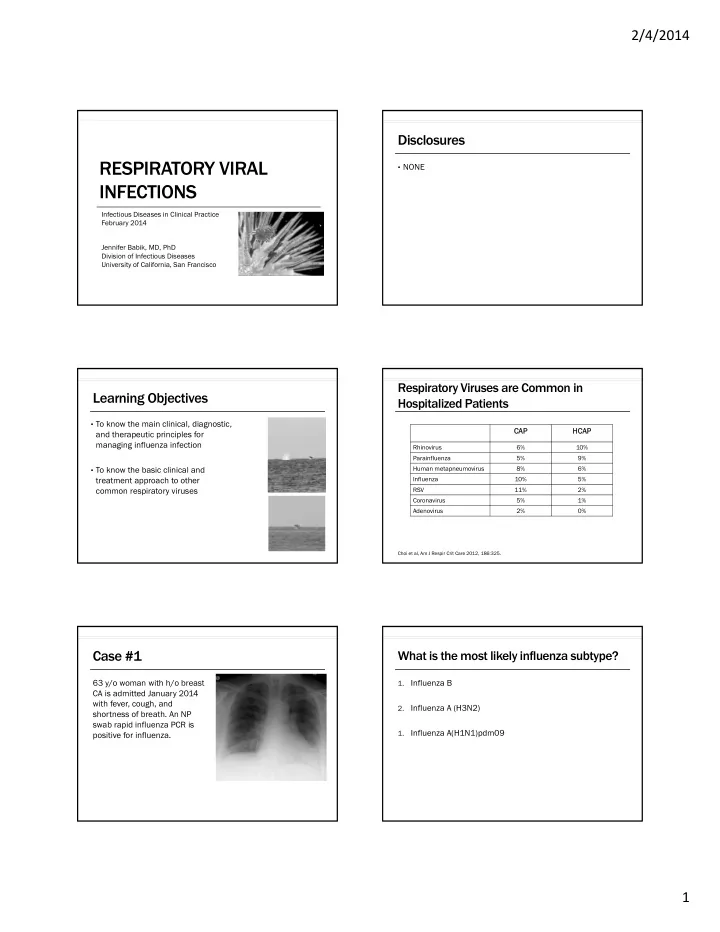
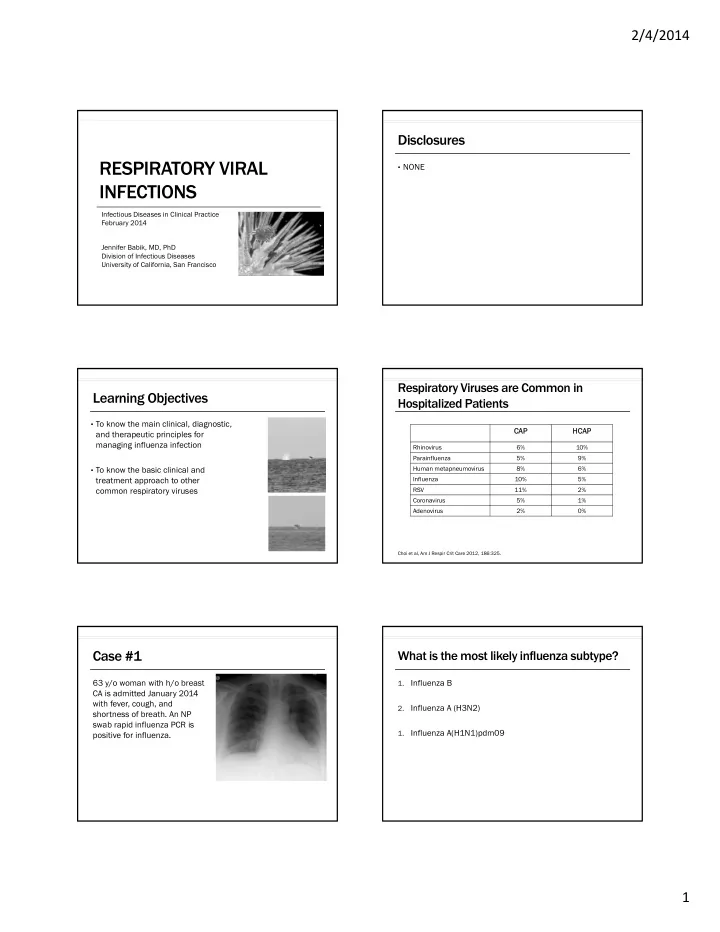
2/4/2014 Disclosures RESPIRATORY VIRAL • NONE INFECTIONS Infectious Diseases in Clinical Practice February 2014 Jennifer Babik, MD, PhD Division of Infectious Diseases University of California, San Francisco Respiratory Viruses are Common in Learning Objectives Hospitalized Patients • To know the main clinical, diagnostic, CA CAP HCAP CAP and therapeutic principles for managing influenza infection Rhinovirus 6% 10% Parainfluenza 5% 9% • To know the basic clinical and Human metapneumovirus 8% 6% treatment approach to other Influenza 10% 5% common respiratory viruses RSV 11% 2% Coronavirus 5% 1% Adenovirus 2% 0% Choi et al, Am J Respir Crit Care 2012, 186:325. Case #1 What is the most likely influenza subtype? 63 y/o woman with h/o breast 1. Influenza B CA is admitted January 2014 with fever, cough, and 2. Influenza A (H3N2) shortness of breath. An NP swab rapid influenza PCR is 1. Influenza A(H1N1)pdm09 positive for influenza. 1
2/4/2014 Influenza Influenza Types • Influenza A • From the Italian word • Infects humans, mammals (pigs), birds meaning “influence” • Subtypes based on type of hemagglutinin (H) or neuraminidase (N) because it was thought present • 18 possible H subtypes, 11 possible N subtypes that the stars and planets caused and • Influenza B controlled diseases • Infects humans only • No subtypes • Influenza C • Causes only mild disease in humans • No subtypes Influenza Nomenclature Antigenic Variation Antigenic Shift • Influenza A/mallard/Memphis/123/95 (H5N1) Antigenic Drift Influenza A only • Influenza A or B • Caused by major change in viral • Caused by point mutations • genome (e.g., reassortment) • Minor changes Influenza Animal host Site of Strain Year Subtype These major changes can result type (A, B, C) (omit if human) isolation number isolated • Leads to annual flu • in a new HA subtype epidemics Can lead to pandemics because • humans have little to no immunity to the new HA • Pandemic influenza A (H1N1) is referred to as A(H1N1)pdm09 Gene Reassortment Terminology • Epidemic: confined to one location • Seasonal influenza • Influenza A, influenza B • Results from antigenic drift • Pandemic: global outbreak • When a population has limited immunity to a virus • Sustained human-to-human spread global transmission • Influenza A only • Results from antigenic shift CDC, Images of Avian Influenza A H7N9, 2013. 2
2/4/2014 Prior Pandemics Pandemic H1N1 (“Swine Flu”) 8000-18000 deaths in the US 50 million deaths 70,000 deaths 34,000 deaths worldwide in the US in the US Neumann et al, Nature 2009, 459:931. Neumann et al, Nature 2009, 459:931. Seasonal Influenza vs Pandemic H1N1 Influenza Transmission • Transmitted via: Pande ndemic H1N H1N1 Seaso asonal Infl Influenz nza Average age 51 72 • Respiratory droplets • Fomites (infective for 2-8h) Major comorbidities 35% 53% • Incubation 1-4 days • Adults are infections from 1 day prior to sx onset until 5-7 days after ( in kids) Back to the Case… Which is the most predictive of influenza? 63 y/o woman with a h/o breast CA admitted with fever, 1. Sudden onset fever + myalgias cough, and shortness of breath and found to have influenza A (H1N1)pdm09. 2. Sudden onset fever + headache 3. Sudden onset fever + cough 3
