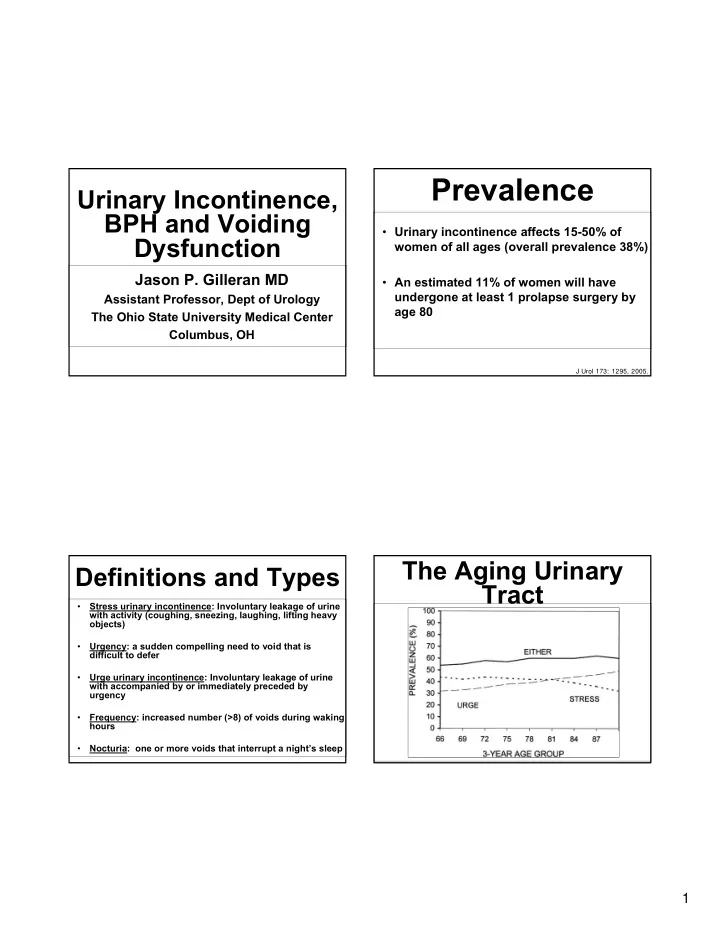
Prevalence Urinary Incontinence, BPH and Voiding • Urinary incontinence affects 15-50% of Dysfunction women of all ages (overall prevalence 38%) Jason P. Gilleran MD • An estimated 11% of women will have undergone at least 1 prolapse surgery by Assistant Professor, Dept of Urology age 80 The Ohio State University Medical Center Columbus, OH J Urol 173: 1295, 2005. The Aging Urinary Definitions and Types Tract Stress urinary incontinence: Involuntary leakage of urine • with activity (coughing, sneezing, laughing, lifting heavy objects) Urgency: a sudden compelling need to void that is • difficult to defer Urge urinary incontinence: Involuntary leakage of urine • with accompanied by or immediately preceded by urgency Frequency: increased number (>8) of voids during waking • hours Nocturia: one or more voids that interrupt a night’s sleep • 1
History Physical Exam • Duration of symptoms • Neurologic exam • Degree of incontinence (number of pads or • Digital rectal exam diapers) � Prostate enlargement (BPH) or • Degree of bother suspicious findings for cancer • Always important to look for and exclude • Female pelvic exam significant urinary tract pathology � Prolapsed bladder or urethral mass � Infection � Visible incontinence with coughing or straining � Blood in urine (hematuria) Laboratory Evaluation History • Urinalysis • Medications • Urine culture and sensitivity • Urine cytology � Diuretics • BUN, Creatinine • Prostate specific antigen (PSA) – consider • Fluid intake referral for: � Two consecutive levels above 4.0 ng/dL or � Total fluid intake any >10 ng/dL without setting of acute urinary retention � Caffeine and soda use � Enlarged prostate on exam with baseline PSA >1.6 AND urinary symptoms 2
Benign Prostatic Radiography Hyperplasia (BPH) • Usually of little help in assessment of • Non-invasive uroflowmetry incontinence or voiding dysfunction • Renal imaging if patient has: � Pressure-flow studies in select cases � Associated flank pain • Post-void residual (PVR) � Hematuria � Bladder scan � New onset renal insufficiency • Ultrasonography or CT scan � Straight catheterization � Bladder ultrasound pre-/post-void Benign Prostatic Medical Management Hyperplasia (BPH) • Alpha-blocker therapy • Histologic diagnosis � Tamsulosin (Flomax): 0.4 mg daily � Clinical finding on digital rectal exam is � Alfuzosin (Uroxatral): 10 mg daily benign prostatic enlargement (BPE) � Side effects: nasal congestion, orthostatic hypotension, decreased • AUA Symptom Score (IPSS) ejaculate � Bother score � Avoid PDE-5 inhibitors (Viagra, etc) within 6 hrs 3
Medical Management Behavioral Modification • 5- α -reductase Inhibitors • Fluid restriction � Finasteride (Proscar): 5 mg daily � 64 fluid ounces total (mostly water) � Dutasteride (Avodart): 0.5 mg daily • Diuretic use � Side effects: Hair growth, decreased � Timing (mid-day vs evening or AM libido dosing) • Herbal therapy • Caffeine intake • Timed Voiding � Saw palmetto Treatment of Urgency, Non-Invasive Options Frequency and Urge Urinary Incontinence 4
