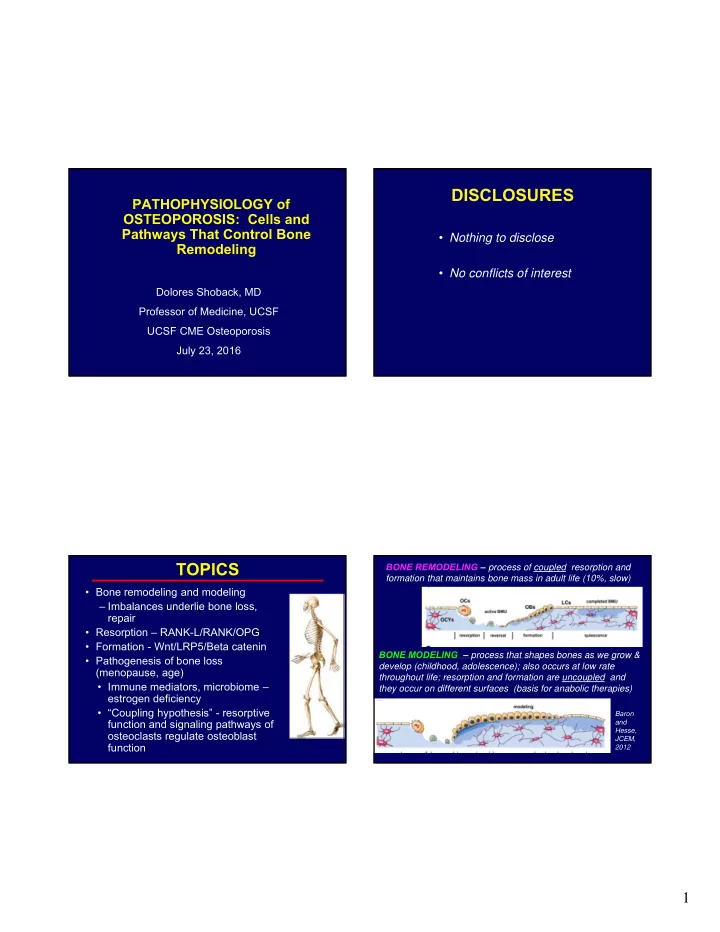
DISCLOSURES PATHOPHYSIOLOGY of OSTEOPOROSIS: Cells and Pathways That Control Bone • Nothing to disclose Remodeling • No conflicts of interest Dolores Shoback, MD Professor of Medicine, UCSF UCSF CME Osteoporosis July 23, 2016 TOPICS BONE REMODELING – process of coupled resorption and formation that maintains bone mass in adult life (10%, slow) • Bone remodeling and modeling – Imbalances underlie bone loss, repair • Resorption – RANK-L/RANK/OPG • Formation - Wnt/LRP5/Beta catenin BONE MODELING – process that shapes bones as we grow & • Pathogenesis of bone loss develop (childhood, adolescence); also occurs at low rate (menopause, age) throughout life; resorption and formation are uncoupled and • Immune mediators, microbiome – they occur on different surfaces (basis for anabolic therapies) estrogen deficiency • “Coupling hypothesis” - resorptive Baron function and signaling pathways of and Hesse, osteoclasts regulate osteoblast JCEM, function 2012 1
Microfracture Is Repaired through Why Do Bones Remodel? Targeted Remodeling Allows skeleton to -- Respond to mechanical loading (modeling) Repair microdamage (“wear and tear”) & prevent accumulation • Maintains “quality control” Segovia-Silvestre T et al, Hum Genet, 2009 Why Do Bones Remodel? Allows skeleton to -- RANK- • Respond to mechanical loading (modeling) • Repair microdamage (“wear and tear”) & prevent Ligand/RANK/Osteoprotegri accumulation n Pathway • Maintains “quality control” Release minerals (Ca and phosphate) & growth factors stored in matrix into circulation • Important in skeletal homeostasis (role in remodeling imbalance of age) 2
Osteoclastogenesis: Hormones, Growth Osteoprotegerin (OPG) Prevents RANK- Factors, Cytokines Stimulate Expression of L/RANK Interaction & Inhibits OC Activity RANK-L {RANK+RANK-L Interact} [OPG=Circulating Inhibitor ] CFU-M RANKL CFU-M Pre-fusion RANKL PTH Glucocorticoids Pre-fusion Osteoclast Osteoclast PGE 2 RANK RANK Vitamin D OPG Multinucleated X Osteoclast IL-11 Denosumab +mCSF does the Multinucleated IL-6 Osteoclast same thing IL-1 Hormones Growth PTHrP X Factors TNF- Cytokines Activated Activated Osteoclast Osteoclast Osteoblasts Bone Formation Osteoblasts & BM Stromal Cells Bone X Boyle WJ et al. Nature 2003;423:337; Hofbauer LC, Boyle WJ et al. Nature 2003;423:337 Bone Resorption Resorption Schoppet M. JAMA 2004;292:490 . OSTEOBLAST LINEAGE CELLS Bone-Formers Mesenchymal stem cells, pre-OB’s, mature OB’s, bone- lining cells, stromal cells, and osteocytes Bone Formation • Produce matrix and mineralize it – – Mechanical support LRP5/Wnt/ -Catenin – Matrix - reservoir of Ca, phosphate, growth factors, hormones – Secrete endocrine & paracrine factors – FGF23, DMP1, etc • Modulate development of tri-lineages of blood cells • Play role in metabolism , male reproduction Function and numbers of cells in OB lineage decline with aging – many factors responsible * 3
