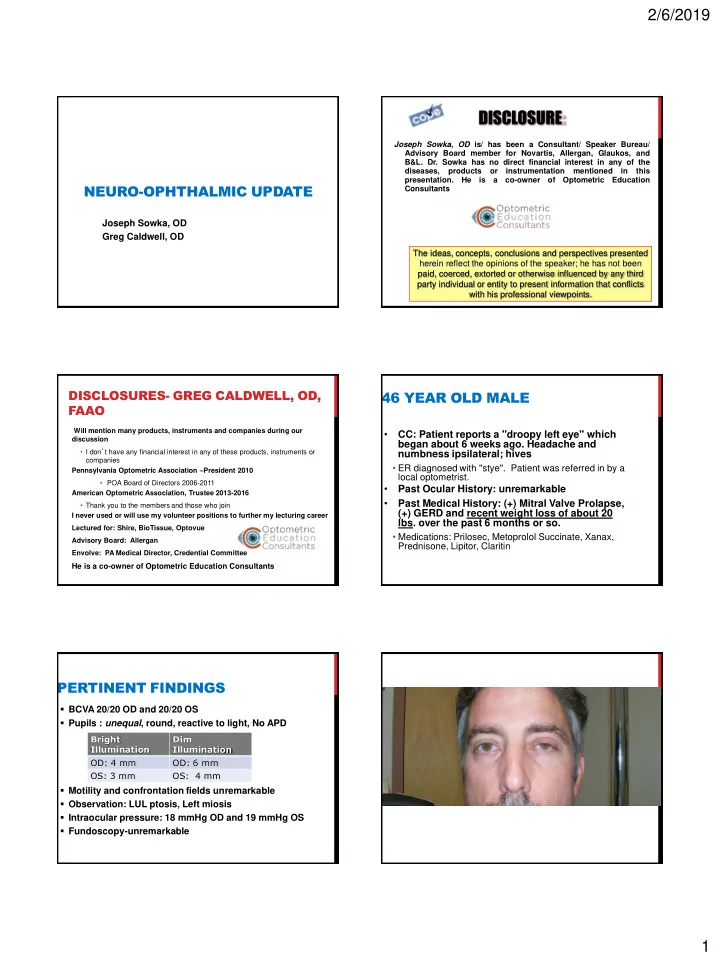
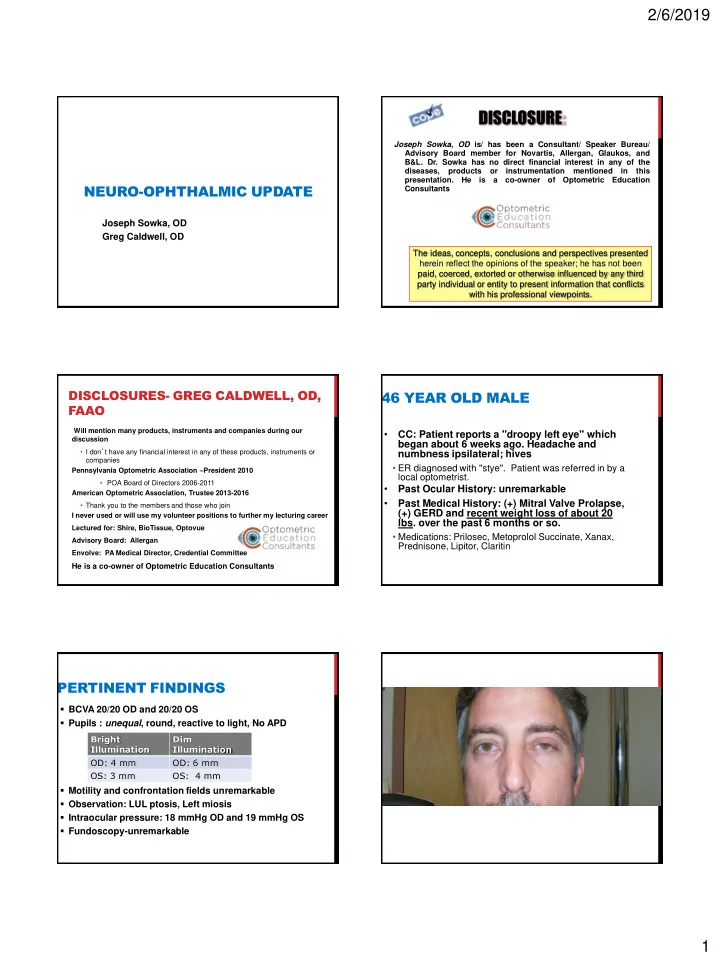
2/6/2019 DISCLOSURE: Joseph Sowka, OD is/ has been a Consultant/ Speaker Bureau/ Advisory Board member for Novartis, Allergan, Glaukos, and B&L. Dr. Sowka has no direct financial interest in any of the diseases, products or instrumentation mentioned in this presentation. He is a co-owner of Optometric Education NEURO-OPHTHALMIC UPDATE Consultants Joseph Sowka, OD Greg Caldwell, OD The ideas, concepts, conclusions and perspectives presented herein reflect the opinions of the speaker; he has not been paid, coerced, extorted or otherwise influenced by any third party individual or entity to present information that conflicts with his professional viewpoints. DISCLOSURES- GREG CALDWELL, OD, 46 YEAR OLD MALE FAAO Will mention many products, instruments and companies during our • CC: Patient reports a "droopy left eye" which discussion began about 6 weeks ago. Headache and • I don ’ t have any financial interest in any of these products, instruments or numbness ipsilateral; hives companies • ER diagnosed with "stye". Patient was referred in by a Pennsylvania Optometric Association – President 2010 local optometrist. • POA Board of Directors 2006-2011 • Past Ocular History: unremarkable American Optometric Association, Trustee 2013-2016 • Past Medical History: (+) Mitral Valve Prolapse, • Thank you to the members and those who join (+) GERD and recent weight loss of about 20 I never used or will use my volunteer positions to further my lecturing career lbs. over the past 6 months or so. Lectured for: Shire, BioTissue, Optovue • Medications: Prilosec, Metoprolol Succinate, Xanax, Advisory Board: Allergan Prednisone, Lipitor, Claritin Envolve: PA Medical Director, Credential Committee He is a co-owner of Optometric Education Consultants PERTINENT FINDINGS BCVA 20/20 OD and 20/20 OS Pupils : unequal , round, reactive to light, No APD Bright Dim Illumination Illumination OD: 4 mm OD: 6 mm OS: 3 mm OS: 4 mm Motility and confrontation fields unremarkable Observation: LUL ptosis, Left miosis Intraocular pressure: 18 mmHg OD and 19 mmHg OS Fundoscopy-unremarkable 1
2/6/2019 POST-IOPIDINE So, what do you think and what do you want to do now? HORNER’S SYNDROME Pre-Iopidine Etiology unclear based upon exam Headache, neuralgia and ‘hives’ - Not consistent with cluster migraine • Dx of exclusion, not convenience Post-Iopidine - Hives- not consistent with HZO Unexplained weight loss concerning- relationship unclear Recommend medical eval by PCP - Additional testing dictated by PCP results DISCUSSION What is Horner’s Syndrome? • a triad of clinical signs arising from disruption of sympathetic innervation to the eye and ipsilateral face that causes miosis , upper lid ptosis , mild elevation of the lower lid, and anhydrosis of the facial skin. 2
