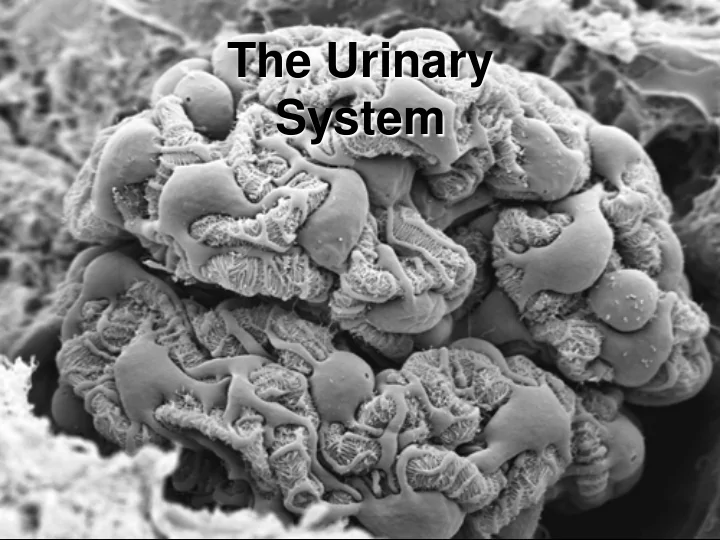
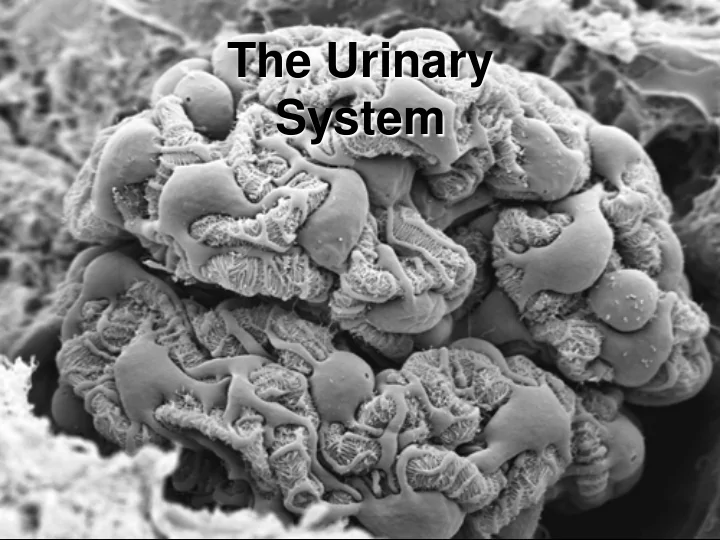
The Urinary System
The Urinary System • General Renal (kidney) Functions – Urine formation and concentration – Maintain the volume and composition of the ECF! – Eliminate toxins, metabolic wastes, and excess water out of the body • Main waste products produced are: – Urea – Uric acid – Creatinine – Hormone Production: • Calcitriol – derivative of Vit D3 that increases Ca2+ absorption by intestinal mucosa • Renin – regulation of blood pressure • EPO (erythropoeitin) – increases erythrocyte production produced by peritubular capillary endothelium
The Urinary System • Function of other urinary system components: – Ureters • Conduct urine from renal hilus to urinary bladder – Urinary Bladder • Store urine & involved in micturition – Urethra • Female: conduct urine from bladder to external environment • Male: conduct urine & semen to external environment
Organs of the Urinary System • Kidneys • Ureters • Urinary bladder • Urethra Figure 23.1a
Location and External Anatomy of Kidneys • Located in the retroperitoneal position • Lateral to T 12 –L 3 vertebrae • Average kidney – 12 cm tall, 6 cm wide, 3 cm thick • Hilus – on concave surface • Kidney surrounded by: – Renal capsule (dense irregular c.t.) – Adipose capsule – Renal fascia (continuous with the renal capsule)
Internal Anatomy of the Kidneys
Microscopic Anatomy of the Kidneys • Functional unit of the kidney = Nephron – Microscopic – approx 1.25 million/kidney equating to about 85 miles of tubules! – Nephron Components: • Vascular – renal corpuscle • Tubular – PCT, Loop of Henle (Nephron Loop), DCT • Tubovascular – Juxtaglomerular apparatus – Collecting Components: • Collecting Duct • Papillary Duct – Nephron + Collecting Components = Uriniferous Tubule (means tubule which conducts urine)
Mechanisms of Urine Production • Glomerular Filtration – filtrate of blood leaves kidney capillaries • Tubular Reabsorption – most nutrients, water, and essential ions reclaimed • Tubular Secretion – active process of removing undesirable molecules
Uriniferous Tubule Location Figure 23.4a
The Nephron • Renal corpuscle – glomerulus and glomerular capsule – Glomerulus – tuft of capillaries • Capillaries are fenestrated • Glomerular (Bowman’s) capsule – Parietal layer – simple squamous epithelium – Visceral layer – consists of podocytes
Renal Corpuscle and the Filtration Membrane
Renal Corpuscle and the Filtration Membrane • Large molecules are prevented from passing through the filtration membrane, due to fenestrations & filtration slits Negatively charged molecules are repelled by large anions in basement membrane
Tubular Section of Nephron • Filtrate proceeds to renal tubules from glomerulus – Proximal convoluted tubule – Loop of Henle (nephron loop) • Descending limb • Thin segment • Thick segment – Distal convoluted tubule
Tubular Section of Nephron Figure 23.4b
Classes of Nephron • Cortical nephrons – 85% of nephrons – Most of nephron is in the cortex of kidney • Juxtamedullary nephrons – 15% of nephrons – Extend deep into the renal pyramid & have long Loop of Henle – Responsible for urine concentration & dilution