If no Wnt present, no signaling - β - Canonical Wnt Signaling catenin levels are LOW • Wnt signaling (OB, OB precursors) recruits IC protein Axin which moves to tail of LRP5/6 (because of interaction with Dvl ) • Complex forms, recruits FRAT1 and glycogen synthase kinase-3 β • Complex formation inhibits β - catenin phosphorylation NEW bone • Non-phosphorylated β -catenin formation accumulates in cytosol, goes to (quiescent & nucleus remodeling • β -catenin binds to LEF/TCF FINAL surfaces) elements and activates OB + OPG transcription program ( osteoprotegerin) • RSPO & norrin modulate Wnt Lewiecki et al, Nat Rev Rheumatol, 2011 Baron R, Kneissel M, Nat Med 2013 Sclerostin Secreted by Osteocytes Wnt Inhibition Negatively Regulates Bone Formation • WIF1 (Wnt inhibitory factor) or SFRP (secreted frizzled related protein) Sclerostin* sequester Wnt ligand Mesenchymal • then, Axin & APC stem cells Mature Pre-osteoblast associate with GSK-3 β Osteoblasts lining cells X X increase phosphorylation of β -catenin New bone • β -catenin~P ubiquinated proteasome for degradation Bone • NO bone made Osteocyte • Other inhibitors: N- cadherin inhibits • Loss of function mutations HIGH Ott SM. JCEM 2005; Semenov M, et al. LRP5/Wnt; sclerostin & bone mass JBC 2005; Semenov MV, et al. JBC DKK1 • Targeted therapy to neutralizing Scl 2006; Li X, et al. JBC 2005 Baron R, Kneissel M, Nat Med 2013 4
Menopause – Lose Estrogen • Remodeling increases, more BMU’s are formed, deeper resorption pits • Amount of bone formed - less than what was resorbed • Remodeling imbalance occurs (negative) - “uncoupling” Pathophysiology of Bone • With time - structural deterioration of bone Loss – Thinned trabeculi, decreased connectivity, perforations Lewiecki EM, Nat Rev Rheumatol , 2011 Gut Microbiome (Tella, Gallagher, J Ster Biochem Mol Bio , 2014) (Hernandez CJ et al, JBMR , 201 6) • Benefits the host – Vitamin production (many) – Extracts nutrients and energy from diet – “Metabolic function” (metabolites host) – Regulate immune system – Protects against pathogens getting in • How might they help the bone? • Enhance absorption of minerals (probiotics, prebiotics) • Estrogen present/therapy : dampens IL-1, TNF decreases IL-6, IL- • Enhance barrier function 11, GM-CSF, RANKL and mCSF; increased OPG • Enhance immune system (good or bad) • Estrogen deficiency/menopause : INCREASED TNF- α , IL-1; INCREASED release of IL-6, M-CSF, IL-11, GM-CSF, RANK-L A LOT OF EVIDENCE FOR MB INVOLVEMENT FOR stimulate OC’s/OC activity; DECREASED OPG, TGF- β BONE IN HUMANS IS INDIRECT 5
How the Gut MB Plays a Fundamental Role in Gut Microbiome Bone Mass Regulation (Igbal et al, JCI , 2016) (Steves et al, JBMR , 2015) • Billions of bacteria live in symbiosis with our bodies – influence health and disease • Gut MB host metabolic potential & innate & adaptive immune systems Aging Inflammation Disease Microbiome • Role in osteoporosis, OA, gout, RA, sarcopenia, frailty • Modified by probiotics (bacteria in food or dietary