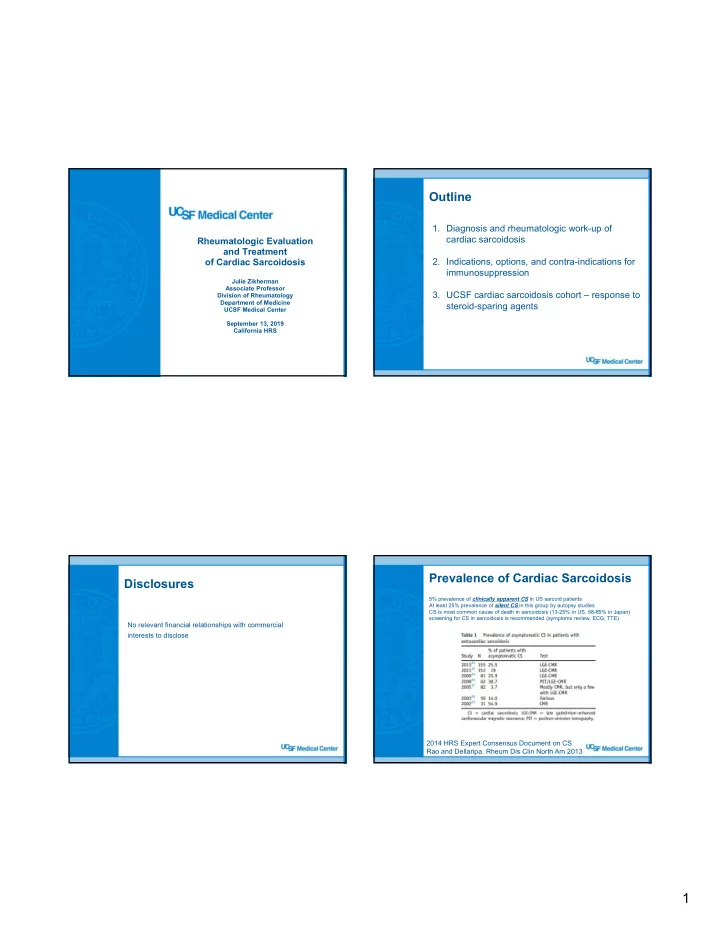
Outline 1. Diagnosis and rheumatologic work-up of cardiac sarcoidosis Rheumatologic Evaluation and Treatment 2. Indications, options, and contra-indications for of Cardiac Sarcoidosis immunosuppression Julie Zikherman Associate Professor 3. UCSF cardiac sarcoidosis cohort – response to Division of Rheumatology Department of Medicine steroid-sparing agents UCSF Medical Center September 13, 2019 California HRS Prevalence of Cardiac Sarcoidosis Disclosures 5% prevalence of clinically apparent CS in US sarcoid patients At least 25% prevalence of silent CS in this group by autopsy studies CS is most common cause of death in sarcoidosis (13-25% in US, 58-85% in Japan) screening for CS in sarcoidosis is recommended (symptoms review, ECG, TTE) No relevant financial relationships with commercial interests to disclose 2014 HRS Expert Consensus Document on CS Rao and Dellaripa. Rheum Dis Clin North Am 2013 1
Clinical Presentation: suspected CS Diagnosis of Cardiac Sarcoidosis Scenario 1 – patient with biopsy-proven (usually pulmonary) sarcoidosis who is subsequently found to have findings/symptoms suggestive of CS including conduction disease and/or VT+/- ventricular dysfunction – may be symptomatic or subclinical. Scenario 2– patient without a known history of sarcoidosis who presents with findings/symptoms suggestive of CS (conduction disease and/or VT +/- unexplained cardiomyopathy). – This group of patients largely present with symptoms – e.g. heart block, VT, CHF. specific electrophysiological features of CS covered in the next presentation 2014 HRS Expert Consensus Document on CS Diagnosis of Cardiac Sarcoidosis Approach to diagnosis and work-up Diagnosing ‘isolated’ cardiac sarcoidosis in absence of myocardial biopsy is challenging but purely clinical criteria exist: (1) Establish CS diagnosis (2) Establish extent of extra-cardiac organ involvement (3) Establish degree of active inflammation in the heart (4) Pre-screening for possible immunosuppression 2017 Japanese criteria of CS diagnosis 2017 Japanese criteria of CS diagnosis Terasaki et al. Ann of Nuc Card 2017 2
Establishing a CS diagnosis Establishing a CS diagnosis Scenario 1 – established systemic Scenario 2– patient presents with findings/symptoms suggestive of CS in sarcoidosis found to have the absence of known sarcoidosis findings/symptoms suggestive of CS. Advanced imaging with: (a) fdg-PET (ideally matched area of cMRI / FDG-PET to establish plausible cardiac inflammation. fdg uptake and perfusion defect) and/or If fdg-avid LAD especially in chest pursue LN biopsy delayed enhancement on cMRI If chest CT shows evidence of sarcoidosis bronchoscopy with EBUS bx are sufficient to establish the diagnosis (b) If neither, consider endomyocardial bx but low yield if area of focal fdg- (exclusion of other causes such as uptake/DE on cMRI does not involve an accessible area. ischemic heart disease etc.) (c) Myocardial biopsy is not required. If no cardiac biopsy, pursue a clinical diagnosis of isolated CS Often these diagnoses are clear. This is the group of patients that includes those in whom diagnosis is less certain. 2014 HRS Expert Consensus Document on CS Work-up for extra-cardiac Establishing a CS diagnosis sarcoidosis Scenario 2– patient presents with findings/symptoms suggestive of CS in Extra-cardiac/pulmonary sarcoidosis: the absence of known sarcoidosis skin, ocular, neurological, MSK, ca/d axis, renal, liver, spleen Screen for and monitor status of extra-cardiac manifestations of sarcoidosis: three routes to diagnosis -chest imaging and PFTs at baseline, and at least q 12 mo PFTs -baseline and annual ophthalmology exam -skin exam (a) (b) (c) -ROS to screen for MSK, neurological symptoms -labs to include 24hr urine ca, serum 1,25 vit D, and 25-oh vitamin D -+/- CD4 lymphocyte counts isolated cardiac -+/- Ig levels to screen for underlying CVID (can cause sarcoid-like granulomatous search for extra-cardiac sarcoidosis diagnosed positive disease) sarcoidosis and clinically (2017 endomyocardial -other w/u determined by symptoms or lab abnormalities (ideally) biopsy it Japanese criteria) biopsy e.g. CBC, LFTs, cr if not if not + + advanced cardiac advanced cardiac imaging imaging (greatest degree of uncertainty) 3
