Transcatheter Aortic Valve Replacement Jesse Jorgensen, MD Medical - PowerPoint PPT Presentation
Transcatheter Aortic Valve Replacement Jesse Jorgensen, MD Medical Director, Cardiac Catheterization Laboratory Greenville Health System Greenville, South Carolina, USA January 30, 2016 Aortic Stenosis is Life Threatening and Progresses
Transcatheter Aortic Valve Replacement Jesse Jorgensen, MD Medical Director, Cardiac Catheterization Laboratory Greenville Health System Greenville, South Carolina, USA January 30, 2016
Aortic Stenosis is Life Threatening and Progresses Rapidly Valvular Aortic Stenosis in Adults (Average Course) • Survival after onset of symptoms 50% at 2 yrs, 20% at 5 yrs • Surgical intervention should be performed promptly once even minor symptoms occur 2 Ross J Jr, Braunwald E. Aortic stenosis. Circulation. 1968;38 (Suppl 1):61-7. 2 C.M. Otto. Valve Disease: Timing of Aortic Valve Surgery. Heart 2000
Aortic Valve Replacement Improves Survival Patient Survival AVR, no Sx 100 AVR, Sx 90 No AVR, no Sx 80 No AVR, Sx 70 Survival, % 60 50 40 30 20 10 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Years Brown ML et al. The benefits of early valve replacement in asymptomatic patients with severe aortic stenosis. J Thorac Cardiovasc Surg. 2008;2:308-315.
Surgical AVR: Not Available To All Patients 31.8% did not undergo intervention, most frequently because of comorbidities
Aortic Stenosis Undertreatment is Profound
Mortality With Standard Therapy Is Worse Than With Certain Metastatic Cancers National Institutes of Health. National Cancer Institute. Surveillance Epidemiology and End Results. Cancer Stat Fact Sheets. Data on file, Edwards Lifesciences LLC. Analysis courtesy of Murat Tuczu.
Percutaneous Aortic Valve Development Professor Alain Cribier (Rouen, France) First described percutaneous aortic valve interventions in 1985 Proved that a stent could be deployed without removing the diseased native valve Implanted first percutaneous aortic valve on a patient on April 16, 2002
Edwards SAPIEN Transcatheter Valve Bovine pericardial tissue The Carpentier-Edwards ThermaFix process* is intended to minimize the risk Stainless steel frame of calcification, helping preserve valve performance PET skirt
Edwards SAPIEN
TAVR: Edwards Valve NEJM 2011; 364:2187-2198
Self Expanding Technology: CoreValve (Medtronic) 2007 CE Mark 2014 FDA Approval
Evolut R System Catheter Delivery System 14Fr-equivalent profile Loading System Transcatheter Valve (26, 29 mm) Supra-annular design, optimized sealing Meredith EuroPCR 2015 13 CoreValve Evolut R CE Study MDT Confidential
TAVR Access 1. Transfemoral 2. Direct Aortic 3. Subclavian 4. Transapical
TAVR Patient Evaluation STS Score <4 Low Risk 4-8 Intermediate Risk * >8 High Risk * Inoperable: >50% death or serious irreversible condition Agarwal S et al. Heart 2015;101:169-177
Patient-Focused Multidisciplinary Heart Team Approach • Multidisciplinary in all aspects: – Patient selection – Procedure Planning – Patient Treatment – Post Operative care
Valve Sizing: TEE
Valve Sizing: CT
CTA: Critical for determining Access
TAVR is the standard of care for inoperable patients with severe AS
TAVR Results: Mean Gradient & Valve Area
PARTNER Cohort B Primary Endpoint
All Cause Mortality (ITT): 5 year Follow up Median Survival Kapadia TCT Sept 2014
Repeat Hospitalization: TAVR vs. Standard Treatment Kapadia TCT Sept 2014
PARTNER B Mean Gradient and Valve Area at 5 years Kapadia TCT Sept 2014
Stroke following TAVR: Inoperable cohort
Vascular Complications: TAVR vs. Standard Treatment
Yakubov TCT 2014
CoreValve Extreme Risk JACC 2014;63:1972-81
