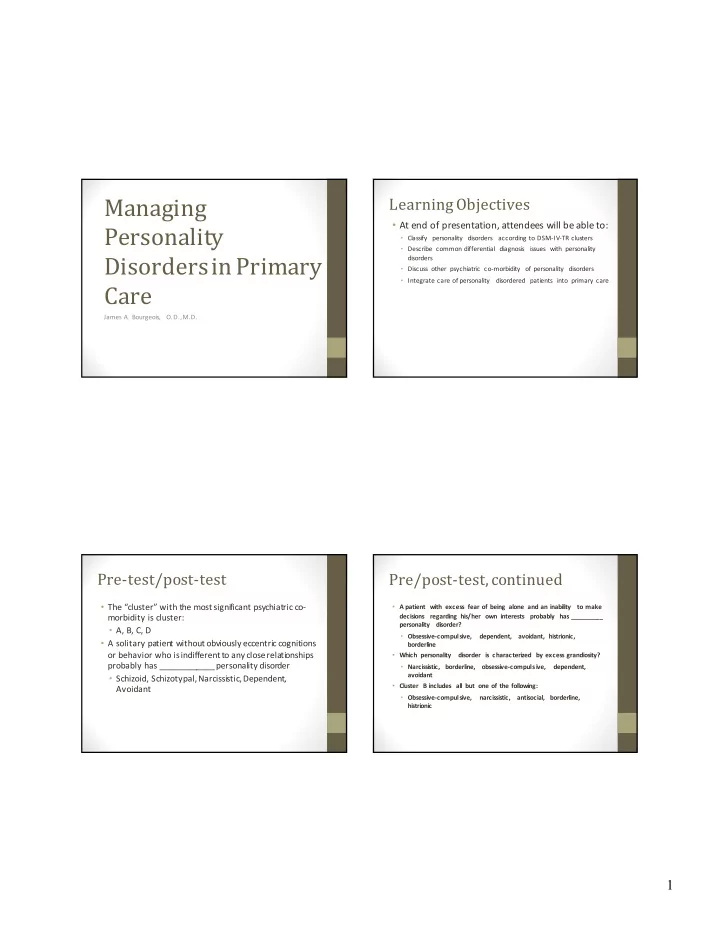
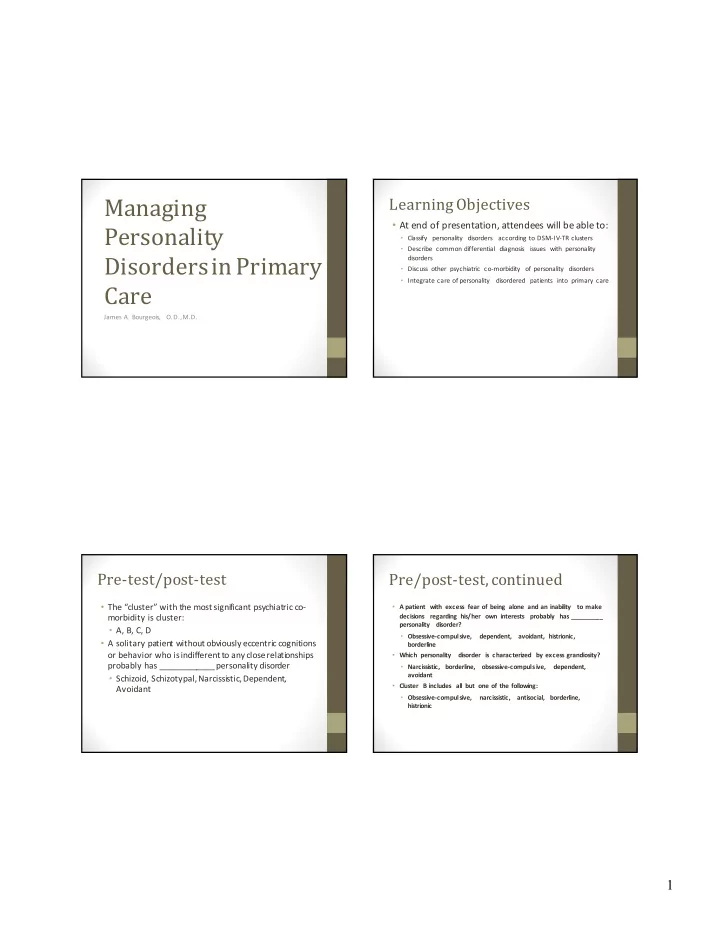
Managing Learning Objectives • At end of presentation, attendees will be able to: Personality • Classify personality disorders according to DSM-IV-TR clusters • Describe common differential diagnosis issues with personality Disorders in Primary disorders • Discuss other psychiatric co-morbidity of personality disorders • Integrate care of personality disordered patients into primary care Care James A. Bourgeois, O.D., M.D. Pre-test/post-test Pre/post-test, continued • The “cluster” with the most significant psychiatric co- • A patient with excess fear of being alone and an inability to make morbidity is cluster: decisions regarding his/her own interests probably has _________ personality disorder? • A, B, C, D • Obsessive-compulsive, dependent, avoidant, histrionic, • A solitary patien t without obviously eccentric cognitions borderline or behavior who is indifferent to any close relationships • Which personality disorder is characterized by excess grandiosity? probably has ____________ personality disorder • Narcissistic, borderline, obsessive-compulsive, dependent, avoidant • Schizoid, Schizotypal, Narcissistic, Dependent, • Cluster B includes all but one of the following: Avoidant • Obsessive-compulsive, narcissistic, antisocial, borderline, histrionic 1
General Considerations Classification, Coding • Enduring patterns of behavior • Axis II disorder (persistent, enduring) • Culturally dys-synchronous • Axis I refers to “episodic” illnesses • Cognition, affectivity, interpersonal functioning, impulse • Clusters A,B,C control • Personality disorder NOS • Not due to other psychiatric illness or substance abuse Cluster A Paranoid PDO 301.0 • Paranoid • Pervasive sense of distrust • Schizoid • 4/7 of: suspiciousness, preoccupation with others’ untrustworthiness, reluctant to confide, reads “threats” in • Schizotypal benign encounters, bears grudges, sensitive to attacks and • co-morbidity: Psychotic disorders quick to counter , suspicious of infidelity • Extremely rare in clinical populations 2
Paranoid PDO Schizoid PDO 301.20 • DfDx: Delusional Disorder , Schizophrenia • Detachment and restricted affect • Approach: T olerate suspiciousness, give thorough • 4/7 of: no desire for close relationships, solitary, hypo-sexual, explanations, respect privacy rigorously, allow to express anhedonia, no close friends, indifferent to feedback, doubts about care issues, build trust over time emotional coldness Schizoid PDO Schizotypal PDO 301.22 • DfDx: Avoidant PDO, Schizophrenia • Isolation, social anxiety, eccentricities, cognitive distortions, near-psychotic at baseline • Approach: T olerate reticence, expect social anxiety in conditions of “forced intimacy” (e.g., hospital admission), car e • 5/9 of: IOR, odd beliefs, unusual percepts, odd through a single trusted physician, build trust over time, relat e thinking/speech, suspiciousness, inappropriate affect, odd on a “fact” rather than “feeling” “currency” appearance/behavior , isolation, social anxiety 3
