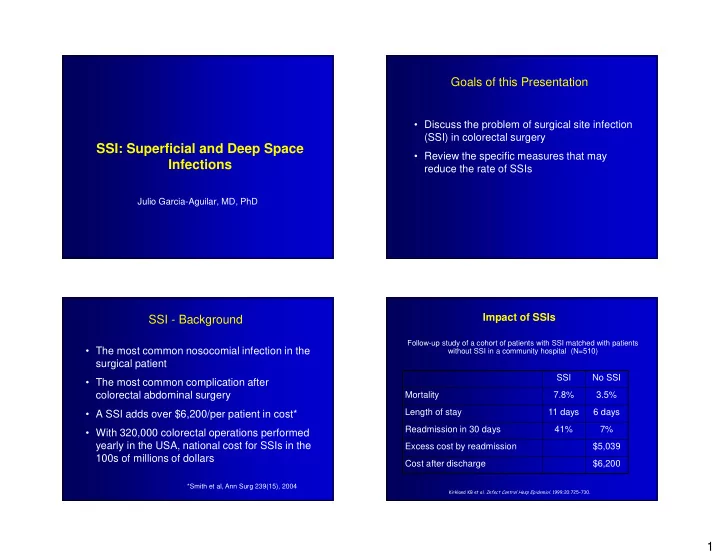
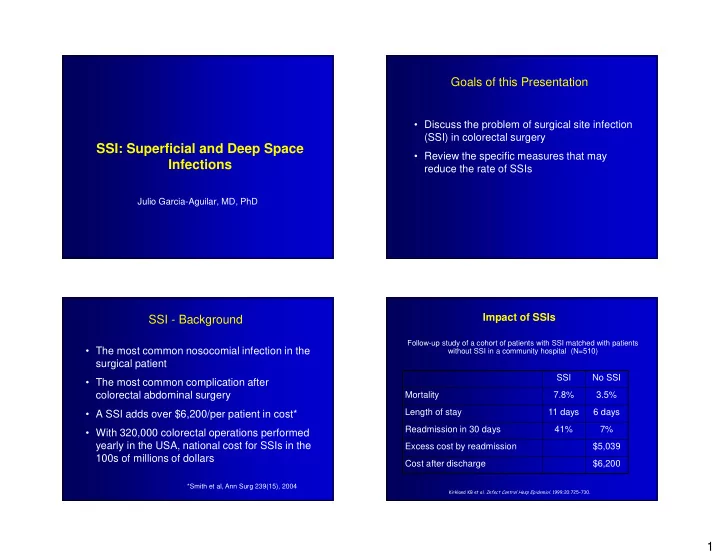
Goals of this Presentation • Discuss the problem of surgical site infection (SSI) in colorectal surgery SSI: Superficial and Deep Space • Review the specific measures that may Infections reduce the rate of SSIs Julio Garcia-Aguilar, MD, PhD Impact of SSIs SSI - Background Follow-up study of a cohort of patients with SSI matched with patients • The most common nosocomial infection in the without SSI in a community hospital (N=510) surgical patient SSI No SSI • The most common complication after colorectal abdominal surgery Mortality 7.8% 3.5% Length of stay 11 days 6 days • A SSI adds over $6,200/per patient in cost* Readmission in 30 days 41% 7% • With 320,000 colorectal operations performed yearly in the USA, national cost for SSIs in the Excess cost by readmission $5,039 100s of millions of dollars Cost after discharge $6,200 *Smith et al, Ann Surg 239(15), 2004 ������������������� ������������������������������� ����������� �!�� 1
SSI – Important Quality Indicator Hospital-Acquired Infections Included in the Value Based Purchasing Model Impacts the bottom line: Value Based Purchasing Model Measure Result Catheter-Associated Blood Stream 3/10 (compared to adjusted state rate Measure Final Score Rank Infection (CLABSI) Med-Surg ICU per 1000 line days) (higher is better: 0- (lower is better: N=90) 100%) Surgical Site Infection (Colon/GYN) 6/10 (compared to adjusted state rate per 100 procedures Hospital-Acquired 43% 61 Surgical Site Infection (Orthopedic) 4/10 (compared to adjusted state rate Infection average per 100 procedures) Mortality 100% 1 Complications not 89% 4 present on admission HCAHPS 60% 1 Overall Score 84% 2 Pathogenesis of SSI Most Important… • Human suffering Host • Distress • Inconvenience Bacteria • Delaying other treatments Surgery • Increase recurrence • Impact survival 2
Pathogenesis of SSI in Colorectal Surgery Surgical Site Infection (SSI) CDC Categories • Bacteria – 10 10 bacteria/gm feces • Host • Superficial Incisional : skin and subcutaneous tissue – cancer, IBD, radiation, steroids, immunomodulators, malnutrition, advanced age,… • Deep Incision: facial and muscle layers • Surgical site • Organ/space: any part of the anatomy, – open bowel other than the incision, opened during – stomas surgery – extensive dissections – more than one field – lengthy procedures – dead space in the pelvis Risk Stratification Wound Classification Risk Index Category (RIC) Nosocomial Infection Surveillance Study • I. Clean: uninfected, no inflammation, no cavities entered: Mastectomy, Thyroidectomy Components - 1 + 1 • II. Clean/Contaminated : respiratory, alimentary, ASA >3 genital, urinary tract entered in controlled conditions. Duration of > 180 min Cholecystectomy, Colectomy, Whipple, Laryngectomy, Urology Operation Wound 3,4 • III. Contaminated : Open accidental wounds, break in Classification sterile conditions, spillage, taking-down stomas. Appendicitis, Diverticulitis Laparoscopy Yes • IV. Dirty/Infected : Infection, perforation, devitalized tissue. (RIC ranges from –1 to +3) Abscess, Peritonitis, Enteric fistulas 3
Infection Rate by CDC Category Rates of SSI after colorectal surgery varies… N=751 patients – National Nosocomial Infection Surveillance (NNIS) 2004: 7.4% Superficial 11% • Am J Infect Control 2004 Deep 1.3% – Single institution retrospective review: 26% • Smith et al, Ann Surg 239(15), 2004 Organ Space 4.1% – Multi institutional prospective study: 28% to 43% TOTAL 16.4% • Itani et al, NEJM 355(25), 2006 Factors associated with SIS Variables associated with SSI Univariate analysis Variable p value p value Variable Odds Ratio Duration of surgery > 180’ 22% vs. 10% <0.001 Fisher’s exact test BMI > 30 kg/m 2 22% vs. 15% <0.05 Risk Index Category >2 2.03 0.026 RCI � 2 24% vs. 10% <0.05 Colon vs. Rectal surgery 18% vs. 11% <0.05 Duration of surgery > 180 Stoma creation 20% vs. 14% <0.05 2.41 0.007 minutes Glucose compliance 25% vs. 15% 0.06 Factors not associated: Diagnosis-IBD 21% vs. 14% 0.07 Age, Gender, Diabetes, ASA, Diagnosis, Surgeon, Pelvic vs. abdominal 20% vs. 15% 0.07 Hospital, Laparoscopy, Compliance with process measures Global compliance 20% vs. 15% 0.08 4
