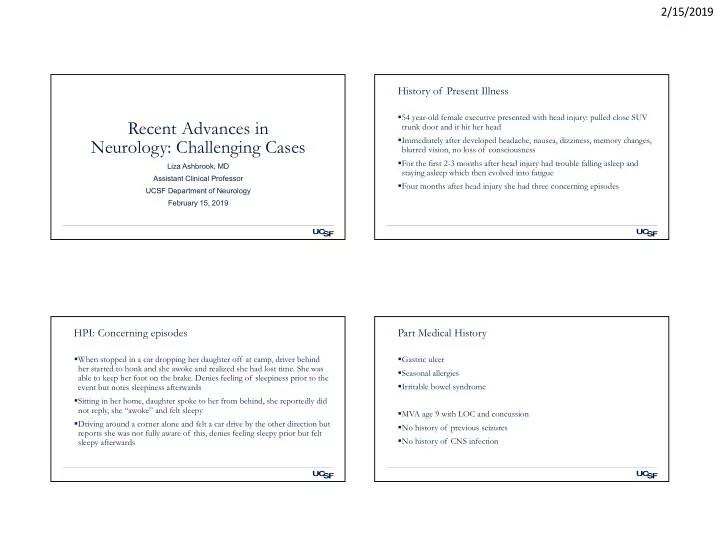
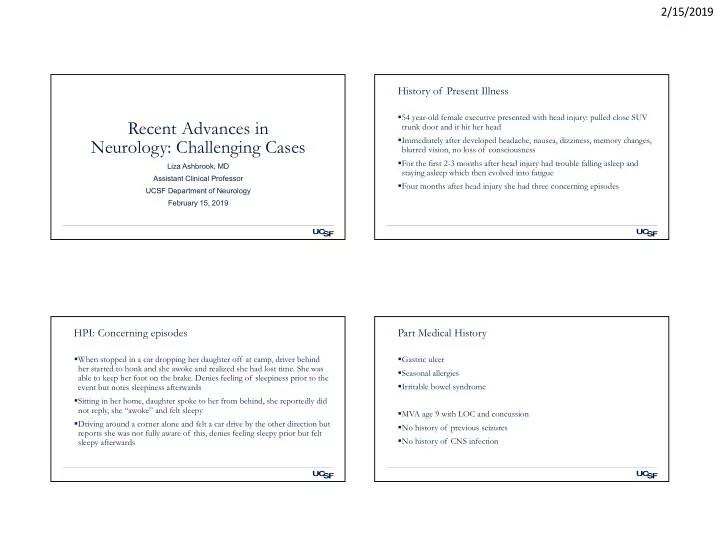
2/15/2019 History of Present Illness 54 year-old female executive presented with head injury: pulled close SUV Recent Advances in trunk door and it hit her head Immediately after developed headache, nausea, dizziness, memory changes, Neurology: Challenging Cases blurred vision, no loss of consciousness For the first 2-3 months after head injury had trouble falling asleep and Liza Ashbrook, MD staying asleep which then evolved into fatigue Assistant Clinical Professor Four months after head injury she had three concerning episodes UCSF Department of Neurology February 15, 2019 HPI: Concerning episodes Part Medical History When stopped in a car dropping her daughter off at camp, driver behind Gastric ulcer her started to honk and she awoke and realized she had lost time. She was Seasonal allergies able to keep her foot on the brake. Denies feeling of sleepiness prior to the Irritable bowel syndrome event but notes sleepiness afterwards Sitting in her home, daughter spoke to her from behind, she reportedly did not reply, she “awoke” and felt sleepy MVA age 9 with LOC and concussion Driving around a corner alone and felt a car drive by the other direction but No history of previous seizures reports she was not fully aware of this, denies feeling sleepy prior but felt No history of CNS infection sleepy afterwards 1
2/15/2019 Additional history Physical Exam General: not manifestly sleepy. Medications at time of concussion Normal HEENT exam with Mallampati 2, no turbinate hypertrophy, Ibuprofen prn micrognathia, retrognathia, or high arched palate Medications started during treatment of concussion Neuro Melatonin 1mg prn • MS: Alert, oriented, memory intact to details of the history aside from the moment of the events Nortriptyline 10mg above • CN: intact, no nystagmus Rizatriptan prn • Motor: intact rapid tapping, no pronator drift FH: No FH of seizure or sleep disorders. Father snores • Sensory: intact to light touch, negative Romberg SH: Mother of 3, twin 14 yo and 12 yo. Works full time as an executive in banking. No • Coordination: No dysmetria smoking, heavy alcohol use • Gait: normal casual gait, can tandem Evaluation Question 1: Which sleep disorder is NOT noted to occur more commonly after TBI than in the general population? Patient was referred to epilepsy clinic and an outpatient EEG was performed and normal A. Insomnia 63% Then referred for sleep evaluation in which she reported B. Hypersomnia • Bedtime: 11 C. Advanced sleep-wake phase disorder • Wake time: 6:30-8am D. Narcolepsy • Sleep latency: 20-60 minutes E. Central sleep apnea 17% 15% • Awakenings after sleep onset: 0-1 3% 3% • Naps: 1-3 times per week (recommended by psychologist), they are refreshing • Epworth sleepiness scale: 7 (>10 ‘pathologic’) a a y a i n i . s e n . . p m m e n • She does snore, no witnessed breathing pauses and no report of leg kicking e p o s l o a o a s s h c n r p e p r e I p a e N e y k l H s a w a l • No hypnogogic or hypnopompic hallucinations, sleep paralysis, cataplexy - r p t n e e e l C s d e c n a :01 v d A 2
