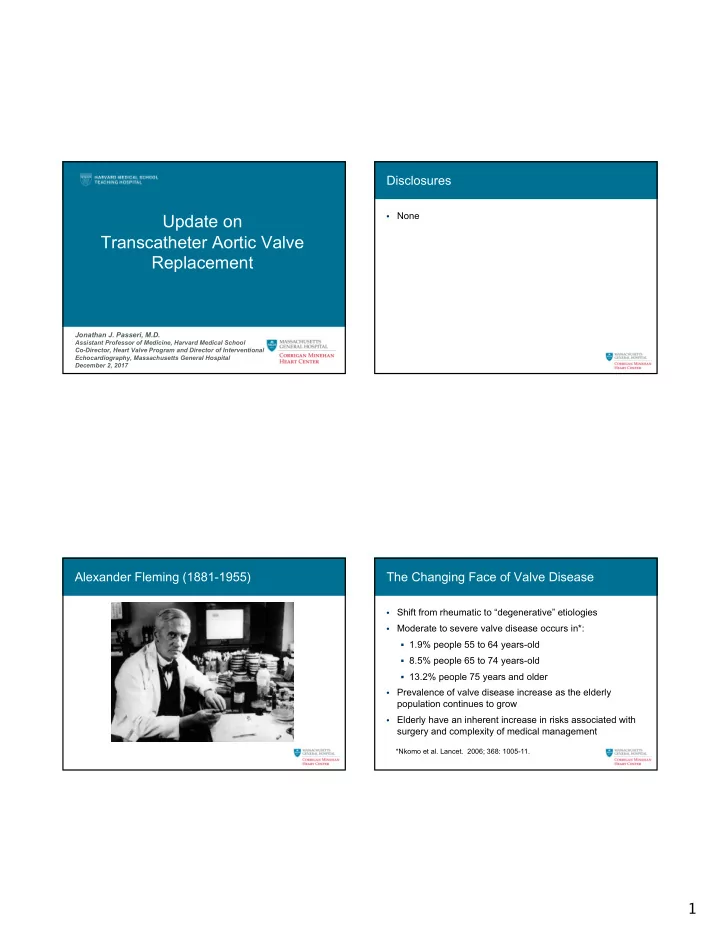
Disclosures None Update on • Transcatheter Aortic Valve Replacement Jonathan J. Passeri, M.D. Assistant Professor of Medicine, Harvard Medical School Co-Director, Heart Valve Program and Director of Interventional Echocardiography, Massachusetts General Hospital December 2, 2017 Alexander Fleming (1881-1955) The Changing Face of Valve Disease Shift from rheumatic to “degenerative” etiologies • Moderate to severe valve disease occurs in*: • § 1.9% people 55 to 64 years-old § 8.5% people 65 to 74 years-old § 13.2% people 75 years and older Prevalence of valve disease increase as the elderly • population continues to grow Elderly have an inherent increase in risks associated with • surgery and complexity of medical management *Nkomo et al. Lancet. 2006; 368: 1005-11. 1
Prevalence of Valve Disease by Age Distribution of Native Heart Valve Disease Nkomo et al. Lancet. 2006; 368: 1005-11. Iung et al. Nat. Rev. Cardiol. 2011;8: 162-172 Calcific Aortic Stenosis: Mechanisms Calcific Aortic Stenosis: Mechanisms Calcific aortic stenosis is a biologically • active process Lipid accumulation • – LDL accumulation and oxidation Inflammation • – T-cells, monocytes, inflammatory mediators, cytokines Calcification • – Osteoblast expression, bone formation Rajamannan et al. Nature Clinic Prac CV Med 2007;5:254 2
Pathophysiology Aortic Stenosis Natural History of Aortic Stenosis Aortic Stenosis LV outflow obstruction LVSP LVET LVDP Aortic Pressure LV Mass Myocardial O2 Diastolic time LV dysfunction consumption Myocardial O2 Myocardial LV failure supply ischemia Ross J Jr, Braunwald E. Circulation 1968; 38: 61–67 Aortic Valve Replacement Surgery Surgery in Elderly Patients with Severe AS Aortic Stenosis >75 years N=408 No severe AS Severe AS N=284 N=124 No symptoms Severe symptoms N=68 N=216 No intervention Intervention N=72 (33%) N=144 (67%) Iung et al. Eur Heart J. 2005; 26: 2714 3
Transcatheter Aortic Valve Replacement Henning Rud Andersen PARTNER : P lacement of A o RT ic Antegrade Transcatheter Aortic Valve Replacement: First Human Case Reported Tra N scathet ER Valves Trial Symptomatic Severe Aortic Stenosis ASSESSMENT: High-Risk AVR Candidate 3,105 Total Patients Screened Total = 1,057 patients N = 699 Inoperable N = 358 High Risk 2 Parallel Trials: Individually Powered ASSESSMENT: ASSESSMENT: Yes Transfemoral No Transfemoral Access Access Transfemoral (TF) Transapical (TA) Yes No 1:1 Randomization 1:1 Randomization 1:1 Randomization Not In Study N = 244 N = 248 N = 104 N = 103 N = 179 N = 179 Standard TF TAVR AVR TA TAVR AVR TF TAVR Therapy VS VS VS Primary Endpoint: All-Cause Mortality Primary Endpoint: All-Cause Mortality at 1 yr Over Length of Trial (Superiority) (Non-inferiority) Co-Primary Endpoint: Composite of All-Cause Mortality and Repeat Hospitalization (Superiority) Cribier A, et al. Circulation 2002;106:3006-8 4
