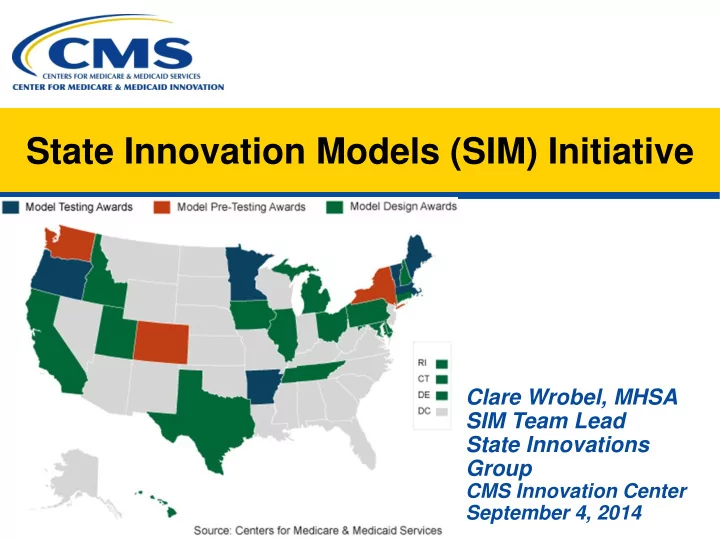
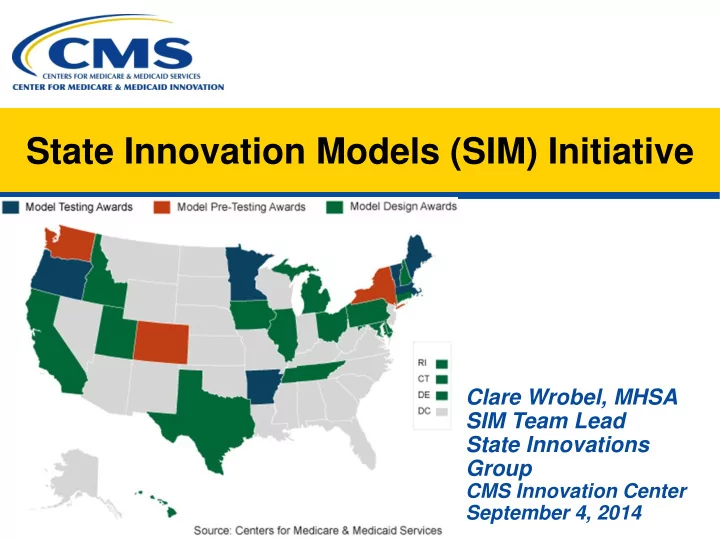
State Innovation Models (SIM) Initiative Clare Wrobel, MHSA SIM Team Lead State Innovations Group CMS Innovation Center September 4, 2014
CMS Innovations Portfolio Accountable Care Organizations (ACOs) Capacity to Spread Innovation • • Medicare Shared Savings Program (Center for Partnership for Patients Medicare) • Community-Based Care Transitions Program • Pioneer ACO Model • Million Hearts • Advance Payment ACO Model Health Care Innovation Awards (Rounds 1 & 2) • Comprehensive End-Stage Renal Disease (ERSD) Care Initiative State Innovation Models (Rounds 1 & 2) • Model Design Primary Care Transformation • • Model Test Comprehensive Primary Care Initiative (CPC) • • Maryland All Payer Model Multi-Payer Advanced Primary Care Practice (MAPCP) Demonstration Initiatives Focused on the Medicaid Population • Federally Qualified Health Center (FQHC) Advanced • Medicaid Emergency Psychiatric Demonstration Primary Care Practice Demonstration • • Medicaid Incentives for Prevention of Chronic Independence at Home Demonstration Diseases • Graduate Nurse Education Demonstration • Strong Start Initiative Bundled Payment for Care Improvement Medicare-Medicaid Enrollees • Model 1: Retrospective Acute Care • Financial Alignment Initiative • Model 2: Retrospective Acute Care Episode & • Initiative to Reduce Avoidable Hospitalizations of Post Acute Nursing Facility Residents • Model 3: Retrospective Post Acute Care • Model 4: Prospective Acute Care 2
State Innovation Model • CMS is testing the ability of state governments to utilize policy and regulatory levers to accelerate health transformation resulting in improved health, improved care and lower cost of care through a sustainable model of multi- payer payment and delivery reform
SIM Focus Areas EXPAND IMPROVE TRANSFORM VALUE BASED POPULATION HEALTHCARE PAYMENT HEALTH DELIVERY MODELS
SIM Mission The mission of the State Innovation Models Initiative (SIM) is to support states in designing and testing innovative care and payment models that will result in improved health, improved quality of care and lower costs • • Governor-led transformation Designed to reach the initiative preponderance of care • • Based on a comprehensive State Leverage federal resources, national Health Care Innovation Plan experts and technical assistance • Multi-payer commitment to value- contractors • based payment Ability to produce quantifiable results • Provider engagement in health care in improvements in quality, health transformation and cost • Population health improvement
SIM Round 1 – Where we are now • In Round 1 (began April 2012), CMS supported: – 6 Model Test states • Up to $45M over 3.5 years • Implementing innovative approaches to statewide multi-payer payment and service delivery transformation – 19 Model Design and Pre-Test States • Up to $3 million over 6-12 months • Developed State Healthcare Innovation Plans
