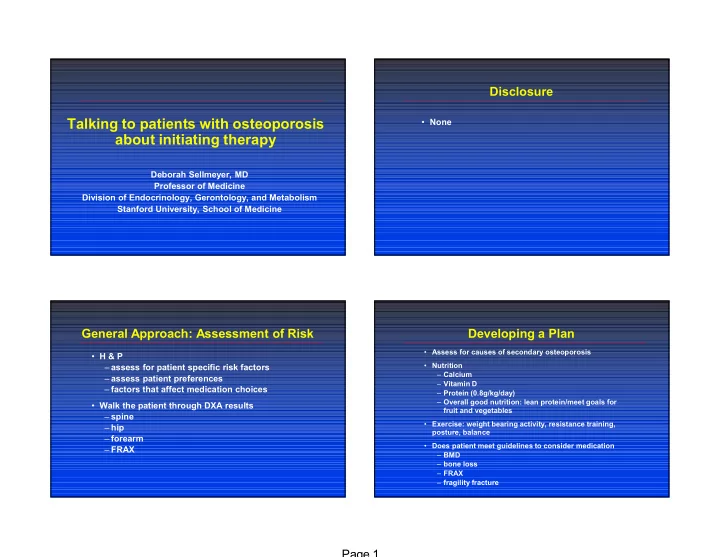
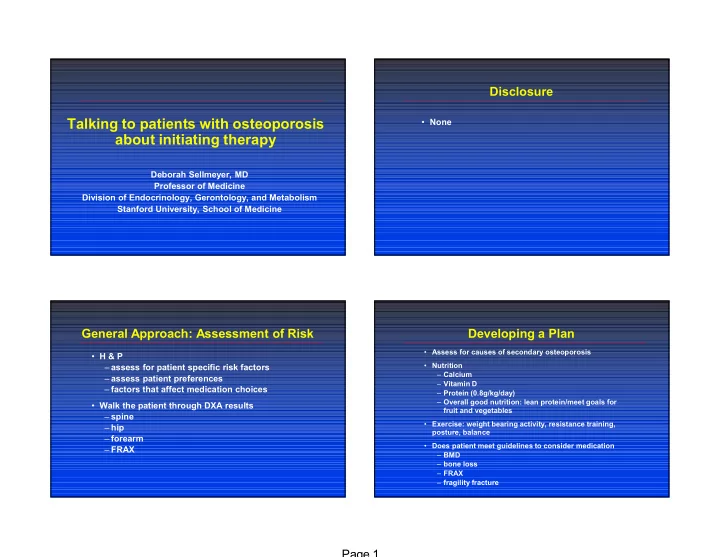
Disclosure Talking to patients with osteoporosis • None about initiating therapy Deborah Sellmeyer, MD Professor of Medicine Division of Endocrinology, Gerontology, and Metabolism Stanford University, School of Medicine General Approach: Assessment of Risk Developing a Plan • Assess for causes of secondary osteoporosis • H & P • Nutrition – assess for patient specific risk factors – Calcium – assess patient preferences – Vitamin D – factors that affect medication choices – Protein (0.8g/kg/day) – Overall good nutrition: lean protein/meet goals for • Walk the patient through DXA results fruit and vegetables – spine • Exercise: weight bearing activity, resistance training, – hip posture, balance – forearm • Does patient meet guidelines to consider medication – FRAX – BMD – bone loss – FRAX – fragility fracture Page 1
Medication Medication specifics • Need hip/non-spine protection • calcitonin – bisphosphonates – 25% spine fractures, no data for other fractures – denosumab – early agent—clinical trials less robust than other – anabolic options – 6% mild nose irritation • Risk limited to spine – calcitonin • raloxifene – raloxifene – 35% spine fractures, does not reduce fx at other sites • Particularly high risk/fractured on treatment – risk invasive breast CA – teriparatide – risk of thrombosis similar to OCP – abaloparatide – risk of death due to stroke in postmenopausal – romosozumab women with CAD • Glucocorticoids – hold for 72 hrs prior to air travel/immobility – bisphosphonate – hot flashes – denosumab – need to take continuously; no ONJ or AFF – teriparatide Medication specifics Medication specifics • Bisphosphonates • denosumab – fracture risk 50-60% spine, 40-50% hip – fracture risk 60% spine, 40% hip – Oral – skin side effects • rashes, eczema • ~20% of pts UGI side effects • <0.5% increased risk of serious skin infections • difficult to absorb: review dosing instructions – UTI risk may be increased – IV – similar risk of rare side effects to bisphosphonates • 25% acute phase reaction after 1 st dose • <0.5% risk of ONJ • may be reduced with acetaminophen pre-tx • 1:30,000 risk atypical fracture with long term treatment • mortality after hip fracture – unlike bisphosphonates, rapidly reversible – Both • need to receive doses on schedule • <0.5% risk of ONJ • need to change to bisphosphonate prior to medication holiday or use continuous therapy • 1:30,000 risk atypical fracture with long term treatment • protection after stopping—medication holidays Page 2
