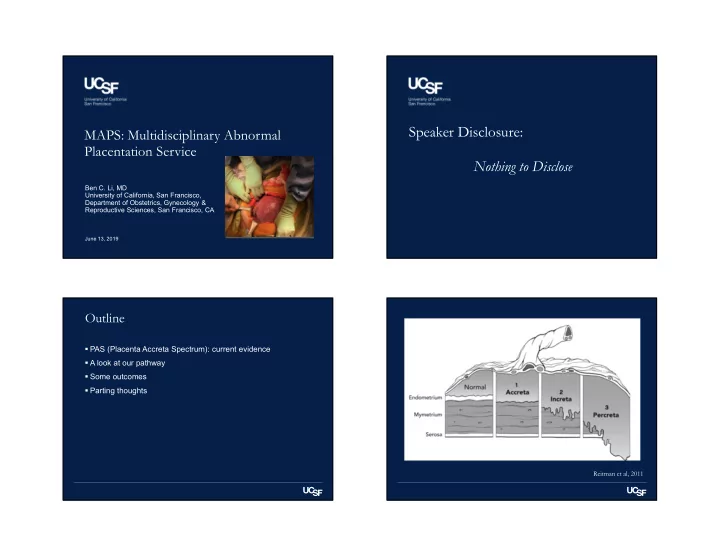
Speaker Disclosure: MAPS: Multidisciplinary Abnormal Placentation Service Nothing to Disclose Ben C. Li, MD University of California, San Francisco, Department of Obstetrics, Gynecology & Reproductive Sciences, San Francisco, CA June 13, 2019 Outline PAS (Placenta Accreta Spectrum): current evidence A look at our pathway Some outcomes Parting thoughts Reitman et al, 2011
Pathological Pathway Incidence of PAS • Scarring disrupts endometrium-myometrium junction It is increasing • Failure of normal decidualization in the area of a uterine scar 1970’s-1980’s: 1 in 2,500 to 4,000 1990’s-2000’s: 1 in 500 • Abnormally deep placental anchoring of villi and trophoblast infiltration 2016 National Inpatient Sample Study: 1 in 272 • Lack of a plane of cleavage between placental basal plate and uterus • Major hemorrhage; maternal and fetal morbidity Risk Factors Previous cesarean delivery Placenta previa (present in more than 80% of accretas in most large series)
Diagnosis of Placenta Accreta Spectrum: Diagnosis of Placenta Accreta Spectrum: US US
Diagnosis of Placenta Accreta Spectrum: Diagnosis of Placenta Accreta Spectrum: MRI MRI Heterogeneous placenta, placental bulge, dark inter placental Not superior to US but complementary bands, placental ischemic infarction, loss of retroplacental dark zone, myocetrial thinning, bladder wall interruption, focal When indicated: US equivocal, plan surgical approach exophytic mass, abnormal vascularization of the placental (hysterectomy or one-step conservative surgery) bed Knowledge of precise topography (superior vs inferior Signs not to be interpreted in isolation: observation of one is LUS, parametrical invasion) can alter surgical approach, likely to lead to detection of others ureteral stenting, vascular clamping or embolization Readers with > 5 y of experience in abdominal MRI MRI shown better to assess the depth of invasion re- demonstrated greater diagnostic accuracy and inter- classifying the extent of invasiveness in up to 30% of observer agreement patients Deep myoinvasion, adjacent organ invasion (increta/percreta) FIGO 2018: “MRI not essential but maybe useful” - Cesarean Hysterectomy Palacios Jaraquemada et al, 2005 Palacios Jaraquemada et al, 2005 Diagnosis of Placenta Accreta Spectrum: Diagnostic Studies Patients Sensitivity Specificity method n n % % US +/- MRI Ultrasound 23 3707 90.72 96.94 (overall) US first overall sensitivity 90.7%, specificity 96.9% (US neg no need for MRI) Placental 13 2725 77.43 95.02 lacunae US/MRI as complementary modalities, MRI better at topography and extent of invasion (most accurate after Loss of hypo 10 2633 66.24 95.76 24 w, exceptions) echoic space Improved results with experienced readers. Standardized Abnormalities reporting, collaborative approach: of uterus 9 2579 49.66 99.75 radiology/surgery/pathology to standardize terminology bladder and pathologic/surgical management interface Color Doppler 12 714 90.74 87.68 abnormalities D’Antonio et al, 2013
Principles of MAPS ACOG/SMFM Levels of Maternal Care Women with suspected PAS diagnosed in the antenatal period based on imaging or by clinical acumen should be delivered at a level III or IV center with considerable experience whenever possible to improve outcomes. FIGO consensus guidelines on placenta accreta spectrum disorders. IJOG 2018
Principles of MAPS Optimal management involves a standardized approach with a comprehensive multidisciplinary care team accustomed to management of PAS. • Obstetrician/Gynecologist • MFM • Gynecologic Oncologist • OB Anesthesiologist • Radiologist • Interventional Radiologist • Vascular Surgeon • Urologist • Intensivist • Neonatologist • Blood Bank • Cell Saver Principles of MAPS Delivery at 34 0/7-35 6/7 weeks of gestation is suggested as the preferred gestational age for scheduled cesarean delivery or hysterectomy absent extenuating circumstances in a stable patient. Earlier delivery may be required in cases of persistent bleeding, preeclampsia, labor, rupture of membranes, fetal compromise, or developing maternal comorbidities.
