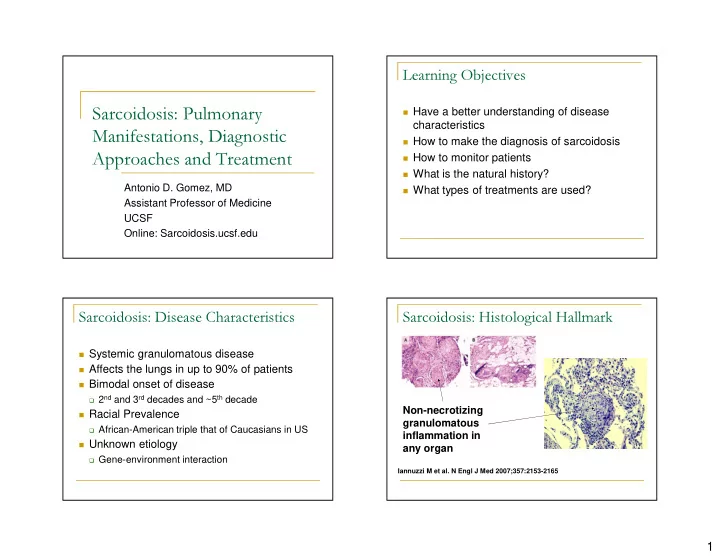
Learning Objectives � Have a better understanding of disease Sarcoidosis: Pulmonary characteristics Manifestations, Diagnostic � How to make the diagnosis of sarcoidosis � How to monitor patients Approaches and Treatment � What is the natural history? Antonio D. Gomez, MD � What types of treatments are used? Assistant Professor of Medicine UCSF Online: Sarcoidosis.ucsf.edu Sarcoidosis: Disease Characteristics Sarcoidosis: Histological Hallmark � Systemic granulomatous disease � Affects the lungs in up to 90% of patients � Bimodal onset of disease � 2 nd and 3 rd decades and ~5 th decade Non-necrotizing � Racial Prevalence granulomatous � African-American triple that of Caucasians in US inflammation in � Unknown etiology any organ � Gene-environment interaction Iannuzzi M et al. N Engl J Med 2007;357:2153-2165 1
Sarcoidosis: Clinical Presentations How to Make a Diagnosis of Sarcoidosis � Acute � Löfgren’s Syndrome � Fever, bilateral hilar lymphadenopathy, arthritis (ankle) No single diagnostic test! and erythema nodosum � Chronic � Subacute to chronic onset of symptoms � Often cough and/or shortness of breath � Systemic complaints in 25-50% � arthalgias, fatigue, chest pains, muscle pain ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 Costabel et al. Curr Opin Pulm Med. 2008 Diagnosis of Sarcoidosis Diagnosis of Sarcoidosis � Role of Angiotensin converting enzyme � High Resolution Chest CT scan (ACE) level � UCSF ILD radiologists think HRCT is very specific for the diagnosis if the classical patterns are present � Insensitive � Non-necrotic granulomas on tissue biopsy of � Non-specific affected organ � Elevated in other granulomatous diseases � Important to have an experienced lung pathologist review biopsy, especially if the interpretation is “granulomas with necrosis” ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 2
CXR Staging System Pulmonary Manifestations: Stage I, Bilateral Hilar Lymphadenopathy (BHL) Pulmonary Manifestations: Stage II, Pulmonary Manifestations: Stage III, BHL with Parenchymal Nodules Parenchymal Nodules Only Distribution: peri-lymphatic nodules, upper lobe nodules can coalesce � � 3
Pulmonary Manifestations: Stage IV, Diagnosis of Sarcoidosis Fibrosis, Cystic � Exclusion of disease mimics: � Mycobacterial or fungal infection � Send tissue specimens for culture � Travel history (e.g. histoplasmosis, coccidioidosis) � Amyloidosis � Check SPEP and UPEP patients older than 50 or 60 in whom you are evaluating for sarcoidosis � Pneumoconiosis and Berylliosis � Take thorough occupational history � Lymphoma � Clinical history of B symptoms ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 Diagnosis of Sarcoidosis Diagnosis of Sarcoidosis � Sarcoidosis can be systemic � Tests that I don’t routinely perform � Gallium scans � Thorough review of systems Unless the patient cannot undergo tissue biopsy � � PET scans � May discover extrathoracic organ involvement Similar reasoning to gallium scans � E.g. skin, joints, cardiac, central or peripheral nervous � system � ACE levels Can consider if cannot obtain a biopsy � Sarcoidosis screening studies � � lysozme levels ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 4
Sarcoidosis Screening Studies Monitoring Patients with Sarcoidosis � Pulmonary disease only: � Once diagnosis is made, the following screening is recommended: � Complete pulmonary function tests every 6 months during the first 2 years, and then yearly � 12 lead ECG and signal averaged ECG over the following 3 years unless symptoms � Serum Calcium level dictate for frequently � Precursor and mature forms of Vitamin D � Extrathoracic disease: � 25-hydroxy Vit D and 1, 25-dihydroxy Vit D � Depends on organ � Ophthalmologic evaluation � E.g Brain MRI for CNS sarcoidosis � 24 hr urine collection for calcium excretion � Monitor symptoms related to organ � Absolute CD4 count involvement ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 Natural History of Sarcoidosis Radiographic Staging: Predictor of Spontaneous Resolution � ~2/3 of patients have spontaneous resolution Spontaneous or persistent, but non-progressive disease Stage Chest Xray Finding Improvement I BHA 55-80% � ~1/3 have progressive disease II BHA, reticular infiltrates 40-60% � ~10% die from sarcoidosis-related organ involvement III Reticular infiltrates only 10-20% IV Fibrosis, volume loss 0% ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 5