Round 1 Model Design/Pre-Test States • California • New Hampshire • Colorado • New York • Connecticut • Ohio • Delaware • Pennsylvania • Hawaii • Rhode Island • Idaho • Tennessee • Illinois • Texas • Iowa • Utah • Maryland • Washington • Michigan
State Health Care Innovation Plans http://www.michigan.gov/documents/mdch/Michigan_Bl CA http://www.chhs.ca.gov/PRI/CalSIM%20State%20Healt MI ueprint_APPENDICES_REMOVED_454499_7.pdf h%20Care%20Innovation%20Plan_Final.pdf CO http://coloradosim.org/ship-final/ NH http://www.dhhs.state.nh.us/ocom/documents/nh-sim- plan.pdf http://www.healthreform.ct.gov/ohri/lib/ohri/sim/plan_doc https://www.health.ny.gov/technology/innovation_plan_i CT NY uments/ct_ship_2013_12262013_v82.pdf nitiative/docs/ny_state_health_innovation_plan.pdf http://www.healthtransformation.ohio.gov/LinkClick.asp DE http://dhss.delaware.gov/dhss/dhcc/cmmi/files/chooseh OH x?fileticket=WsSlPFly5GI%3D&tabid=138 ealthplan.pdf http://www.portal.state.pa.us/portal/server.pt/communit http://hawaiihealthcareproject.org/images/pdf/policy- HI PA y/department_of_health_information/10674/center_for_ papers/Hawaii%20Healthcare%20Innovation%20Plan_ medicare_and_medicaid_innovation_(cmmi)/1535774 February%202014.pdf http://www.healthcare.ri.gov/healthyri/resources/SHIPw ID http://healthandwelfare.idaho.gov/Portals/0/Medical/SHI RI ithAppendix.pdf P/IdahoSHIP.pdf http://www2.illinois.gov/gov/healthcarereform/Documents http://www.tn.gov/HCFA/forms/SHIP.pdf IL TN /Alliance/Alliance%20011614.pdf http://www.dhs.state.ia.us/uploads/IA%20SHIP%20Final. http://www.hhsc.state.tx.us/hhsc_projects/Innovation/pr IA TX pdf oposal.pdf http://health.utahsummit.com http://hsia.dhmh.maryland.gov/Documents/SIM%20Plan MD UT %20Final%20(compressed).pdf http://www.hca.wa.gov/shcip/Documents/SHCIP_Innov WA ationPlan.pdf
Round 1 Model Test States • Arkansas • Maine • Massachusetts • Minnesota • Oregon • Vermont
Arkansas What is the State testing? What is CMMI funding? • • Engaging primary care providers in Provider/payer infrastructure and patient-centered medical homes operational support for new care • Bundle payments for acute models • conditions Payment model design (episodes • Support providers with data, and Patient-Centered Medical technical assistance and learning Home (PCMH)) • system Funding for provider engagement • Program management, governance, and technical support
Arkansas Health Information Technology (HIT) State HIT Plans and Existing Infrastructures: • Medicaid Management Information System (MMIS): Core claims processing and payment system for Medicaid. • Enterprise Data Warehouse (EDW) – Storing data in a centralized location bring Department of Human Services (DHS) closer to the goal of full data integration. Arkansas Payment Improvement Initative (APII) Investments in existing and new HIT & Analytics infrastructures: • SHARE (State HIE) – Connecting large practices and hospitals serves as a key accelerant to HIT adoption and transformation in Arkansas. • Episode Analytics Engine • All Payer Claims Database Plus (APCD+) • Broadband Technology Opportunities Program (BTOP): • Provider Portal based data collection • PCMH Analytics Engine
