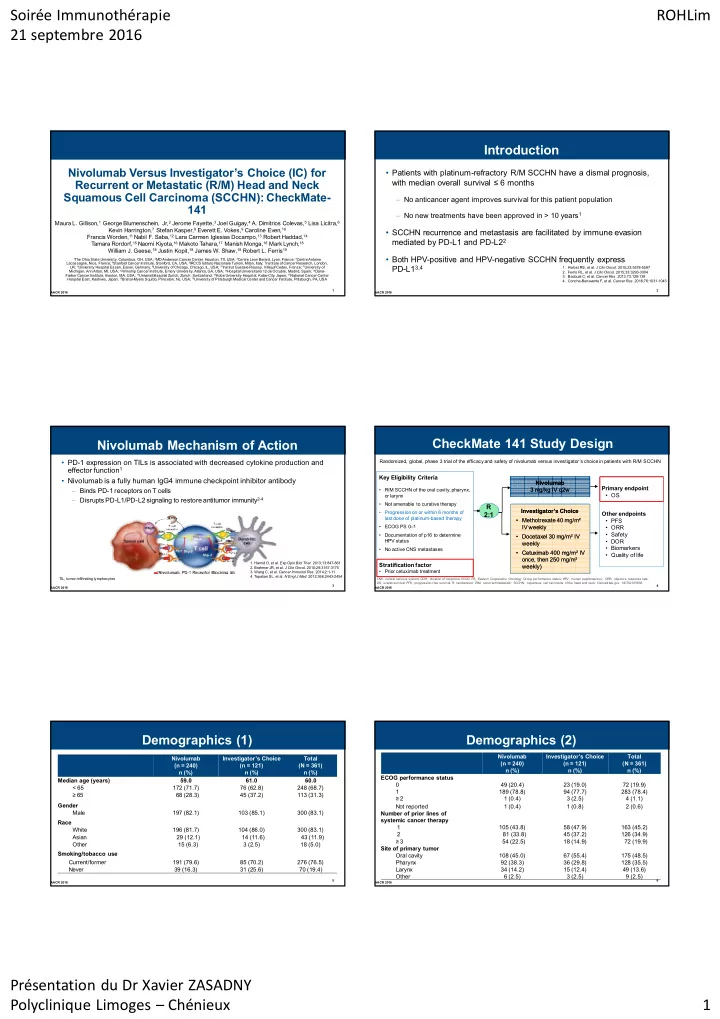
Soirée Immunothérapie ROHLim 21 septembre 2016 Introduction Nivolumab Versus Investigator’s Choice (IC) for • Patients with platinum-refractory R/M SCCHN have a dismal prognosis, Recurrent or Metastatic (R/M) Head and Neck with median overall survival ≤ 6 months Squamous Cell Carcinoma (SCCHN): CheckMate- – No anticancer agent improves survival for this patient population 141 – No new treatments have been approved in > 10 years 1 Maura L. Gillison, 1 George Blumenschein, Jr, 2 Jerome Fayette, 3 Joel Guigay, 4 A. Dimitrios Colevas, 5 Lisa Licitra, 6 Kevin Harrington, 7 Stefan Kasper, 8 Everett E. Vokes, 9 Caroline Even, 10 • SCCHN recurrence and metastasis are facilitated by immune evasion Francis Worden, 11 Nabil F. Saba, 12 Lara Carmen Iglesias Docampo, 13 Robert Haddad, 14 mediated by PD-L1 and PD-L2 2 Tamara Rordorf, 15 Naomi Kiyota, 16 Makoto Tahara, 17 Manish Monga, 18 Mark Lynch, 18 William J. Geese, 18 Justin Kopit, 18 James W. Shaw, 18 Robert L. Ferris 19 • Both HPV-positive and HPV-negative SCCHN frequently express 1 The Ohio State University, Columbus, OH, USA; 2 MD Anderson Cancer Center, Houston, TX, USA; 3 Centre Leon Berard, Lyon, France; 4 Centre Antoine Lacassagne, Nice, France; 5 Stanford Cancer Institute, Stanford, CA, USA; 6 IRCCS Istituto Nazionale Tumori, Milan, Italy; 7 Institute of Cancer Research, London, PD-L1 3,4 UK; 8 University Hospital Essen, Essen, Germany; 9 University of Chicago, Chicago, IL, USA; 10 Institut Gustave Roussy, Villejuif Cedex, France; 1 1 University of 1. Herbst RS, et al. J Clin Oncol . 2015;23:5578-5587 Michigan, Ann Arbor, MI, USA; 12 Winship Cancer Institute, Emory University, Atlanta, GA, USA; 13 Hospital Universitario 12 de Octubre, Madrid, Spain; 14 Dana- 2. Ferris RL, et al. J Clin Oncol . 2015;33:3293-3304 Farber Cancer Institute, Boston, MA, USA; 15 Universitätsspital Zurich, Zurich, Switzerland; 16 Kobe University Hospital, Kobe-City, Japan; 17 National Cancer Center 3. Badoual C, et al. Cancer Res . 2013;73:128-138 Hospital East, Kashiwa, Japan; 18 Bristol-Myers Squibb, Princeton, NJ, USA; 19 University of Pittsburgh Medical Center and Cancer Institute, Pittsburgh, PA, USA 4. Concha-Benavente F, et al. Cancer Res . 