Treatment Recommendations Markers of Disease Activity First Assess the need for therapy � No clinically proven biomarkers of disease activity or progression Absolute indication for corticosteroids: � Cardiac* � ACE Level: should it be used to monitor � Neurologic* disease course? � Ophthalmologic � Not enough data to recommend routine use � Hypercalcemia � Some clinicians use ACE levels to assess disease activity � In patients who present with very elevated levels, it *Often high dose (60-80 mg/day) for first several may reflect disease activity weeks/months ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 Treatment Recommendations Treatment for Pulmonary Disease Progressive worsening of symptoms or PFTs � Non-life Threatening Disease or Severe Organ Dysfunction � ~ 40 mg prednisone for 3-6 wks, and if improved symptoms, taper by 5-10 mg � Expert opinion/Controversial topic increments every 4-8 wks � High rate of spontaneous remission and low mortality rate from pulmonary disease � Relapse rate can be up to 60%, so � Stage I pts (BHA) should be observed for 6 maintenance continued for 6-8 mos, resulting months and not treated in at least a year of treatment. � Early treatment of Stage II disease (BHA + � Second-line agents added for steroid- infiltrates) may improve lung function dependent, progressive disease or steroid � No data for disease-modification long term intolerance ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 ATS/ERS/WASOG. Am J Respir Crit Care Med. 1999 Pietinalho A. Chest. 2002 Pietinalho A. Chest. 2002 6
Second-Line/Alternative Therapies Second-Line/Alternative Therapies � Methotrexate: (up to 15mg/week) � TNFa-blockers � DB-RCT: 15 new onset disease given MTX concordantly � Infliximab (Remicade): chimeric, humanized monoclonal with steroids. Less steroids used in MTX group. antibody Sarcoidosis Vasc Diffuse Lung Dis. 2000;17(1):60 � RCT: 138 patients with chronic pulmonary and extrapulmonary sarcoidosis refractory to glucocorticoid therapy (placebo, low- � Azathioprine (up to 200mg/day) dose (3 mg/kg), higher-dose (5 mg/kg) at baseline and weeks � open-label series studied azathioprine (2 mg/kg per day) 2, 6, 12, 18, and 24) combined with glucocorticoids in 11 patients with chronic or � Minimal improvement in FVC relapsing pulmonary sarcoidosis: Eur Respir J. � Adalimumab (Humira): fully human anti-TNFa antibody 1999;14(5):1117 � Case reports and small case series suggest benefit � Check serum thiopurine-S-methyltransferase (TPMT) to � Etanercept (Enbrel): soluble TNFa receptor fusion protein avoid severe pancytopenia � Not effective in pulmonary sarcoidosis Novel Therapies Take Home Points � IL-12 Antagonism (ustekinumab) � Sarcoidosis has a variable clinical course � Unpublished � Treatment often tailored to individual patient � All outcome measures negative � Spontaneous remissions are common � PRO � Difficult to predict progression, response to � Skin treatment, or relapse � Lung � No single test to indicate “active” disease � Treatment does not “cure” sarcoidosis 7
Take Home Points: Treatment of GRADS: Genomics Research in Alpha-1 Pulmonary Disease Antitrypsin disease and Sarcoidosis � No evidence that any treatment is disease modifying � NIH funded, multicenter � ICS may be beneficial for cough without significant � UCSF -- only West Coast center radiographic disease � Study design: obtain clinical data, CT scans, � Methotrexate good for steroid-dependent and blood, and BAL specimens for genomic, refractory disease genetic and microbiomic analyses � Azathioprine good as second line after methotrexate � Goal: Identify markers for disease progression intolerance or treatment failure and determine the role of microorganisms in � Modest improvement with TNF- α inhibitors and disease etiology and progression very expensive � Enrollment: NOW Thank you for your attention! 8
Recommend
More recommend