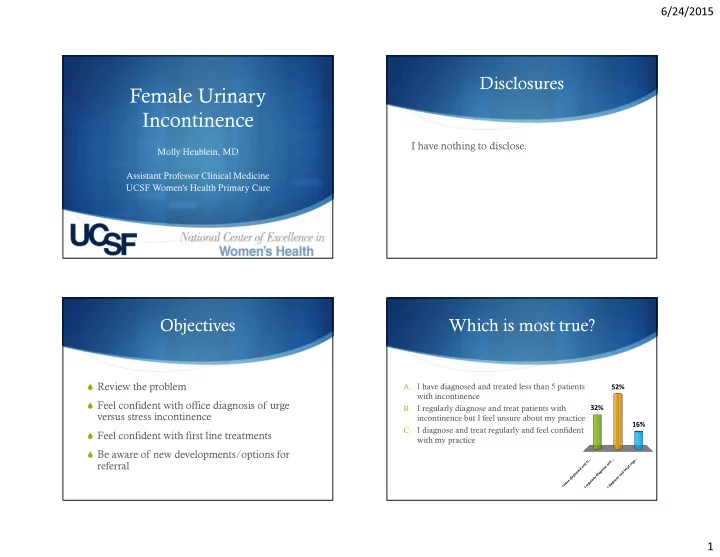
6/24/2015 Disclosures Female Urinary Incontinence I have nothing to disclose. Molly Heublein, MD Assistant Professor Clinical Medicine UCSF Women’s Health Primary Care � Objectives Which is most true? � Review the problem A. I have diagnosed and treated less than 5 patients 52% with incontinence � Feel confident with office diagnosis of urge I regularly diagnose and treat patients with 32% B. versus stress incontinence incontinence but I feel unsure about my practice 16% C. I diagnose and treat regularly and feel confident � Feel confident with first line treatments with my practice � Be aware of new developments/options for . . . . . . . . . r u t d g n e d n a r referral a e t s a d o e e n r s t o g d a n i n g d a a y i e d r l s a o e l n v u g a g a h e i r d I I I 1
6/24/2015 Female Urinary Incontinence If we don’t ask, they won’t tell � An estimated 20 million American women struggle with urinary incontinence- around 50% of middle aged � “Do you have any bothersome leakage of urine?” women, and 75% over the age of 75 1 � Projected costs for urge incontinence alone: $76.2 billion � Asking about bothersome symptoms increases treatment in 2015 in the US 2 rates 15% in the elderly 1 � It leads to lower quality of life scores � Urge incontinence increases risks for fractures and falls 3 � It really is a primary care problem! Female Urinary Incontinence Female Urinary Incontinence � Transient � Transient � Chronic � Chronic � Urge � Urge � Stress � Stress � Mixed � Mixed � Overflow � Overflow � Functional � Functional 2
6/24/2015 Urge Incontinence/Overactive Stress Incontinence (SUI) Bladder (UI/OAB) � Sphincter/pelvic floor � Detrusor muscle contracts more frequently/ at lower weakness gets stimulatory threshold and leakage occurs overwhelmed by increased abdominal � Women feel the urge to urinate, but lack control to pressure and leakage occurs hold it until the ideal time. � Symptoms occur with � Frequency and nocturia can occur cough, sneeze, laugh, exercise, or change in position. Picture from NIDDK: http://kidney.niddk.nih.gov/KUDiseases/pubs/uiwomen/index.aspx accessed 5/2015 Mixed Incontinence The basics…. � Both stress + urge Jan is a 66 year old overweight female with hyperlipidemia and low back pain who complains of � Focus on treating the more bothersome symptoms urinary leakage for several years, recently worsening. She leaks a few times per day and wears pads most of the time. She’s pretty bothered by her symptoms and wants to know what can be done to help. 3
6/24/2015 Female Urinary Incontinence � Jan reports that she usually leaks when she laughs or � Transient coughs. She has cut back on aerobic exercise because � Chronic jogging makes her leak too. She gets up to urinate once per night, and in the day, goes every 2 hours. � Urge � Stress � Mixed � Overflow � Functional Question: What is the next best Feel confident in your office step? diagnosis! 79% A. Refer Jan for post void residuals and � Basic questions have fair to good sensitivity and specificity in differentiating causes of incontinence 9 urodynamic testing to evaluate the cause � Post void residual are not needed 7 of her incontinence B. Diagnose her with urge incontinence � Neurologic testing adds little in a relatively healthy 15% outpatient without known neurologic disease C. Diagnose her with stress incontinence 6% 0% � Urodynamic testing does not improve outcomes for D. Order an MRI of her back to make sure conservative treatments (and it is controversial for surgical Diagnose her with stress... Refer Jan for post void re... Order an MRI of her back .. Diagnose her with urge i... her back pain and urinary incontinence is options) 8 not cauda equina syndrome 4
6/24/2015 The Sensitivity and Specificity of a Simple Test To Distinguish between Urge and Stress Urinary Incontinence 9 UI SI Sensitivity (95% 0.75 (0.68- 0.86 (0.79- CI) 0.81) 0.90) Specificity (95% 0.77 (0.69- 0.60 (0.51- CI) 0.84) 0.68) + Likelyhood 3.29 (2.39- 2.13 (1.71- ratio (95% CI) 4.51) 2.66) Neg Likelyhood 0.32 (0.24- 0.24 (0.16- ratio (95% CI) 0.43) 0.35) Free copy available at: http://coe.ucsf.edu/wcc/3questions.pdf Audience Question: Jan is diagnosed with stress incontinence, and treatment is initiated. The most effective initial treatment based on high quality evidence to suggest for her is: 93% A. A. Tolterodine (Detrol) once daily B. B. Mirabegron (Mybetriq) once daily C. C. Pelvic floor muscle training D. D. Intravesicular OnabotulinumtoxinA 5% 2% 0% (Botox) injections . . . . . . . . . . t . . q i o o i a r r b ) t t a o l e b e n r l O t y c e M s D u r ( a ( m l n u e o c n r i i r o s d g o e e o f l v r b a e a c r r i t t i v n o l M l e I T P . . D . B . A C 5