All Cause Mortality (ITT) PARTNER Trial (1A): 5-Year Outcomes Mack et al. Lancet 2015; 385:2477-2484 Torsten P. Vahl et al. JACC 2016;67:1472-1487 CoreValve Pivotal Trial: Extreme Risk CoreValve US Pivotal Trials All Cause Mortality Figure Legend: Cumulative Event Curve for All-Cause Mortality or Major Stroke Event rates were calculated with Kaplan-Meier methods. Brackets indicate 95% confidence interval. J Am Coll Cardiol. 2014;63(19):1972-1981. 5
CoreValve Pivotal Trial: High-Risk The PARTNER 2A Trial Two-year outcomes Study Design Symptomatic Severe Aortic Stenosis ASSESSMENT by Heart Valve Team Operable (STS ≥ 4%) Randomized Patients n = 2032 ASSESSMENT: Yes No Transfemoral Access Transfemoral (TF) Transapical (TA) / TransAortic (TAo) 1:1 Randomization (n = 1550) 1:1 Randomization (n = 482) TF TAVR Surgical AVR TA/TAo TAVR Surgical AVR VS. VS. (n = 775) (n = 775) (n = 236) (n = 246) Primary Endpoint: All-Cause Mortality or Disabling Stroke at Two Years Reardon et al. J Am Coll Cardiol. 2015;66(2):113-121. PARTNER 2: Time-to-event curves PARTNER 2: Time-to-event curves Leon et al. NEJM. 2016;374(17):1609-1620. Leon et al. NEJM. 2016;374(17):1609-1620. 6
Primary Endpoint Events (ITT) Other Clinical Endpoints (ITT) At 30 Days and 2 Years At 30 Days and 2 Years 30 Days 2 Years 30 Days 2 Years Events (%) Events (%) TAVR Surgery TAVR Surgery TAVR Surgery TAVR Surgery p-value* p-value* p-value* p-value* (n = 1011) (n = 1021) (n = 1011) (n = 1021) (n = 1011) (n = 1021) (n = 1011) (n = 1021) Death (all-cause) Rehospitalization 6.5 6.5 0.99 19.6 17.3 0.22 6.1 8.0 0.11 19.3 21.1 0.33 and Stroke (disabling) 1.2 1.9 0.22 3.6 4.1 0.56 MI Death Major Vascular 7.9 5.0 0.008 8.6 5.5 0.006 3.9 4.1 0.78 16.7 18.0 0.45 Complications All-cause Life-Threatening / 3.3 3.2 0.92 10.1 11.3 0.38 10.4 43.4 <0.001 17.3 47.0 <0.001 Cardiovascular Disabling Bleeding Neurological Events AKI (Stage III) 1.3 3.1 0.006 3.8 6.2 0.02 New Atrial Fibrillation 9.1 26.4 <0.001 11.3 27.3 <0.001 All Stroke 5.5 6.1 0.57 9.5 8.9 0.67 New Permanent 8.5 6.9 0.17 11.8 10.3 0.29 Disabling Stroke 3.2 4.3 0.20 6.2 6.4 0.83 Pacemaker 0.9 0.4 0.17 3.7 2.3 0.09 0.4 0.0 0.05 1.4 0.6 0.09 TIA Re-intervention 0.0 0.0 NA 1.2 0.7 0.22 Endocarditis Leon et al. NEJM. 2016;374(17):1609-1620. Leon et al. NEJM. 2016;374(17):1609-1620. Unadjusted Time-to-Event Analysis Sapien 3 THV: Intermediate Risk Registry All-Cause Mortality and All Stroke (AT) 40 P2A Surgery All-Cause Mortality / Stroke Rate (%) SAPIEN 3 TAVR 30 20 18.8% 10.8% 9.7% 10 3.7% 0 0 3 6 9 12 Months from Procedure Number at risk: P2A Surgery 944 805 786 757 743 S3 TAVR 1077 1012 987 962 930 Thourani et al. 2016 ACC 7