Medication specifics Case #1 • teriparatide/abaloparatide • 70 y/o woman, known low bone density for 8 years, – 70-80% reduction vert fxs concerned about medication side effects – 50% reduction non-vert fxs • No fractures – side effects: injection site reactions, hypercalcemia/uria, nausea, dizziness • No family history of osteoporosis or hip fracture • romosozumab • + celiac disease, on gluten free diet, + reflux, – 50% (vs. aln) - 70% (vs. pbo) reduction vert fx constipation – 20% reduction non-vert (vs. alendronate) • Consumes 2-3 servings Ca rich food/day – vascular risk (MI, CVA) • No difference vs. placebo (0.8% both groups) • Walks 10,000 steps/day • 2.0% romosozumab vs. 1.1% alendronate • Meds: Vit D 2000 IU, statin, H 2 blocker, ASA – one ONJ and one AFF (n>11,000) • PE: mild thoracic kyphosis Case #1 Case #1 • Nutrition: • DXA – Calcium: OK – Lumbar spine T-score -3.1 – Vitamin D: OK – Femoral neck T-score -2.0 – Protein: OK – Total hip T-score -1.6 – Gluten free: OK – FRAX hip fracture risk = 1.6% • Physical activity: • Recommendations? – Weight bearing activity: OK – Consider adding resistance activities – Exercise program to reduce kyphosis • Stand Tall: (415) 514-4816 or wellness@ptrehab.ucsf.edu • PT referral • Assess for secondary osteoporosis, ensure TTG IgA low • Vertebral imaging Page 3
Case #1: Medication? Case #1: Medication? • Meets guidelines for pharmacologic therapy based on • Meets guidelines for pharmacologic therapy based on lumbar spine T-score of -3.1 lumbar spine T-score of -3.1 • Options: • Options: – calcitonin – calcitonin • Vertebral imaging: no – raloxifene – raloxifene fractures • Labs normal, TTG IgA neg – oral bisphosphonate – oral bisphosphonate • Added resistance and – IV bisphosphonate – IV bisphosphonate posture training – denosumab – denosumab • Raloxifene – anabolic – anabolic Case #2 Case #2 • 60 y/o woman, low bone density dx 2009 • DXA • risedronate 2009-2011, stopped due to concern about side effects – Lumbar spine T-score -0.5 – Femoral neck T-score -2.5 • no fractures – Total hip T-score -1.9 • type 1 DM, insulin pump, A1C 7.8%, + nephropathy – FRAX: • frequent UTIs, one episode nephrolithiasis • Major osteoporotic fx: 11% • FH: maternal aunt kyphosis, ? vert fx • Hip fx: 2% • Meds: vitamin D 1000-2000 IU/day, calcium 500 mg bid, insulin, • Recommendations? ACE inhibitor • 1-2 servings calcium rich food/day • Body Pump class at gym three times/week • PE: unremarkable Page 4
Case #2 Case #2: Medication? • screen for causes of secondary osteoporosis • Meets guidelines for pharmacologic therapy based on femoral neck T-score of -2.5 – urine calcium 172 mg/24 hrs – serum Cr 0.78, eGFR 83 • FRAX estimated risk low – Ca 9.2, phos 3.7 – uses femoral neck BMD – PTH 53 – does not include DM as a risk factor • Nutrition: • Options: – calcium: high, decrease suppl to 500 mg/day – calcitonin – vitamin D: OK – raloxifene – protein: OK – oral bisphosphonate – glycemic control: review with diabetologist – IV bisphosphonate – denosumab • Physical activity: consider 30 mins walking on days not at the gym – anabolic Case #2: Medication? Case #3 • 88 y/o woman, known low bone density since 2001 • Meets guidelines for pharmacologic therapy • previously tried alendronate and risedronate— based on femoral neck T-score of -2.5 discontinued due to UGI symptoms • FRAX estimated risk low • no fractures – uses