supplements) and prebiotics (usu complex CHO fibers in fruits/vegetables) Normal gut flora antigens (in MB) are presented to APC, T cells Pro-inflammatory cytokines made (ESTROGEN will normally dampen this, maintain barrier via gap junctions) Probiotics: Signal through APCs/T cells to reduce TNF- α , IL1- β , RANK- NO estrogen , these cytokines drive L; increase IL10 and OPG and Treg activity Increase TGF- β bone resorption systemically; barrier function May be “estrogen-like” molecules restore nl estrogen also reduced signaling and barrier function 6
Sex Steroid Deficiency (SSD) Associated Bone Mechanisms for Age-related Bone Loss - Loss Is Microbiota-Dependent and Prevented • Sex steroid def present (women, men) + nutritional issues by Probiotics (Li et al, J Clin Inv 2016) (Ca & vitamin D def, often secondary HPT, sarcopenia) • Intrinsic defects in marrow stromal cells with aging • Female mice (SSD) impaired proliferation & differentiation (“senescent OB’s”) – gut permeability, expanded TH17 cells (OC-genic pop. T cells) – osteoclastogenic cytokines in small intestine, marrow (TNF, RANK-L, IL-17) – Bone loss (micro-CT, histomorphometry, BTM’s) • These events don’t happen to mice kept under germ-free conditions. • Twice weekly treatment of SSD mice with probiotic – – Reduce/reverse trabecular bone boss (4 weeks after OVX) – No effects on cortical bone – Cytokines, T cell profiles are ones that “less pro-resorptive” More fat • Probiotics improve trabecular BMD in control mice • Several potential mechanisms postulated Khosla S, J Ger Med Sci, 2013 Age-related Osteoporosis Factors Released from Bone with Osteoclastic Resorption Sims NA, Ng KW, Curr Osteo Rep , 2014 • Imbalance in the bone formation response • IGF-1 to ongoing bone resorption • TGF- β • Bone as tissue “ages” – Promote bone cell proliferation, differentiation • Changes in material properties – affect – TGF- β and IGF-1 levels in strength – and in matrix components – bone fall with age affect constituents - released into IGF-1 IGF-1 – Bone matrix changes with microenvironment TGF- β TGF- β aging – May underlie reduced bone Is the problem only with osteoblasts? formation responses seen with Osteoclast lineage involved? aging in men and women 7
Coupling Factor Hypothesis (OC OB) - S1P/Rho GTPase Control of Osteoclast-Derived Factors Osteoblast Lineage Cells Sphingosine-1 PRE-OSTEOBLAST BMP6 Phosphate Wnt10b S1P RhoA GTPase OSTEOBLAST SCLEROSTIN OSTEOCLAST OSTEOCLAST Migration MSC/OSTEOBLAST Pederson et al. PNAS Chemotaxis Quint et al, JBC 2013; 105:20764, 2008 PRE-OSTEOCLAST (provided by MJ Oursler) TGF- β from OC Activity – TGF- β Released From Bone Influences Migration of OB Cells Matrix During Resorption Osteoblasts TGF- MSC LIF Leukemia inhibitory factor TGF- CXCL16 chemokine OSTEOCLAST Migration OSTEOBLAST Sites of Resorption Ota et al, Bone, 2013; Tang et al, Nat Med, 2009; Fracture Repair (provided by MJ Oursler) TGF- (provided by MJ Oursler) 8
Recommend
More recommend