Superiority Analysis Unadjusted Time-to-Event Analysis Components of Primary Endpoint (VI) All Stroke (AT) Favors Surgery Favors TAVR 40 P2A Surgery Weighted Difference -5.2% Superiority Testing Mortality SAPIEN 3 TAVR p-value < 0.001 Upper 2-sided 95% CI -2.4% 30 All Stroke (%) -10 -8 -6 -4 -2 0 2 4 6 8 10 20 Weighted Difference -3.5% Superiority Testing Stroke Upper 2-sided 95% CI -1.1% p-value = 0.004 10 8.2% 6.1% -10 -8 -6 -4 -2 0 2 4 6 8 10 4.6% 2.7% Weighted Difference +1.2% 0 Superiority Testing AR > Moderate Lower 2-sided 95% CI +0.2% p-value = 0.0149 0 3 6 9 12 Months from Procedure Number at risk: P2A Surgery 944 805 786 757 743 S3 TAVR 1077 1012 987 962 930 -10 -8 -6 -4 -2 0 2 4 6 8 10 Thourani et al. 2016 ACC SURTAVI: Noninferiority Analysis and Time-to-Event Curves CoreValve Evolution for the Primary End Point. CoreValve Evolut-R Evolut-Pro 2014 2015 2017 Reardon MJ et al. N Engl J Med 2017;376:1321-1331. 8
Improving outcomes with TAVR TAVR within Failed Bioprosthesis Torsten P. Vahl et al. JACC 2016;67:1472-1487 Self-expanding TAVR within Failed Surgical Balloon-expandable TAVR within Failed Bioprosthesis Surgical Bioprosthesis Deeb et al. JACC Cardiovasc Interv 2017;10(10):1034-1044 Webb et al. JACC 2017;69(18):2253-2262 9
What’s next? So where are we at now? Low surgical risk • Bicuspid aortic valve • Asymptomatic severe aortic stenosis • Moderate aortic stenosis with low ejection fraction • New transcatheter heart valves • SAVR versus TAVR Appropriate Use Criteria Estimated surgical risk • – STS risk scores – Frailty – Other risk factors Concomitant cardiac pathology • Anatomic and technical considerations • Other factors • Multidisciplinary Heart Valve Team 10
Looking ahead What’s going to happen to centers? Expansion of “TAVR centers” • Impact on cardiac surgical programs • Centers of excellence • TAVR Centers in United States TAVR Experience and Outcomes John D. Carroll et al. JACC 2017;70:29-41 2017 American College of Cardiology Foundation 11
Proliferation of transcatheter heart valves Conclusion TAVR has become an established therapy for aortic • stenosis TAVR is no longer excluded to “high surgical risk” patients • Choosing TAVR or SAVR is complex decision that • requires the integration of multiple factors Multidisciplinary Heart Team concept is becoming • increasingly important We are likely to see significant shifts on how centers and • programs function in the era of TAVR Torsten P. Vahl et al. JACC 2016;67:1472-1487 46 THANK YOU! 12
Recommend
More recommend