femoral neck BMD – does not include DM as a risk factor • no FH osteoporosis or hip fracture • Options: • PMH: GERD, CAD, HTN, arthritis, glaucoma • Increased weight bearing – calcitonin activity • meds: vitamin D 600 IU, calcium 500 mg, MVI, beta – raloxifene • Improve glycemic control blocker, eye drops – oral bisphosphonate • Hold on pharmacologic – IV bisphosphonate • participates in senior exercise class 2-3x/week therapy for now – denosumab • Assess DXA in one year • 1 serving calcium rich food/day – anabolic • PE: unremarkable Page 5
Case #3 Case #3 • DXA: • Nutrition: – Lumbar spine not available due to DJD – Calcium: prob OK, check calcium content of MVI – Femoral neck T-score -3.3 – Vitamin D: OK – Total hip T-score -2.4 – Protein: OK – 1/3 forearm T-score -4.2 – Review general goals for fruit/veg • Recommendations? • Physical activity: – Encouraged continued participation in Senior exercise classes – Fall prevention strategies • Assess for causes of secondary osteoporosis, particularly PTH given 1/3 forearm BMD Case #3: Medication? Case #3: Medication? • Meets guidelines based on femoral neck and 1/3 • Meets guidelines based on femoral neck and 1/3 forearm BMD values forearm BMD values • Options: • Options: – calcitonin – calcitonin • Labs: 25 OH vitamin D 28, – raloxifene – raloxifene PTH 63 – oral bisphosphonate – oral bisphosphonate • Increase vitamin D to 1500 – IV bisphosphonate – IV bisphosphonate IU/day • Needs agent with both – denosumab – denosumab spine and non-spine/hip – anabolic – anabolic protection • Denosumab—largest effect on 1/3 forearm BMD Page 6
Case #4 Case #4 • 59 y/o woman, low bone density since 2006 • DXA: – lumbar spine T-score -2.1 ( 6% over 2 years) • wrist fracture 2016 with fall from standing height – femoral neck T-score -2.8 ( 8% over 2 years) • hx breast CA, on aromatase inhibitor, 3 more years of tx – total hip T-score -2.2 ( 8% over 2 years) • GERD • Recommendations? • vegetarian, consuming 1 serving Ca fortified almond milk, 3-4 servings/day cruciferous vegetables • +FH osteoporosis: mother, no fractures • Meds: vitamin D 2000 IU, calcium 500 mg, aromatase inhibitor, H2 blocker • Torn meniscus—limited weight bearing activity • Tooth being watched, may need procedure/extraction • PE: unremarkable Case #4 Case #4: Medication? • Nutrition: • Meets guidelines for pharmacotherapy by BMD, also – Calcium: OK has ongoing bone loss – Vitamin D: OK • Needs to continue aromatase inhibitor – Protein: low—recommended increased protein to meet RDA of 0.8 g/kg/day • Possible dental procedure – Vegetarian/vegan: ensure B12 adequate • GERD • Physical activity: limited at present, recommended walking program and resistance exercises as able • Options: – calcitonin • Assess for causes of secondary osteoporosis, B12 level, 24 hour urine calcium, PTH – raloxifene – oral bisphosphonate • Follow up with dentist regarding need for dental work – IV bisphosphonate – denosumab – anabolic Page 7
Recommend
More recommend