(Apply patient label) (Apply patient label) Morbidly Adherent Placenta (MAPS) Patient Checklist (to be completed in OR, prior to Pre-Op Team huddle (ideally to be completed day before surgery) induction of anesthesia) Surgical plan Date/time of surgery: ________________ Most recent Hct _______Date: _________ Patient positioning: ❑ Lithotomy ❑ Supine Location: ❑ L&D ❑ Main OR #_________ Skin incision: ❑ Pfannenstiel ❑ Vertical Blood products in OR? ❑ Yes ❑ N/A GA at time of surgery: ________________ Placenta plan: ❑ Remove ❑ Leave in place Diagnosis: ICN Set Up/Ready? ❑ Yes ❑ N/A Uterus: Planned C hyst? ❑ Yes ❑ No ❑ Accreta ❑ Increta ❑ Percreta Tubal if no hys? ❑ Yes ❑ No ❑ N/A Pathology Requisition Concern for involved organs/areas? Special equipment needed? ❑ No ____________________________________ ❑ Yes:___________________________________ Specimen Dissection Instructions Level of concern: ❑ 3-way foley ❑ hyst tray ❑ cysto ❑ stents (directed by radiologist): ❑ Low ❑ Medium ❑ High ❑ Other:________________________________ ❑ Axial Plane ❑ Sagittal Plane (to be completed immediately post-op, Personnel Also note: ❑ If portion of urinary bladder wall Nursing/OR Staff before leaving OR) resected en bloc w/ uterus & Primary surgeon: _____________________ Main OR staff notified? ❑ Yes ❑ if uterine serosa intact upon entering the Gyn Onc surgeon: _____________________ Planned scrub tech: ❑ L&D ❑ Main OR abdomen, prior to any surgical manipulation Back Up ❑ Scrubbed In ❑ Ancillary services Contact number: ___________________ Post-Op Cell saver notified? ❑ Yes Anesthesiologist: _____________________ Urology aware? ❑ Yes Radiologist: __________________________ Interventional Rad:_____________________ Contact: _____________________________ Disposition: Vascular aware? ❑ Yes ❑ ICU ❑ L&D ❑ Ante ❑ Postpartum Anesthesia Plan Contact: _____________________________ Type of anesthesia: ___________________ ICU aware? ❑ Complications? ❑ Yes ________________ IV access/lines: _______________________ ICN aware? ❑ Yes I&O/Products received: Special equipment needed? ❑ Belmont? Patient EBL: ________ UOP: ________ IVF: ______ Other:____________________________ Healthcare proxy: ________________________ Blood products (# of units to be prepared) PRBC: ________ FFP: _______ Cryo: _____ Contact: _____________________________ DO NOT REMOVE FROM CHART PRBC: ____ FFP: _____ Plt: ______ Cryo: ____ Patient aware of all plans: ❑ Yes SMFM. Placenta accreta. Am J Obstet Gynecol 2010. Principles of MAPS Although ultrasound evaluation is important, the absence of ultrasound findings does not preclude a diagnosis of PAS; thus, clinical risk factors remain equally important as predictors of PAS by ultrasound findings.
Uterine Artery Embolization Following Cesarean Delivery but Prior to Hysterectomy In Press Principles of MAPS Parting thoughts The role of preoperative placement of catheters or balloons into pelvic arteries for potential PAS incidence is increasing interventional radiologic occlusion is controversial. C/S and placenta previa are greatest risk factors Iliac artery occlusion has been reported to Multidisciplinary team approach (including patient) decrease blood loss in some but not all case series. A small randomized controlled trial also Optimal management involves a standardized approach showed no benefit. with a comprehensive multidisciplinary care team accustomed to management of PAS Because serious complications such as arterial damage, occlusion, and infection may occur, routine use is not recommended.
Thank you!
Recommend
More recommend