6/24/2015 Pelvic Floor Muscle Training Lifestyle modifications � Stress, urge and mixed all show >50% reduction in Fluid management - incontinence episodes compared to no treatment, number needed to treat 3 (NNT 6 for full continence) 1 Consideration of dietary factors - � Give a “Kegels Prescription” or refer to pelvic physical Timed voids - therapy. Handout available at: weight loss and exercise reduce incontinence episodes http://campuslifeservices.ucsf.edu/dmx/PatientEd/SDOB - in obese women (NNT 4) 1 G0030.pdf Bladder diaries alone can improve symptoms - significantly Pharmacologic Options: Stress No FDA approved treatments - off label duloxetine showed trend toward improvement - off label vaginal estrogens show trend toward improvement But neither has proven statistical significance Image from NIDDK: http://kidney.niddk.nih.gov/KUDiseases/pubs/diary/pages/page1.aspx (accessed 5/2015) 6
6/24/2015 Pharmacologic Options: Urge Pharmacologic Options: Urge Isabel is a healthy 70 year old woman. She had struggled with daily urge incontinence. She complains that she gets little warning before she gets a strong � Anticholinergics feeling of needing to pee, and sometimes can’t make it to the bathroom. Regular kegels, fluid management, and timed voids helped reduce her leakage to � Beta-3 adrenergic agonists about 5 episodes/day. She is still bothered enough to want to try more 68% treatment. What is the next best choice for therapy? A. Darifenacin (enablex) Mirabegron (Mybetriq) 32% B. C. Oxybutynin transdermal patch D. Any of the above 0% 0% ) ) e x q v e i . l r . . o b t b a e a l a n b m y e e h ( M e r n t ( d f c i n s o a n n o a y r n e g r f e t A i b n r i a a n D r y M i u t b y x Anticholinergics Anticholinergics � darifenacin (Enablex) ($290 branded only) � Side effects can be limiting � fesoterodine (Toviaz) ($250 branded only) � Limited effectiveness- all seem to have similar effects, NNT 7-9 for improvement in UI � oxybutynin (Ditropan) XL ($210 branded, $100 generic) � NNH with side effects 7-12 7 � solifenacin (Vesicare) ($290 branded only) � tolterodine (Detrol) ($240/mo generic, $320/mo branded) � trospium (Sanctura) ($200/mo branded only) Approximate monthly costs (data from uptodate.com 5/2015) 7
6/24/2015 Effects of Fesoterodine in Anticholinergics Vulnerable Elderly Subjects De Beau, et al. Journal of Urology 2014 � Continuation rates are only 12-40% at 1 year and 6-12% at 2 years across all drugs 10 Next line therapies urge: Mirabegron (Mybetriq) Jan has tried long acting oxybutynin but experienced excessive dry mouth. She tried tolterodine but did not experience � Novel class of treatment significant benefit in her symptoms. How should we next best � NNT 12 help her: 56% � More favorable side effect profile A. Recommend the best brand of incontinence supplies 23% � Safe to combine with anticholinergics B. Refer her for percutaneous tibial nerve 15% stimulation 6% � Cost is about $300/mo C. Refer her for incontinence surgery D. Refer her for pessary fitting g . . . . . . n a o c . i r e n t t b i n e f t a n s t y e u t i r c n a b o s r s e e c e h p n p t i r r d o o r o n f f f e r r r m e e e h h m h r r o e r e f e c e f e f e R e R R R 8
6/24/2015 Percutaneous Tibial Nerve Next line therapies: UI Stimulation � Neuromodulation: � Percutaneous Tibial Nerve Stimulators � Sacral Nerve Stimulator � OnabotuliniumtoxinA injections � Surgery is generally NOT an option for urge incontinence Picture from: Uroplasty Device Manufacturer https://www.uroplasty.com/patients/urgentpc SUmiT Trial SUmiT Results 11 Peters et al. Journal of Urology 2010 � S tudy of U rgent PC vs Sha m Effectiveness i n T reatment of Overactive Bladder Symptoms 9
6/24/2015 STEP trial STEP Trial � 50 participants who benefited from the active arm of SUmiT � Prospective monitoring � Tapered protocol to approximately once monthly PTNS over 3 years 12 Results of Sacral Neuromodulation Therapy for Urinary Sacral Nerve Stimulators Voiding Dysfunction: Outcomes of a Prospective, Worldwide Clinical Study Picture from webmd: http://www.webmd.com/urinary-incontinence-oab/ss/slideshow-overactive-bladder 10
6/24/2015 OnabotulinumtoxinA Image from urology patient information: http://www.camurology.org.uk/incontinence-treatment/ (accessed 5/2015) 11
Recommend
More recommend