2016;76:1031-1043 1 2 AACR 2016 AACR 2016 CheckMate 141 Study Design Nivolumab Mechanism of Action • PD-1 expression on TILs is associated with decreased cytokine production and Randomized, global, phase 3 trial of the efficacy and safety of nivolumab versus investigator’s choice in patients with R/M SCCHN effector function 1 Key Eligibility Criteria • Nivolumab is a fully human IgG4 immune checkpoint inhibitor antibody Nivolumab Nivolumab Primary endpoint – Binds PD-1 receptors on T cells • R/M SCCHN of the oral cavity, pharynx, 3 mg/kg IV q2w 3 mg/kg IV q2w • OS or larynx – Disrupts PD-L1/PD-L2 signaling to restore antitumor immunity 2-4 • Not amenable to curative therapy R R Investigator’s Choice Investigator’s Choice • Progression on or within 6 months of 2:1 2:1 Other endpoints last dose of platinum-based therapy • Methotrexate 40 mg/m² • Methotrexate 40 mg/m² • PFS • ECOG PS 0–1 IV weekly IV weekly • ORR • Safety • Documentation of p16 to determine • Docetaxel 30 mg/m² IV • Docetaxel 30 mg/m² IV HPV status • DOR weekly weekly • Biomarkers • No active CNS metastases • Cetuximab 400 mg/m² IV • Cetuximab 400 mg/m² IV • Quality of life once, then 250 mg/m² once, then 250 mg/m² 1. Hamid O, et al. Exp Opin Biol Ther. 2013;13:847-861 Stratification factor weekly) weekly) 2. Brahmer JR, et al. J Clin Oncol. 2010;28:3167-3175 • Prior cetuximab treatment 3. Wang C, et al. Cancer Immunol Res. 2014;2:1-11 4. T opalian SL, et al. N Engl J Med. 2012;366:2443-2454 TIL, tumor-infiltrating lymphocytes CNS, central nervous system; DOR, duration of response; ECOG PS, Eastern Cooperative Oncology Group performance status; HPV, human papillomavirus; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; R, randomized; R/M, recurrent/metastatic; SCCHN, squamous cell carcinoma of the head and neck; Clinicaltrials.gov. NCT02105636. 