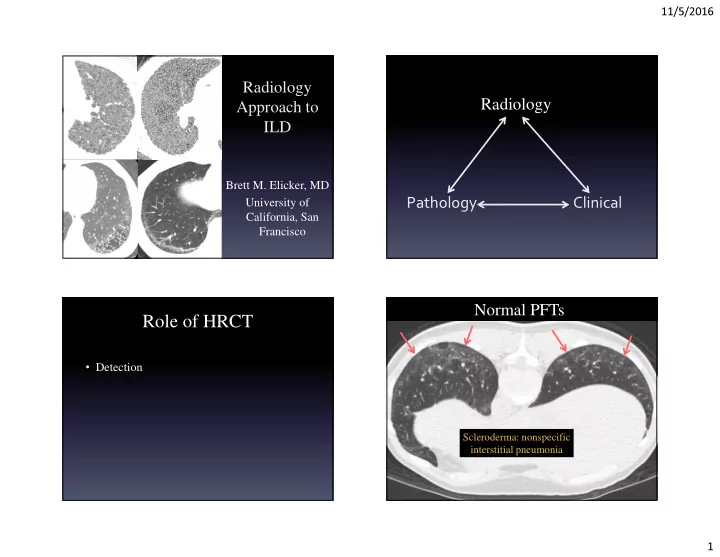
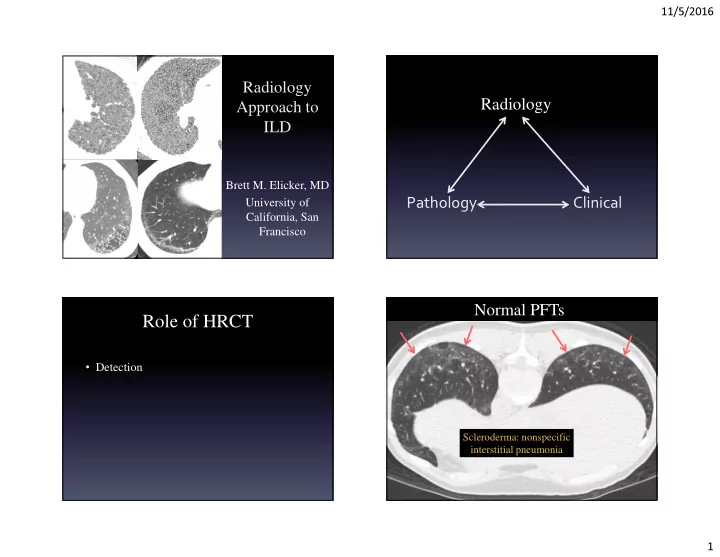
11/5/2016 Radiology Radiology Approach to ILD Brett M. Elicker, MD University of Pathology Clinical California, San Francisco Normal PFTs Role of HRCT • Detection Scleroderma: nonspecific interstitial pneumonia 1
11/5/2016 End stage constrictive bronchiolitis Inspiration Expiration HRCT may show reduced sensitivity for: • Small airways diseases – Constrictive broncholitis – Hypersensitivity pneumonitis – Asthma • Emphysema • Pulmonary hypertension Markedly reduced FEV1 NSIP + pulmonary hypertension Role of HRCT • Detection • Diagnosis Markedly reduced DLCO 2
11/5/2016 Confidence in diagnosis Definitive HRCT HRCT + clinical: Nonspecific HRCT pattern diagnostic 3
11/5/2016 Pathology: the gold standard Clinical Context Adenocarcinoma Scar • Bird exposure -> hypersensitivity pneumonitis • Smoker -> respiratory bronchiolitis • Connective tissue disease -> follicular bronchiolitis • Iron welder -> siderosis • Acute symptoms -> viral infection Pathology: NSIP Diagnosis: HP Role of HRCT • Detection • Diagnosis • Fibrosis vs. inflammation 4
11/5/2016 Fibrosis vs. Inflammation Role of HRCT No GGO- fibrosis GGO- inflammation GGO- fibrosis • Detection • Diagnosis • Fibrosis vs. inflammation • Next step in management HRCT guides further work-up Role of HRCT Bronchoscopy Sputum VATS • Detection • Diagnosis • Fibrosis vs. inflammation • Next step in management • Serial changes 5
11/5/2016 Clinical/PFT deterioration HRCT: follow-up after tx 6 months later Initial Acute exacerbation of IPF Role of HRCT • Detection • Diagnosis • Fibrosis vs. inflammation • Next step in management • Serial changes 6
11/5/2016 ? diagnosis Idiopathic Clinical Histologic Pattern Associated Diseases Syndrome Usual interstitial Idiopathic pulmonary Connective tissue disease pneumonia fibrosis (CTD), drugs, asbestosis CTD, drugs, Nonspecific interstitial Idiopathic NSIP hypersensitivity pneumonia (NSIP) pneumonitis (HP) Desquamative interstitial Smoking, CTD, drugs, toxic Idiopathic DIP pneumonia (DIP) inhalation CTD, drugs, infections, Organizing pneumonia Cryptogenic OP chronic eosinophilic (OP) pneumonia, HP Post-viral, CTD, drugs, Constrictive bronchiolitis Idiopathic CB graft vs. host disease, lung (CB) transplant rejection Infection, aspiration, Acute interstitial Diffuse alveolar damage trauma, sepsis, pneumonia pancreatitis, etc. Radiology <-> Pathology Idiopathic Clinical Idiopathic Clinical Histologic Pattern Histologic Pattern Associated Diseases Associated Diseases Syndrome Syndrome Usual interstitial Usual interstitial Idiopathic pulmonary Idiopathic pulmonary Connective tissue disease Connective tissue disease pneumonia pneumonia fibrosis fibrosis (CTD), drugs, asbestosis (CTD), drugs, asbestosis CTD, drugs, CTD, drugs, Nonspecific interstitial Nonspecific interstitial Idiopathic NSIP Idiopathic NSIP hypersensitivity hypersensitivity pneumonia (NSIP) pneumonia (NSIP) pneumonitis (HP) pneumonitis (HP) Desquamative interstitial Desquamative interstitial Smoking, CTD, drugs, toxic Smoking, CTD, drugs, toxic