Caveats of Drug Medical Management Therapy Anticholinergic Therapy • May take 3-4 weeks to see full effect (>50% symptom improvement) • Contraindications: urinary retention, narrow angle glaucoma, gastroparesis • Watch for side effects � Dry mouth � Constipation Detrol, Detrol LA (tolterodine) Oxytrol (oxybutynin transdermal system) � Worsening dementia (elderly) 2 or 4 mg daily 3.9 mg twice weekly • Consider referral if symptoms not improved after 1-2 different anticholinergic medications More Antimuscarinic Other Pharmacology Agents • Amitriptyline (Elavil): 10-25 mg qhs • Ditropan XL (oxybutynin): 5 mg, titrate up to 30 mg daily • Vesicare (solifenacin) – 5-10 mg once daily • Imipramine (Tofranil): 75 mg qhs • Enablex (darfenacin): 7.5-15 mg once daily • Phenazopyridine (Pyridium): 100-200 • Sanctura (trospium chloride): 20 mg twice daily, once daily (Sanctura XR) available in mg tid x 3-4 days February 2008 5
Sacral Neuromodulation Treatment of Stress (InterStim TM ) Urinary Incontinence • FDA-approved 1997 for treatment of: � Chronic urgency and frequency � Refractory urge urinary incontinence � Non-obstructive urinary retention • Temporary placement of electrode in one (or occasionally both) S3 nerve roots • 2-3 week “test phase” � Implanatable generator (“pacemaker”) if >50% subjective and objective improvement Neuromodulator Pelvic Floor Physical Devices Therapy • Non-invasive means of improving pelvic floor muscles (Kegel exercises) • Often very successful in addressing mild incontinence in motivated and active women • Need specialized pelvic floor therapy referral 6
BULKING Summary AGENTS / INJECTION THERAPY • Always investigate for signs of more significant genitourinary pathology Before After • Empiric course of medical therapy and/or behavioral modification in idiopathic cases • Referral to specialist if no response to first Transurethral needle passage line therapy or other pathology detected Collagen (Contigen) Durasphere Coaptite Macroplastique Surgical Management Diagnosis and Management of Renal • Bladder neck suspension Calculi: Update for 2008 • Sling urethropexy • Artificial Urinary Sphincter Bodo E. Knudsen, MD FRCSC Director, OSU Comprehensive Kidney Stone Program � Designed for male Assistant Professor, Department of Urology incontinence secondary to post-prostate surgery 7
Overview Types of Stones • Calcium oxalate or phosphate – 70- • Initial presentation 80% • Imaging options • Uric acid – 5-10% • Treatment • Struvite – 5-15% � Watchful waiting • Cystine – 1% � Surgical options • Other (xanthine, drug related) Introduction Initial Evaluation • Complete medical history and • 5-15% of population develop renal physical exam calculi � Severe flank pain; may radiate to • Recurrent rate ≈ 50% groin • Primary care and specialists � Nausea and vomiting involved in ca � Lower urinary tract symptoms 8