3 4 AACR 2016 AACR 2016 Demographics (1) Demographics (2) Nivolumab Investigator’s Choice Total Nivolumab Investigator’s Choice Total (n = 240) (n = 121) (N = 361) (n = 240) (n = 121) (N = 361) n (%) n (%) n (%) n (%) n (%) n (%) ECOG performance status Median age (years) 59.0 61.0 60.0 0 49 (20.4) 23 (19.0) 72 (19.9) < 65 172 (71.7) 76 (62.8) 248 (68.7) 1 189 (78.8) 94 (77.7) 283 (78.4) ≥ 65 68 (28.3) 45 (37.2) 113 (31.3) ≥ 2 1 (0.4) 3 (2.5) 4 (1.1) Gender Not reported 1 (0.4) 1 (0.8) 2 (0.6) Male 197 (82.1) 103 (85.1) 300 (83.1) Number of prior lines of systemic cancer therapy Race 1 105 (43.8) 58 (47.9) 163 (45.2) White 196 (81.7) 104 (86.0) 300 (83.1) 2 81 (33.8) 45 (37.2) 126 (34.9) Asian 29 (12.1) 14 (11.6) 43 (11.9) ≥ 3 54 (22.5) 18 (14.9) 72 (19.9) Other 15 (6.3) 3 (2.5) 18 (5.0) Site of primary tumor Smoking/tobacco use Oral cavity 108 (45.0) 67 (55.4) 175 (48.5) Current/former 191 (79.6) 85 (70.2) 276 (76.5) Pharynx 92 (38.3) 36 (29.8) 128 (35.5) Never 39 (16.3) 31 (25.6) 70 (19.4) Larynx 34 (14.2) 15 (12.4) 49 (13.6) Other 6 (2.5) 3 (2.5) 9 (2.5) 5 6 AACR 2016 AACR 2016 Présentation du Dr Xavier ZASADNY Polyclinique Limoges – Chénieux 1
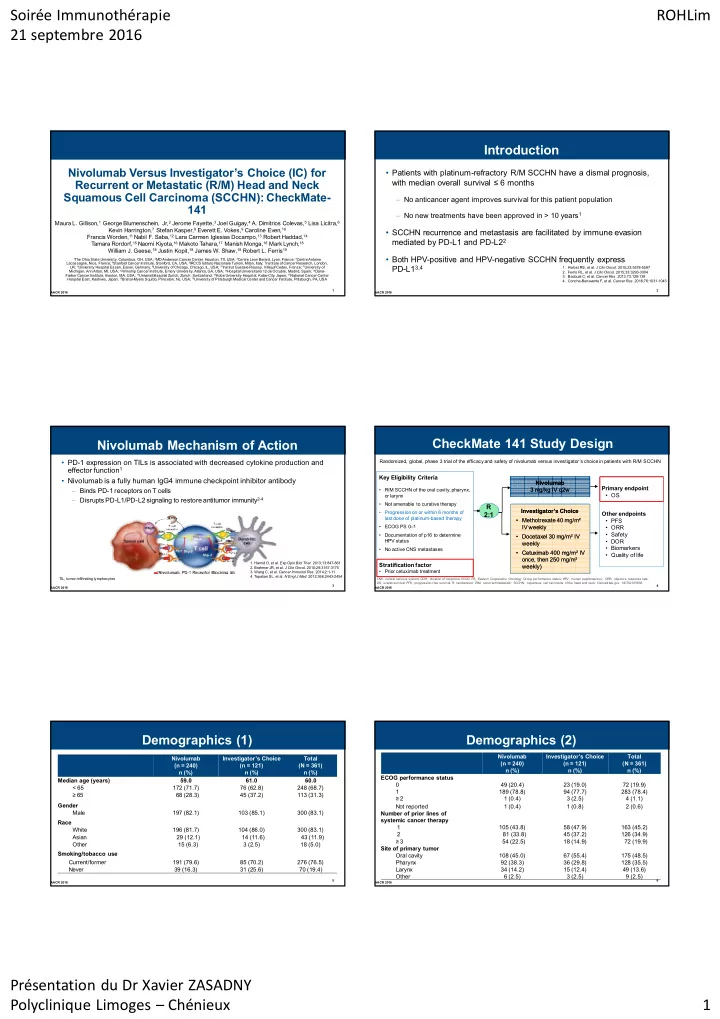
Soirée Immunothérapie ROHLim 21 septembre 2016 Treatment Administration Overall Survival Median OS, HR 100 p-value Nivolumab Investigator’s Total Overall Survival (% of patients) mo (95% CI) (97.73% CI) (n = 240) Choice (N = 361) 90 Nivolumab (n = 240) 7.5 (5.5–9.1) 0.70 (n = 121) 80 0.0101 (0.51–0.96) Investigator’s Choice (n = 121) 5.1 (4.0–6.0) Patients receiving ≥ 1 dose, n (%) 236 (98.3) 111 (91.7) 347 (96.1) 70 Investigator’s choice therapy, n (%) 60 1-year OS rate (95% CI) Methotrexate – 46 (38.0) – 50 36.0% (28.5–43.4) Docetaxel – 52 (43.0) – 40 Cetuximab – 13 (10.7) – 30 16.6% (8.6–26.8) 20 Median time on therapy, mo (95% CI) 1.9 (1.6–2.3) 1.9 (1.6–2.0) – 10 Median duration of follow-up, mo 0 5.3 (0–16.8) 4.6 (0–15.2) – 0 3 6 9 12 15 18 (range) Months Number of deaths, n (%) 133 (55.4) 85 (70.2) 218 (60.4) No. at Risk Nivolumab 240 167 109 52 24 7 0 Ongoing treatment, n (%) 41 (17.4) 3 (2.7) 44 (12.7) Investigator’s 121 87 42 17 5 1 0 Choice 7 8 AACR 2016 AACR 2016 Progression-Free Survival Objective Response Rate Nivolumab in R/M SCCHN After Platinum Therapy Nivolumab in R/M SCCHN After Platinum Therapy Median OS, mo HR Nivolumab Investigator’s Choice P -value (95% CI) (97.73% CI) 