear program to build bench � Reluctance to give (and get) constructive strength feedback. 31 32 #5: Diminished incentives #6: Lone wolf syndrome � 24/7 on-call responsibility � Isolation, especially in ED, OR, Women’s Center management roles � Back up for staffing holes � Format of typical management � Narrowing gap between staff and meetings is information-giving vs. manager pay problem solving, dialogue � Nobody likes me � Networking, team building, retreats seen as “frivolous,” expendable costs 33 34 �������������������������� ������������������ Conclusion: These issues are ������������������������� leading to burnout and turnover �������� among mid level managers, just at a time when the healthcare industry needs leadership more than ever before. 35 36
Recommend
More recommend