2/4/2014 Influenza: Clinical Influenza: Are any Symptoms Predictive? Signs/Sx Sign s/Sx in in pa patie tients with with pH1N1 pH1N1 • Hospitalized patients with • In studies looking at pts ≥ 60 yrs old, the strongest predictors were: pandemic H1N1 are more Fever 95% likely to be: • Acute onset of both fever and cough (LR 5.4) Cough 93% • Fever (LR 3.8) • Younger SOB 73% • Malaise or (LR 2.6) Fatigue/weakness 54% • Obese • Myalgias (LR 2.4) Chills 61% • Pregnant Rhinorrhea 32% • In studies without age restriction • Have no comorbidities Myalgias 51% • Need ICU admission • There were no strong positive predictors HA 45% • Absence of fever, cough, congestion were negative predictors (LR<0.5) • No difference in mortality Sore throat 31% Vomiting 26% Wheezing 27% Diarrhea 25% Call et al, JAMA 2005, 293:987. Lee et al, J Infect Dis 2011, 203:1739. Jain et al, N Engl J Med 2009, 361:1935. Influenza in Immunocompromised Hosts Back to the case… • Less likely to have: She starts requiring more oxygen while in the ED and so gets a CT scan. • Fever • Cough, SOB • Chills/sweats • More likely to have: • Decreased appetite • Abnormal pulmonary exam/CXR • Need for hospitalization • Need for mechanical ventilation • Higher mortality • Longer viral shedding (median 8 vs 5d, mean 19 vs 6 d) ICH non-ICH Memoli et al, Clin Infect Dis 2014, 58:214. Ison, Influenza and Other Respir Viruses 2013, 7 Suppl 3: 60. Centilobular nodules indicate: CXR Findings in Influenza • Of hospitalized adults with 1. Influenza PNA influenza, 40-60% have an abnormal CXR 2. Secondary bacterial PNA • Infiltrates are: 3. Either • Bilateral 60-70%, unilateral 30-40% • Consolidations in 75-90% • Interstitial thickening 60% • ~8% of patients with PNA by CT scan have a normal CXR Jain et al, Clin Infect Dis 2012, 54:1221. Jartti et al, Acta Radiologica 2011, 52: 297. Jain et al, N Engl J Med 2009, 361:1935. Agarwal et al, AJR 2009, 193: 1488. 4
2/4/2014 Chest CT Findings in Influenza PNA Pathology of Influenza PNA • GGO 90% • Capillary thrombosis • Consolidations 66% • Alveolar necrosis and • Centrilobular nodules 60% hemorrhage • Tree-in-bud 22% • Necrotizing bronchitis and bronchiolitis Consolidations+GGO Centrilobular nodules+GGO GGO predominant Kang et al, J Comput Assist Tomogr 2012, 36:285. Cesario, Clin Infect Dis 2012, 55:107. Case #2 What is the next appropriate test? A 35 year old man is admitted 1. Rapid influenza antigen test with 5 days of fever and cough and progressive respiratory 2. Repeat NP swab for influenza PCR distress. He is intubated but rapidly deteriorates and is 3. Nasal wash for influenza PCR started on ECMO. Rapid influenza PCR from an NP swab is negative. 