100 (n = 240) (n = 121) Nivolumab (n = 240) 2.0 (1.9, 2.1) 0.89 90 Objective response rate, n (%) 32 (13.3) 7 (5.8) 0.3236 Progression-Free Survival (0.70, 1.1) Investigator’s Choice (n = 121) 2.3 (1.9, 3.1) 80 95% CI 9.3, 18.3 2.4, 11.6 70 (% of patients) Best overall response, n (%) 60 50 Complete response 6 (2.5) 1 (0.8) 40 6-month PFS rate (95% CI) Partial response 26 (10.8) 6 (5.0) 19.7% (14.6, 25.4) 30 Stable disease 55 (22.9) 43 (35.5) 20 Progressive disease 100 (41.7) 42 (34.7) 10 9.9% (5.0, 16.9) 0 Not determined 53 (22.1) 29 (24.0) 0 3 6 9 12 15 18 Time to response, mo No. at Risk Months Nivolumab 240 79 32 12 4 1 0 Median (range) 2.1 (1.8–7.4) 2.0 (1.9–4.6) Investigator’s 121 43 9 2 0 0 0 Choice 9 10 ASCO 2016 ASCO 2016 Baseline PD-L1 Expression No. of patients Overall Survival and p16 Status Subgroups a Nivolumab IC Unstratified Hazard Ratio (95% CI) Overall 240 121 0.69 (0.53, 0.91) Age category , years <65 172 76 0.64 (0.45, 0.89) Nivolumab Investigator’s Choice Total ≥65 to <75 56 39 0.93 (0.56, 1.54) (n = 240) (n = 121) (N = 361) ≥75 12 6 n (%) n (%) n (%) ECOG performance status PD-L1 quantifiable 161 (67.1) 99 (81.8) 260 (72.0) 0 49 23 0.60 (0.30, 1.23) ≥1 190 97 0.71 (0.53, 0.96) ≥ 1% 88 (54.7) 61 (61.6) 149 (57.3) Tobacco use Current/Former 191 85 0.71 (0.52, 0.99) < 1% 73 (45.3) 38 (38.4) 111 (42.7) Never 39 31 0.58 (0.32, 1.06) PD-L1 not evaluable 79 (32.9) 22 (18.2) 101 (28.0) Prior lines of systemic therapy , n 1 106 58 0.72 (0.48, 1.07) p16 status a,b 2 80 45 0.64 (0.40, 1.00) ≥3 54 18 0.77 (0.38, 1.57) Positive 63 (26.3) 29 (24.0) 92 (25.5) Intended IC therapy Methotrexate 119 52 0.64 (0.43, 0.96) Negative 50 (20.8) 36 (29.8) 86 (23.8) Docetaxel 88 54 0.82 (0.53, 1.28) Not tested 127 (52.9) 56 (46.3) 183 (50.7) Cetuximab 33 15 0.47 (0.22, 1.01) a Required from oropharyngeal cancer patients only. 0.125 0.25 0.5 1 2 b Determined via p16 immunohistochemistry. a Hazard ratios w ere not calculated for subgroups w ith few er than 20 patients across both arms Favors Nivolumab Favors IC 12 ASCO 2016 11 AACR 2016 Présentation du Dr Xavier ZASADNY Polyclinique Limoges – Chénieux 2
Recommend
More recommend