Pre-screening for possible Immunosuppression – Why Treat? immunosuppression No Randomized Data! Observational Data: -hep B serologies 1. Prevent Scarring/Heart Failure -hep C serologies -HIV 2. Prevent Arrhythmias -quantiferon 3. Reverse AV Block -baseline labs including cbc with diff, cr, LFTs 4. Prolong Life? Immunosuppression: options Who should be treated with immunosuppression? No consensus on optimal approach Standard of care had been corticosteroids Emerging role for steroid-sparing agents (SSA) Patients with definite or probable CS who have -methotrexate: ‘active cardiac inflammation’ as determined by can’t use with significant renal impairment or liver disease FDG uptake on PET first line SSA for pulmonary sarcoidosis -TNF blockers: concern in heart failure, especially NYHA class 3/4 effective for ocular and neurologic sarcoidosis, but less so with pulmonary disease clinical judgment is important in cases where -azathioprine: contra-indications to immunosuppression exist screen for low metabolizer TPMT pht/gt, (e.g. recent cancer) and/or uncertainty about the risk of cytopenias especially leukopenia diagnosis exists (e.g. no tissue, isolated CS) Second line SSA for pulmonary sarcoidosis -cellcept: less data for sarcoidosis, but likely effective - newer kinase inhibitors and other biologics: Jak inhibitors? IL-6 blockade? Insufficient data so far 14 4
Response of UCSF CS cohort to Our treatment algorithm immunosuppression INITIAL APPROACH n p e r Prednisone approx. 40mg/d taper over 3-4 months to <=5mg/d u t n p . Simultaneously introduce SSA (first line is mtx) o d w c e titrate mtx up to 20mg po weekly (or sc if GI intolerance) e s s i o t v f/u PET once pred <=5mg/d and >= 3 months on mtx i l e c d r s n l i d a a SECOND LINE n t r p r e u If intolerant to mtx or incomplete response on PET: TNFi i h r o t c j r Adalimumab (Humira) 40mg sc q 2 weeks (+ mtx 7.5-15mg/wk) s u r u o f Other TNF mAbs reasonable (e.g. infliximab, certolizumab, golimumab) n e f a b d Etanercept (Enbrel) is a soluble TNF receptor: m e o d t NOT effective and can cause sarcoidosis (rarely). e n h t e o T If CS diagnosis isolated and uncertain: less likely to use TNFi t n n : i d If EF severely depressed and/or class 3-4 NYHA symptoms, avoid TNFi r e , n l m a a i i t , a n THIRD LINE y l e l c n s d If neither mtx nor TNFi can be used, or both fail: aza or cellcept o i i f D n o Confirmatory PET on each new therapy to ensure response Surveillance PETs on stable therapy Rosenthal et al. manuscript in press, JAHA 2019 17 19 UCSF CS cohort: Response of UCSF CS cohort to nearly all with clinical disease immunosuppression and extra-cardiac sarcoidosis Rosenthal et al. manuscript in press, JAHA 2019 Rosenthal et al. manuscript in press, JAHA 2019 18 20 5
Conclusions Recurrence OFF immunosuppression • Patients with systemic sarcoidosis should be screened for CS High rate of recurrent positive PET after discontinuing IS • Increasing role for advanced cardiac imaging (cMRI, PET) in diagnosis and monitoring of CS (89%) • No randomized data, but immunosuppression for active disease can prevent deterioration in EF, improve ventricular arrhythmias, and (16%) reverse complete heart block • UCSF cohort data suggests mtx or adalimumab may be effective SSAs • UCSF cohort data suggests significant rate of radiographic and clinical recurrence after IS stopped • UCSF cohort shows some relapse ON immunosuppression so we favor ongoing surveillance with PET scans Rosenthal et al. manuscript in press, JAHA 2019 21 Active Questions in clinical Relapse ON immunosuppression diagnosis and management of CS (89%) -Should clinically-silent CS be treated? (16%) -What is optimal up-front IS? -Duration of IS? We have seen recurrent disease ON therapy : -How common is isolated CS? -subclinical progression caught on PET -clinical disease including worsening LV dysfunction and recurrent heart block consider surveillance PET even ON therapy Rosenthal et al. manuscript in press, JAHA 2019 22 6
Acknowledgements clinical research and care of UCSF sarcoidosis patients: David Rosenthal, UCSF EP Fellow Vasanth Vedantham and colleagues, UCSF EP Van Selby, Teresa DeMarco and colleagues, UCSF cardiology Laura Koth, Nikko Arger and colleagues, UCSF Pulmonary Jeff Gelfand, UCSF Neurology 25 7
Recommend
More recommend