Initial Evaluation Initial Evaluation • Urinalysis • Identify comorbidities � Microhematuria � Immunosuppressed � Nitrites/bacteria and/or leucocytes � Pregnant � Hexagonal crystals diagnostic of � Solitary kidney cystinuria • CBC � Renal insufficiency • Electrolytes and Cr Initial Evaluation Imaging Studies • Vitals • Unenhanced CT of abdomen and pelvis (CT stone study) � Febrile? • IVP • CVA tenderness • Abdominal tenderness • Ultrasound 9
Imaging – CT Scan Imaging – CT Scan • New “gold standard” • Fast, readily available • Only secondary signs of obstruction � Perinephric stranding � Hydronephrosis � Rim sign Imaging – CT Scan Imaging Studies - IVP • May identify other of pain • Previous gold standard but (appendix, aneurysm, bowel carried risk of contrast reaction problems, etc) • Useful for assessing obstruction • Most stones visualized including uric acid • Indinavir not visible 10
Imaging Studies - Imaging Studies - IVP Ultrasound Imaging Studies - Indications of Acute Ultrasound Intervention • Intractable pain or nausea/vomiting • Limited role • Renal failure • Pregnancy • Obstruction in a solitary kidney or bilaterally • Uric acid lithiasis • Obstruction in a transplant kidney • Follow up after surgery • Fever or urosepsis 11
Acute Intervention Watchful Waiting • Urine culture • Calculi ≤ 5 mm ≈ 50% chance they will pass spontaneously • Antibiotics � Factors to consider: • Pain control • # of stones � Narcotics • Level of stone � NSAIDS • History of prior spontaneous passage • Caution with renal insufficiency or • Time frame (may take up to 6 weeks to history of GI bleed pass) • Ureteral stent or nephrostomy tube • Degree of obstruction Medical Expulsion Treatment Options Therapy 1. Watchful waiting • Calcium channels blockers (nifedipine), corticosteroids, and alpha-blockers have � ± medical expulsion therapy been used 2. Shockwave lithotripsy • Best evidence currently for alpha-blockers 3. Ureteroscopy with laser lithotripsy � Tamsulosin (Flomax) 0.4 mg QD 4. Percutaneous nephrolithotomy • ?Improved pain control • May also be used to after shockwave 5. Open stone surgery lithotripsy Singh et al., Ann Emerg Med, 2007 12
Lithotomy Instruments of the Modern Stone Age 18th & 19th Centuries • Percutaneous approach (Johansson,1976) • ESWL (Chaussey, 1980) • Intracorporeal Lithotripsy (Alken, 1978) • Ureteroscopy (Perez-Castro, 1980) Treatment of Upper Urinary Tract Calculi Factors to Consider • Stone size • Location • Composition (if known) • Anatomic factors • Failure of other therapies • Renal function 13
Storz Modulith SLX F2 Shockwave Lithotripsy • Developed in early 1980’s by Dornier • Shockwave generated extracorporeal (F1) and targeted to stone (F2) • Stone fragments secondary to mechanical stresses and cavitation bubbles • 1 – 2% risk of perinephric hematoma • Risk of obstruction from fragments (Steinstrasse) • Longterm effects?? ESWL Contraindications Dornier HM-3 2007 � Uncorrected Bleeding Diatheses � Uncorrected Hypertension � Febrile UTI � Unfit for Anesthesia � Morbid obesity � Pregnancy � Proximate Calcified Aneurysms 14
Recommend
More recommend