Classes of Nephron Figure 23.9a
Collecting Tubules (Collecting ducts) • Collecting tubules – receive urine from distal convoluted tubules Figure 23.4a
Microscopic Blood Vessels • Nephrons are associated with several types of capillary beds: – Glomerulus – fed and drained by afferent & efferent arterioles – Peritubular capillaries – arise from efferent arterioles • Low-pressure, porous capillaries • Absorb solutes – Vasa recta – thin-walled looping vessels • Part of the kidney’s urine-concentrating mechanism
Summary of Blood Vessels Supplying the Kidney abdominal renal segmental Interlobar arcuate Interlobular afferent aorta artery arteries arteries arteries arteries arterioles 1 glomerular ~ 1,000,000 capillaries efferent arterioles peritubular capillaries & vasa recta 1 inferior vena renal Interlobar arcuate interlobular cava vein vein vein vein
Summary of Blood Vessels of the Kidney
The Tubovascular Component • Juxtaglomerular apparatus – Functions in the regulation of blood pressure • Vascular – afferent arteriole • Tubular - DCT • Juxtaglomerular cells of afferent arteriole – Act as mechanoreceptors – JGA cells secrete renin • Macula densa cells of distal convoluted tubule – Tall, closely packed epithelial cells – Act as chemoreceptors control vasodilation/vasoconstriction of afferent arteriole
Juxtaglomerular Apparatus Figure 23.11
Ureters • Carry urine from the kidneys to the urinary bladder • Oblique entry into bladder prevents backflow of urine • Histology of ureter – Mucosa – transitional epithelium – Muscularis – two layers • Inner longitudinal layer • Outer circular layer – Adventitia – typical connective tissue
Urinary Bladder • A collapsible muscular sac • Stores and expels urine – Full bladder – spherical • Expands into the abdominal cavity – Empty bladder • Lies entirely within Figure 23.14 the pelvis
Urinary Bladder • Urachus – closed remnant of the allantois • Prostate gland – in males – Lies directly inferior to the bladder – Surrounds the urethra Figure 23.15
Structure of the Urinary Bladder and Urethra Figure 23.17a
Structure of the Urinary Bladder and Urethra Figure 23.17b
Urethra • Epithelium – Transitional epithelium – near the bladder – Stratified and pseudostratified columnar – mid urethra – Stratified squamous epithelium – near the distal end • Internal urethral sphincter – involuntary smooth muscle • External urethral sphincter – voluntarily inhibits urination
Urethra • In females – length of 3–4 cm • In males – 20 cm in length – three named regions – Prostatic urethra – passes through the prostate gland – Membranous urethra – through the urogenital diaphragm – Spongy (penile) urethra – passes through the length of the penis
Micturition
Slides • Renal cortex • Cross section & long section through pyramids • Ureter • Urinary bladder • urethra
Renal cortex
Renal Pyramid (cs) Renal Papillae
ureter cross section
Urinary Bladder
Urethra (male)
Urethra (female)
Recommend
More recommend