Schizotypal PDO Cluster B • DfDx: Schizophrenia (often a difficult distinction) • Antisocial • Approach: T olerate odd interactive style, may have a need for • Borderline “alternative” evaluation and therapy, tolerate anxiety in force d • Histrionic intimacy situations (as with schizoid PDO), relationship with one physician over time, psychotic decompensation likely • Narcissistic • Co-morbidity: Mood, anxiety (PTSD), eating (bulimia), dissociative, somatoform, substance abuse disorders • Extremely common in clinics Antisocial PDO 301.7 Antisocial PDO • DfDx: Borderline and Narcissistic PDO, ADHD • Disregard/violation of rights of others • Approach: Caution, expect dishonest reporting of symptoms, high • 3/6 of: unlawful behavior , deceitfulness, impulsivity, risk of malingering and litigious threats, interact with judicial irritability, disregard for safety, irresponsibility system, document thoroughly, rely on objective findings, don’t “go it alone” 4
Borderline PDO 301.83 Borderline PDO • Instability and chaos • DfDx: Broad but cases usually clear to experienced clinician • 5/9 of: frantic efforts to avoid abandonment, • Approach: Limit setting, stable relationship with one physicia n, idealization/devaluation, identity disturbance, impulsivity, limit doctor shopping, capitalize on “institutional suicidal behavior , affective instability, “emptiness,” anger dys- transference,” tolerate affects but confront unsafe behavior , control, transient paranoia or dissociation use extenders appropriately, limit phone contacts Histrionic PDO 301.50 Histrionic PDO • Excessive emotionality and attention seeking • DfDx: Borderline and Narcissistic PDO • 5/8 of: must be center of attention, seductive, shallow • Approach: Seek details, do not base therapeutic decisions on emotions, physical appearance to derive attention, complaints alone, as they are inevitably exaggerated, may be impressionistic speech, dramatic, suggestible, “pseudo- good placebo responders, confront behavior gently in the intimacy” “here and now” 5