2/15/2019 PSG with MSLT was performed Question 2: What are the MSLT criteria for narcolepsy? KEY: MSL=Mean sleep latency; SOREMP=sleep onset REM period 44% MSLT: mean sleep latency test A. MSL<15 minutes, 5/5 SOREMP 29% • Following an all night polysomnogram, patient undergoes a series of 5 B. MSL <8 minutes, 2+/5 SOREMP naps at two hour intervals 15% C. MSL <5 minutes, 5/5 SOREMP • There is a 20 minute opportunity to sleep D. MSL <8 minutes, 0/5 SOREMP 6% 6% • Once asleep, the patient’s sleep is observed for 15 minutes to assess for E. MSL <15 minutes, 2+/5 SOREMP the presence of REM P P P P M M M M . E E E E . R R R R O . O O O O S S S S S 5 5 5 5 5 / / / / / + + 2 5 5 0 2 , s , , , s e , s s e s e e t e t t t u t u u u n u n n n i n i i m i m i m m m 5 5 8 5 1 8 < < 1 < < < L L :01 L L L S S S S M M S M M M PSG results MSLT 3
2/15/2019 Epidemiology of sleep disorders in traumatic brain injury MSLT Results Prevalence varies by definition of TBI, sleep disorder: 30% to 70% Insomnia 29% Hypersomnia 28% Periodic limb movements 19% Obstructive sleep apnea 25% Narcolepsy 4% From a meta-analysis with all TBI, Mild 214, mod 38, severe 1147 Mathias et al, Sleep Medicine, 2012 Natural history Natural history • By one year post injury Mild TBI • 65% report some sleep disruption initially ( N=346, Theadom et al Sleep Medicine, 2015) ‒ 41% still have some sleep difficulties • Excessive daytime sleepiness increased from the two weeks to one month post-injury ‒ 20% have insomnia symptoms at a clinically significant level (PSQI>8) • Less than 10% reported pre-injury sleep trouble ‒ 20% have excessive daytime sleepiness (ESS>10) • Improvement up to six months • After six months many sleep issues remain stable or worsen ‒ Within mild TBI, severity of injury did not predict sleep disturbance • At 18 months those with TBI of any severity require more sleep on average than controls (7.1 vs 8.1 hours) • Patients are often not aware of their daytime sleepiness or higher sleep need Severe TBI • 84% had sleep-wake disturbances upon admission to rehab, 66% at one month post-injury 4
2/15/2019 Question 3: Sleep trouble immediately after concussion Risk factors for sleep trouble at one year predicts trouble with what at one year? • Pre-injury sleep difficulty A. Prolonged concussion recovery 93% • Sleep difficulty within first two weeks after injury B. Anxiety • Cognitive difficult within first two weeks after injury C. Depression • Increased age (in some studies) D. Worsened post-concussive symptoms • Female gender (in some studies) E. All of the above 5% 1% 0% 1% n y e y t o . r e . . v e i s i e o x s b v n v o e i a c A r s p s e e u h r e D c t n n o o f o s i c - l l s t A u s c o n p o c d e d n e e g s n r o o :01 W l o r P Sleep disruption predicts worse recovery Mechanisms of sleep change in TBI Sleep trouble within first two weeks predicts at twelve months Hypocretin (orexin): • Post concussive symptoms • Anxiety Hypocretin is low in >90% of TBI patients admitted to the hospital but returns to normal in all but 19% • Depression at six months • Decreased social integration Mouse models show low hypocretin in mild TBI as well • Productivity Melatonin These factors do not predict sleep quality at one year Total melatonin levels are decreased in TBI Among patients with mTBI who presented to the ED, those with sleep complaints were Most studies show normal timing of dim light melatonin onset (DLMO), arguing against TBI causing a • nearly five times more likely to have depression at six weeks phase delay • three times more likely to have headache Other Premorbid sleep disruption contributes to prolonged recovery Diffuse axonal injury interferes with sleep and circadian circuits Countercoup injuries can impact the basal forebrain, a major wake promoting center, due to collision with sphenoid ridge at the skull base Bramley et al, Clinical pediatrics 2017; Chaput et al, Sleep Medicine, 2009 5
2/15/2019 Treatment: Insomnia Treatment: Circadian disruption Treatment is similar to insomnia in the general population including: One of three with insomnia have a circadian rhythm disorder • Cognitive behavioral therapy for insomnia • Delayed sleep-wake phase disorder or irregular sleep-wake phase disorder are the most common circadian disorders in the post concussive period • Melatonin and melatonin agonists Likely blunting of circadian rhythm from injury and/or from change in • Antidepressants including trazodone, doxepin external circadian cues and unmasking of underlying chronotype rather • Hypnotics: zolpidem, eszopiclone, zaleplon, suvorexant than a shift in the rhythm Treated with morning light, evening melatonin 0.5 mg 4-5 hour before bedtime, daytime activity, minimizing evening light exposure Treatment: Excessive daytime sleepiness Our patient Look for underlying causes: • Insufficient sleep • Sedating medications Narcolepsy criteria • Obstructive sleep apnea • Daily periods of irrepressible need to sleep or daytime lapses into sleep for at least • Restless leg syndrome/periodic leg movement disorder three months • Depression Adequate sleep opportunity at night • MSLT with MSL<8 min and 2+ SOREMPs Timed naps The patient does not meet the daily sleepiness criteria Morning bright light : sunlight, lightbox 10,000 Lux full spectrum, blue light Differential diagnosis for positive MSLT: • 45 min/morning, short wavelength blue light therapy (λmax = 465 nm, 39.5 lux) superior to yellow light therapy • Sleep deprivation : this reported tinnitus and husband’s snoring were disturbing her sleep in the two weeks prior to the study, 44% stage 3 sleep suggests rebound from Wake promoting medication sleep deprivation • Modafinil 100-200mg BID improves excessive daytime sleepiness but not fatigue • Antidepressant withdrawal : she was actually on nortriptyline 20mg at the time of the study, reports sometimes missing doses • Armodafinil 150-250mg Treatment: modafinil 100-200mg Stimulants : methylphenidate, dextroamphetamine/amphetamine 6
Recommend
More recommend