CoreValve Extreme Risk Clinical Outcomes at 1 and 12 Months JACC 2014;63:1972-81
CoreValve Hemodynamics and Functional Improvement JACC 2014;63:1972-81
CoreValve Extreme Risk 2 year Outcomes
TAVR is AT LEAST as good as Surgical AVR in High Risk patients
Echo Aortic Valve Gradients: Sapien TAVR vs. SAVR
PARTNER A Primary Endpoint: 1 Year All-Cause Mortality TAVR vs SAVR
Cohort A Quality of Life: TAVR vs. SAVR
High Risk: TAVR vs SAVR
Paravalvular Aortic Regurgitation: Sapient TAVR vs. SAVR
CV Mortality Stratified by PV Leak (ITT) Partner A
Corevalve High Risk Adams ACC 2014
Primary Endpoint: 1 Year All-cause Mortality Surgical Transcatheter 19.1% 14.2% 4.5% P = 0.04 for superiority 3.3% Adams ACC 2014
All Stroke Adams ACC 2014
Other Endpoints Events* 1 Month 1 Year TAVR SAVR P Value TAVR SAVR P Value Vascular complications (major), % 5.9 1.7 0.003 6.2 2.0 0.004 Pacemaker implant, % 19.8 7.1 <0.001 22.3 11.3 <0.001 Bleeding 13.6 35.0 <0.001 16.6 38.4 <0.001 (life threatening or disabling),% New onset or worsening atrial fibrillation, % 11.7 30.5 <0.001 15.9 32.7 <0.001 Acute kidney injury, % 6.0 15.1 <0.001 6.0 15.1 <0.001 * Percentages reported are Kaplan-Meier estimates and log-rank P values Adams ACC 2014
Echocardiographic Findings Adams ACC 2014
Paravalvular Regurgitation 45
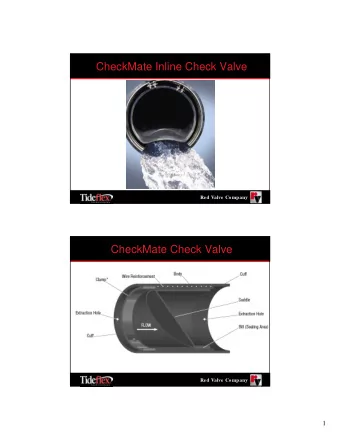
Vascular Safety: Get Smaller Terumo Solopath: 15f insertion, balloon expandable to 19f. Corevalve compatible
Edwards evolution of valve design SAPIEN SAPIEN XT SAPIEN 3
Evolution of the Edwards Balloon- Expandable Transcatheter Valves Kodali ACC 2015
PARTNER II Study Design Leon ACC 2013
PARTNER II Inoperable Cohort Leon ACC 2013
PARTNER II Mortality and Stroke Leon ACC 2013
PARTNER II: Comparison of Valve Function Leon ACC 2013
PARTNER II: Comparison Vascular Complications Leon ACC 2013
Partner II S3 Trial Kodali ACC 2015
Kodali ACC 2015
Kodali ACC 2015
Kodali ACC 2015
Kodali ACC 2015
Kodali ACC 2015
TAVR Growth in U.S. Sites Enrolled in the TVT Registry J Am Coll Cardiol. 2015;66(25):2813-2823.
Complications in patients undergoing TAVR Neurological Complications Bleeding and Vascular Complications
So, What’s New?
Valves Under Development JACC 2012;60:483-92
Cerebral Emboli During TAVR and SAVR Using Transcranial Doppler TAVR, N=85 SAVR, N=42 1 patient in each arm suffered a stroke at 30 day follow up Alassar Ann Thor Surg 2015, In Press
Protection of cerebral events during TAVR Embrella Embolic Deflector Triguard (Edwards Lifesciences) (Keystone Heart, Herzliya Pituach, Israel) Freeman et al. CCI 2014;84(6):885-896
Protection of cerebral events during TAVR Claret Montage (Claret Medical, CA)
Valve in Valve Implantation JACC 2011; 58 (21):2196-209
Valve in Valve Implantation JAMA 2014; 312(2):162-70
TAVR for Pure Aortic Insufficiency Wendt D et al. JACC Int. 2014;7(10):1159-1167.
Focus shifting from clinical outcomes to procedural efficiency Babaliaros V et al. JACC Int 2014;7(8):898-904
Bern TAVI Registry: The European Experience with less than high risk patients Wenaweser P et al. Eur Heart J 2013;34:1894-1905
Conclusions 1. TAVR (TAVI) is the current standard of care for inoperable patients with severe AS 2. TAVR is an acceptable option for high risk operable patients 3. TAVR is an acceptable option for patients with prior surgical AVR (? And MVR) 4. TAVR may soon be an option for intermediate and low risk patients
Conclusions • Outcomes will continue to improve with smaller profile delivery systems and methods to reduce paravalvular leak • Stroke prevention: embolic protection devices • Dedicated valve designs for pure aortic insufficiency • TMVR
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.