2/6/2019 PHARMACOLOGICAL TESTING HORNER’S SYNDROME: ETIOLOGIES First-order neuron disorder: Stroke (e.g., • Cocaine vertebrobasilar artery insufficiency or infarct); tumor; multiple sclerosis (MS), and, rarely, • Horner’s pupil doesn’t dilate, normal pupil does severe osteoarthritis of the neck with bony • Hydroxyamphetamine (Paredrine) spurs. • Differentiates post- from pre-ganglionic • Not available and doesn’t matter because bad stuff happens everywhere Second-order neuron disorder: Tumor (e.g., lung • carcinoma, metastasis, thyroid adenoma, Apraclonidine 0.5% (Iopidine) neurofibroma). Patients with pain in the arm or • Denervation suprasensitivity scapular region should be suspected of having a • 36-72 hours from onset Pancoast tumor. In children, consider • Horner’s pupil dilates, normal doesn’t neuroblastoma, lymphoma, or metastasis. • Reversal more classic and diagnostic that cocaine MANAGEMENT HORNER’S SYNDROME: ETIOLOGIES • Third-order neuron disorder: Headache syndrome • Localizable- targeted workup (e.g., cluster, migraine, Raeder paratrigeminal • Neck and facial pain- carotid dissection syndrome), internal carotid dissection, herpes zoster • Facial paraesthesia- middle cranial fossa disease virus, otitis media, Tolosa – Hunt syndrome, neck • Necessary Work Up (non-localizable): trauma/tumor/inflammation, prolactinoma. • MRI of brain, orbits and chiasm with and without contrast, • Congenital Horner syndrome: Trauma (e.g., during attention to middle cranial fossa. delivery). • MRA of head and neck-rule out carotid dissection • Facebook tomography • MRI of neck and cervical spine, include lung apex and brachial plexus • Other rare causes: Cervical paraganglioma, ectopic • Horner’s syndrome patient needs to be imaged from chest to head - 3 cervical thymus scans • Horner’s protocol • All imaging in patient unremarkable CAROTID DISSECTION CAROTID DISSECTION A 3rd- order Horner’s and ipsilateral head, Carotid artery dissection presents with the eye, or neck pain of acute onset should sudden or gradual onset of ipsilateral neck or be considered diagnostic of internal hemicranial pain, including eye or face pain carotid dissection unless proven Often associated with other neurologic findings otherwise. including an ipsilateral Horner’s syndrome, TIA, stroke, anterior ischemic optic neuropathy, subarachnoid hemorrhage, or lower cranial nerve palsies - 52% with ocular or hemispheric stroke with 6 days • 67% within first week; 89% within 2 weeks; none after 31 days Horner’s from suspected carotid dissection should go to ER 3
2/6/2019 HORNER SYNDROME ALGORITHM RULE 1. Confirm it is Horner syndrome - Apraclonidine; dilation lag Diagnosing Horner’s 2. Determine if accidental or surgical trauma syndrome is insufficient. as cause You must try to ascertain 3. Urgent imaging a cause and never - CT/CTA; MRI/MRA head and neck if present< 2 weeks assume that it is benign. 