Idiopathic DIP Idiopathic DIP pneumonia (DIP) pneumonia (DIP) inhalation inhalation CTD, drugs, infections, CTD, drugs, infections, Organizing pneumonia Organizing pneumonia Cryptogenic OP Cryptogenic OP chronic eosinophilic chronic eosinophilic (OP) (OP) pneumonia, HP pneumonia, HP Post-viral, CTD, drugs, Post-viral, CTD, drugs, Constrictive bronchiolitis Constrictive bronchiolitis Idiopathic CB Idiopathic CB graft vs. host disease, lung graft vs. host disease, lung (CB) (CB) transplant rejection transplant rejection Infection, aspiration, Infection, aspiration, Acute interstitial Acute interstitial Diffuse alveolar damage Diffuse alveolar damage trauma, sepsis, trauma, sepsis, pneumonia pneumonia pancreatitis, etc. pancreatitis, etc. 7
11/5/2016 Definite UIP: IPF Usual interstitial pneumonia (HRCT) • Honeycombing features Raghu et al. Am J Respir Crit Care Med 2011; 183: 788 – Air density Inconsistent with – Round with fairly thick wall Definite UIP Possible UIP UIP – Always involves subpleural Irregular reticulation Irregular reticulation lung Honeycombing NO honeycombing – Associated signs of fibrosis Mid-upper lung Subpleural, basilar Subpleural, basilar distribution OR not distribution distribution subpleural distribution OR presence of Absence of features Absence of features features inconsistent inconsistent with UIP inconsistent with UIP with UIP UIP: non-idiopathic causes What % of patients have IPF? Raghu et al. Am J Respir Crit Care Med 2011; 183: 788 95% 65% 25% Drug Asbestosis Inconsistent with Definite UIP Possible UIP UIP Irregular reticulation Irregular reticulation Honeycombing (HC) NO honeycombing Mid-upper lung Subpleural, basilar Subpleural, basilar distribution OR not distribution distribution subpleural distribution Rheumatoid OR presence of Absence of features Absence of features features inconsistent inconsistent with UIP inconsistent with UIP with UIP 8
11/5/2016 Nonspecific interstitial pneumonia Findings inconsistent with UIP (NSIP) Subpleural • 1. Ground glass opacity sparing • 2. Mosaic perfusion/air trapping ( ≥ 3 lobes) • 3. Profuse micronodules • 4. Discrete cysts • 5. Consolidation • 6. Mid-upper lung predominance • 7. Peribronchovascular predominance Nonspecific interstitial pneumonia Bronchiectasis 9
11/5/2016 Desquamative interstitial pneumonia Desquamative interstitial pneumonia Cystic abnormality Lymphoid interstitial pneumonia VATS: UIP Explant: HP Cysts + nodules Mosaic perfusion ≥ 3 lobes Definitely not “possible UIP” 10
11/5/2016 Familial Interstitial Lung Disease Idiopathic pulmonary fibrosis Leslie et al. Arch Pathol Lab Med 2012; 136: 1366 Lee et al. Chest 2012; 142: 1577 • Genetic mutation (e.g. telomerase) or idiopathic • 2-20% cases of IPF • Earlier age of onset (<50 years old) • Pathology – Unclassifiable fibrosis: 60% Ground glass opacity – UIP: 40% • Radiology – Definite/possible UIP (22%) Inconsistent with UIP – Honeycombing (32%) Radiology Approach to Familial: ILD surfactant protein C mutation Brett M. Elicker, MD University of California, San Francisco 11
Recommend
More recommend