Narcissistic PDO 301.81 Narcissistic PDO • Grandiosity, Grandiosity, Grandiosity • DfDx: Bipolar d/o, antisocial, borderline, histrionic PDO • “Legends in their own minds” • Approach: Very challenging patients who like to challenge y ou. As long as safe to do so, involve them in treatment decisions • 5/9 of: grandiose, fantasies of idealization, “specialness,” (“pseudo-colleague”), capitalize on entitlement by mobilizing requires excess admiration (“mirror-hungry”), entitlement, it in service of care, set limits on acting out exploitation, “hypo-empathic,” envy, arrogance Cluster C Avoidant PDO 301.82 • Avoidant • Social inhibition and inadequacy • Dependent • 4/7 of: social avoidance, reticent of involvement without reassurance, restraint within intimate relationships, • Obsessive-compulsive preoccupation with criticism, self-view as socially inept, • Comorbidity: anxiety and mood disorders, substance use reluctant to take risks disorders for avoidants with social phobia, eating d/o (avoidant and obsessive-compulsive) 6
Avoidant PDO Dependent PDO 301.6 • DfDx: Social phobia, Schizoid PDO • Failure of differentiation • Approach: Allow warm-up, tolerate oblique style of • 5/8 of: excess need for advice, deferential, inability to communication, more active role in interview disagree, lack of initiative, excess need for support, helpless when alone, urgently seeks new relationships, fear of being alone Obsessive-compulsive PDO Dependent PDO 301.4 • DfDx: Borderline and avoidant PDO • Preoccupation with order and control • Approach: Allow dependency but set limits, thorough use of • 4/8 of: detail preoccupation, perfectionism, “work-oholism,” extenders to “diffuse” dependency, groups of almost any sort over-conscientiousness,hoarding, reluctant to delegate, parsimonious, rigidity and stubbornness 7
Personality D/O NOS and Obsessive-compulsive PDO “Traits Only” • DfDx: OCD, Narcissistic PDO • For cases who are not a clear fit or for whom suspicion is greater than the available data • Approach: Expect to see articles, internet searches, data of all sorts; avoid feeling threatened, but appreciate the patient’s need for data more than emotional support, be quantitative, allow them control over treatment options where safe Psychiatric Referral Co-management • Dangerousness (suicidal, homicidal, psychotic) • Clear communication in both directions, patient must consent • Face-to-face meeting with psychiatrist/other MHP and • Diagnostic clarification primary care physician • Management of co-morbid psychiatric illness, • Other agencies very commonly involved including substance abuse • Psychopharmacologic consult - e.g., some newer literature suggests pharmacotherapy for personality disorders directly 8
Other considerations Summary/Questions • Many “high utilizers” are personality disordered patients • Discussion (often with other psychiatric co-morbidity) with significant dependency needs • Consider confronting utilization itself as a dependency behavior 9
Recommend
More recommend