4. Lower tract sampling for influenza PCR Diagnosis Case #2 Continued • Rapid antigen tests (point-of-care) and DFA testing: He gets an endotracheal aspirate and the sample is positive • ~50-70% sensitive (a lot of false negatives during flu season!) for influenza A. • >90% specific • PCR testing (test of choice): • ~95% sensitive and specific • Samples: • NP aspirates or swabs • Collect samples preferably within 5 days (as shedding is after 5d) • In critically ill patients: collect both upper and lower tract specimens as lower tract samples can be positive even if viral shedding is no longer detectable in the upper tract Harper et al, Clin Infect Dis 2009, 48:1003. CDC, Influenza Symptoms and the Role of Laboratory Diagnostics, 2011. 5
2/4/2014 Would you give him antivirals? Antivirals 1. No antivirals (he is out of the treatment window) 2. Oseltamivir 75mg PO bid x 5 days 3. Oseltamivir 150mg PO bid x 10 days Matrix proteins (M1 and M2) 4. Zanamavir 10mg inhaled daily X M2 Inhibitors Neuraminidase Inhibitors • Amantadine, rimantidine • Oseltamivir, Zanamivir • Influenza A only • Influenza A and B • Widespread resistance • Drugs of choice Neurominidase Inhibitors Timing of Oseltamivir in Outpatients • Effect of oseltamivir <48h after symptom onset in healthy adults: • symptoms by ~1 day Drug Drug Adul ult dosag age Renal ally Can us Can use if Contrain raindica dicati tions Adverse se Effects cts • Conflicting data on the effect on influenza complications (e.g., PNA), do dose se? intu in tuba bated? hospitalizations, and mortality • The earlier therapy is started the greater the effect Oseltamivir 75mg PO bid Yes Yes None N/V in ~10% • Why 48hrs?: viral replication is largely controlled by most healthy Zanamivir 10 mg No No Underlying Bronchospasm, outpatients by 48 hours (2 inhalations) respiratory cough daily disease (eg, asthma, COPD) • Recent RTC showing Rx for up to 72 h after illness onset sx by ~1 d and viral shedding (mostly children) Jefferson et al, Cochrane Database Syst Rev 2012. Fry et al, Lancet Infect Dis, 2014, 14:109. Aoki et al, J Antimicrob Chemother 2003, 51:123. Timing of Oseltamivir in Inpatients Timing of Rx: Better Late than Never Treatment mortality, even up Days after symptom onset • >40% of patients hospitalized with influenza present at >48 to 5 days after symptom onset 0 1 hrs after symptom onset 2 3 4 % patients who survived Rx 5 No • Multiple studies have shown a mortality benefit for treating Rx inpatients: • Treatment within 48hrs mortality by 50-65% • Treatment seems to be effective even out to 5-6 days • But earlier is better: each day in delay increases risk of death by 20% Lee and Ison, Clin Infect Dis 2012, 55:1205. Viasus et al, Chest 2011, 140:1025. Muthuri et al, J Infect Louie et al, Clin Infect Dis 2012, 55:1198. Dis 2013, 207:553. 6
Recommend
More recommend