Maine What is the State testing? What is CMMI funding? • Expanding PCMH, ACO’s and • Initiative support/governance Health Homes Structure (including personnel) • • Operate a public-private partnership Incentives for HIT adoption for to accelerate delivery system behavioral health providers • reform Quality measurement and • Align PCMH model with behavioral advanced data sharing, and health and long term delivery enhanced analytics • • Providing data/analytics Learning collaborative for providers
Maine HIT Examples Existing Infrastructure: • Maine Health Data Organization (MHDO) maintains health care utilization data on all patients in an inpatient, outpatient, and ER setting • The Maine Health Management Coalition (MHMC) will enable the development of data analytics capability for population health management. • HealthInfoNet (HIN) Ongoing SIM Investments: • Clinical “dashboard” • Statewide HIE Future Investments: • Maine is promoting efforts to encourage HIT among Behavioral Health (BH) providers.
Massachusetts What is the State testing? What is CMMI funding? • • Expand Primary Care Payment Design assistance and project Reform Initiative (MassHealth) management • • Data Infrastructure for LTSS Infrastructure support • • Establish a statewide patient Technical assistance to providers experiences of care measurement strategy
Massachusetts HIT Examples Ongoing investments in existing and new HIT & Analytics infrastructure: • Quality Data Repository/Clinical Data Repository (QDR/CDR) – Goal is to receive Quality Reporting Document Architecture (QRDA) data from provider EHRs via HIE, use quality data for payment reform, research and reporting, and make MMIS more “quality aware.” • HIE Technical Assistance to Behavioral Health and Long Term Services and Support providers • Electronic Referrals : – Goal is to enable providers to provide electronic referrals to community resources. • All Payer Claims Database (APCD) Provider Portal – Mass will utilize their APCD to enable providers to access claims-based reports for their entire patient panels with standard formats and timeframes.
Minnesota What is the State testing? What is CMMI funding? • • Broaden Medicaid ACOs to include Support for data analytics and behavioral health, long-term exchange • support services, and social Direct support to providers for services transformation • • Planning Accountable Communities Design Accountable Communities for Health for Health • • Transformation Center for rural Technical assistance to standardize primary care practices ACO metrics, payment methodologies
Minnesota HIT Examples Ongoing HIT Investments • Direct Gateway • Community Collaboratives e-health Grant Program • E-health Roadmaps • Privacy and Security Ongoing Data Analytics Investments • Integrated Health Partnership Program (IHP): expansion of Data analytics reporting and support for partners participating. • Analytic Infrastructure Enhancements • Technical Assistance on development and use of customized reports
Recommend
More recommend