4. Image lung apex CASE: 59 BF Long time patient presents for her glaucoma f/u. She reports drooping in the right eye and smaller pupil for about 1 month. Symptoms were noticed at/ about time of dx of lung cancer and subsequent surgery. - `She also reports scapular pain and weakness in the right hand. Past Medical History: (+) Lung Cancer, (+) Pancreatitis, (+) HTN and (+) Acid Reflux Social History: Smokes 1 pack per day for 45 years, Drinks a 6 pack of beer daily CASE: PERTINENT FINDINGS PANCOAST TUMOR CONTINUED… A Pancoast tumor is a lung cancer arising in the apex of the lung that involves structures of the apical chest wall. Treatment • Pharmacological testing not done • Chemotherapy • Radiation Therapy • New onset of ptosis and miosis with • Surgery: lobectomy vs. wedge resection dx lung cancer and h/o recent lung Prognosis: 5 year survival rate is around 30% • surgery Not an emergency • Dx=Pancoast Syndrome 4
2/6/2019 ODE TO HORNER’S SYNDROME 80 YEAR OLD MAN When the lid is low and the pupil small, Reports a sudden loss of vision OD Check to see the sweat don’t fall. Vision is count fingers at 2 feet OD and 20/25 Cocaine is no longer universal, OS Iopidine will cause reversal. APD OD grade 4 You have to scan head to chest, Fundus photos OU And remember that MRA is best. Pain in association, will surely cause commotion. Send to the ER without correction, Remember, it might be carotid dissection. Joseph Sowka, OD CRAO TREATMENT/WORK- UP/FOLLOW-UP? PHOTOS OU weeks ❌ 🆙 Anterior chamber paracentesis (less than 24 hours) STAT blood work - 2-10% of all CRAOs are caused by thrombosis from Giant Cell Arteritis (GCA) - Sed-rate - C-reactive protein • Qualitative or quantitative? - CBC with diff Monitor for neovascularization, every 3-6 CRAO, BRAO, TIA (AMAUROSIS 35 YEAR OLD MAN FUGAX) Wants another opinion due to “ hemorrhage Acute Stroke Ready Hospital on my right eye ” - Certification recognizes hospitals that meet standards to support better outcomes for stroke care as part of a stroke system of care - Developed in collaboration with the Joint Commission (TJC), eligibility standards include: Happened 3 days ago after vomiting - Dedicated stroke-focused program - Staffing by qualified medical professionals trained in stroke care - Relationship with local emergency management systems (EMS) that encourages training in field assessment tools - Claims food poisoning from chicken Caesar salad and communication with the hospital prior to bringing a patient with a stroke to the emergency department - Access to stroke expertise 24 hours a day, 7 days a week (in person or via telemedicine) and transfer agreements with facilities - Still feels a little nauseated that provide primary or comprehensive stroke services. - 24/7 ability to perform rapid diagnostic imaging and laboratory testing to facilitate the administration for IV thrombolytics in Saw ophthalmologist 3 days ago, told he had eligible patients - Streamlined flow of patient information while protecting patient rights, security and privacy - Use of data to assess and continually improve quality of care for stroke patients a bruise on his eye and it should go away in Warn hospital is suspicion for GCA 1-2 weeks 20% of stroke or heart attack within 3 years However of those who experienced CVA or MI - 80% were within 24-48 hours; those remaining - 50% occurred in 2 weeks - Majority within the next 90 days Not PCP, not retinologist, just the Acute Stroke Ready Hospital! 5
Recommend
More recommend