SSI Prophylaxis SSI Prophylaxis – General Measures Measures with Level 1 Evidence – Open wounds healed when possible • Eliminate S. aureus carriers – Patient free of infection • Hair removal • Skin antiseptics – Quit cigarette smoking • Mechanical bowel preparation (MBP) – Treat co-morbid conditions • Antibiotic prophylaxis – Optimize nutrition • Normothermia (Tem > 36 o C) – Surgical technique • Supplemental oxygen (80%) • bleeding, transfusion, hematoma, devitalized tissue • Glucose control (<200 mg/dl) • Intravenous fluid restriction S. aureus decontamination Hair Removal • Several prospective randomized trials and a • Nasal carriers of S. aureus have a higher risk of systematic review infection compared to non-carriers – Tanner et al, Cochrane Database Syst Rev 2006 • Treating carriers with Mupirocin nasal ointment may • Hair removal does not prevent wound infection. reduce the risk of SSI • If necessary, it should be done by clipping rather than shaving. • A recent RCT has proven that S. aureus decontamination reduces the risk of SSI by this • Depilatory cream also better than shaving organism by 60%. • Should be done immediately prior to the surgical incision • The risk reduction was more obvious in deep SSI (Bode, NEJM 2010) 5
Preoperative Skin Antisepsis Preoperative Skin Antisepsis Patients Personnel • Meta-analysis of 7 trials concluded that there • Barrier devices carried by operating personal is no evidence of benefit for preoperative have no impact on the risk of SSI bathing or showering with antiseptic solutions before surgery (Webster J and Osborne S, Cochrane • Hand-scrubbing with antiseptic soap and Database Syst Rev 2006) hand -rubbing with alcohol-based solution are • Clorhexidine-Alcohol is more effective than equally effective in reducing SSI (Parienti JJ et al, Povidone-Iodine for surgical prophylaxis in JAMA 2002) clean contaminated wounds. (Dorouiche et al, NEJM 2010) Mechanical Bowel Preparation (MBP) Mechanical Bowel Preparation (MBP) Reasons to do it Reasons to avoid it • Decrease of fecal flora burden • Poorly tolerated by some patients • Better bowel handling • Electrolyte imbalances / renal failure • Easier to palpate tumors • Increased bacterial translocation • Decrease fecal load proximal to anastomosis • Increases risk of intraoperative fecal spillage • Reduce risk of septic complications and leaks • Less physiologic for bowel mucosa • May increase surgical complications 6
Evidence Regarding MBP Evidence Regarding MBP Multiple RCT’s comparing MBP to no MBP show no Multiple recent RCT’s comparing MBP to no MBP difference, possibly fewer complications in no MBP show no difference, possibly fewer complications group in no MBP group Meta-Analyses show trend toward better outcomes with no MBP – Santos JCM, Br J Surg, 1994 n=149 MBP, � wound infn. – Bucher P, Arch Surg, 2004 (n=1297) – Burke P, Br J Surg 1994 n=169 No difference – Slim K, Br J Surg, 2004 (n=1454) – Miettinen R, DC & R, 2000 n=267 No difference – Wille-Jorgensen P, Colorectal Disease, 2005 (n=1592) – Zmora O, Ann Surg, 2003 n=380 No difference (also published as Cochrane Review) – Ram E, Arch Surg, 2005 n=329 No difference Wound Infection Rate: MBP vs No MBP Newer Studies on MBP Trend is also toward a lower SSI rate without MBP • Swedish study - 21 hospitals • 686 MBP, 657 no MBP • No difference in length of stay, CV complications or SSI • “MBP does not lower the complication rate and can be omitted before elective colonic resection” Jung B, et al Br J Surgery 2007 7
Recommend
More recommend