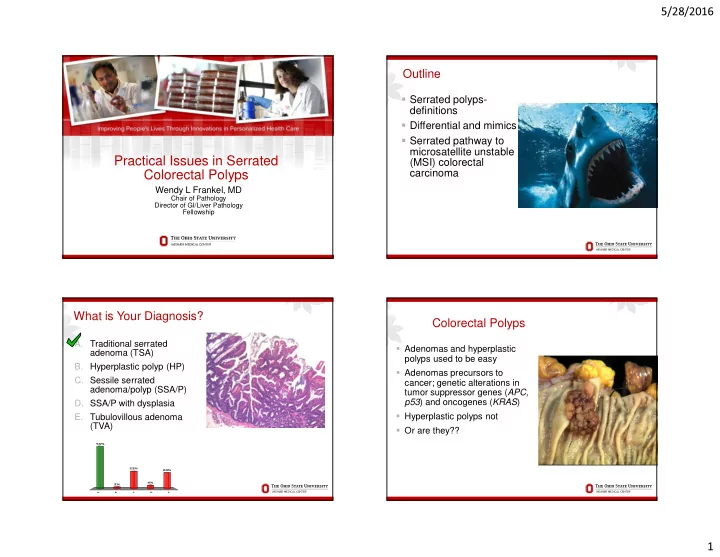
5/28/2016 Outline � Serrated polyps- definitions � Differential and mimics � Serrated pathway to microsatellite unstable Practical Issues in Serrated (MSI) colorectal carcinoma Colorectal Polyps Wendy L Frankel, MD Chair of Pathology Director of GI/Liver Pathology Fellowship What is Your Diagnosis? Colorectal Polyps A. Traditional serrated � Adenomas and hyperplastic adenoma (TSA) polyps used to be easy B. Hyperplastic polyp (HP) � Adenomas precursors to C. Sessile serrated cancer; genetic alterations in adenoma/polyp (SSA/P) tumor suppressor genes ( APC , p53 ) and oncogenes ( KRAS ) D. SSA/P with dysplasia � Hyperplastic polyps not E. Tubulovillous adenoma (TVA) � Or are they?? 53% 22% 20% 4% 2% A. B. C. D. E. 1
5/28/2016 USCAP 2004 Rodger Haggitt GIPS Companion Meeting Evolution of a Shift CURRENT ISSUES IN GI POLYP PATHOLOGY Moderator : Wendy Frankel � 1984; Urbanski described CRC arising in HP/TA Agenda: 1:30 Diagnosis and management of polyps in IBD � 1990; Longacre and Fenoglio-Prieser described polyps architectural features of HP but with dysplasia- serrated Robert D. Odze 2:05 Adenocarcinoma in adenomas: Diagnosis and management adenoma Mary P. Bronner � 1996; Torlakovic & Snover characterized lesions in 2:40 Annoying polyps without names: Pimples and zits of the gut patients with hyperplastic polyposis; serrated Henry D. Appelman adenomatous polyposis 3:15BREAK 3:45 Serrated colorectal polyps: New challenges to old dogma � 2003; Torlakovic studied sporadic serrated lesions and Kenneth P. Batts identified some with abnormal proliferation, SSA RODGER C. HAGGITT MEMORIAL LECTURE 4:20 Gastric lumps and bumps Robert M. Genta Urbanski, Am J Surg Pathol , 1984; Longacre, Am J Surg Pathol , 1990; Torlakovic and Snover, Gastroenterol, 1996; Torlakovic, Am J Surg Pathol , 2003 Hyperplastic Polyp Hyperplastic Polyp (HP) � 75-90% of serrated polyps � Throughout colon, distal predominance � Lower crypts narrow without dilatation and serration � Serration may be in upper half � Lower crypts with proliferative cells 2
5/28/2016 Hyperplastic Polyp Sessile Serrated Adenoma (SSA/P) Subtype � Approximately 10-20% of serrated polyps � Right colon predominance � Architectural rather than cytologic dysplasia � Crypt branching and basal dilatation Mucin-poor � Transverse, L or T shaped crypts � Serration at base, goblet or gastric foveolar cells rather than proliferative cells � No surface cytologic dysplasia � This is the serrated lesion (we previously called them HP) that CRC appears to arise in Microvesicular Goblet cell rich Dilatation and Serration to the Base 3
5/28/2016 TA Small SSA/P HP SSA/P SSA/P 2012: 1 convincing crypt 2010: 2-3 contiguous crypts Rex, Am J Gastroenterol, 2012 Traditional Serrated Adenoma (TSA) Traditional Serrated Adenoma � Rare, 1-2% of CR polyps � Uniform cytologic � Distal predominance dysplasia � Usually villous or � Eosinophilic tubulovillous cytoplasm, centrally � May be focally flat like located nuclei SSA/P � Luminal serration � Surface dysplasia � Ectopic crypts-not � Usually not as high grade sine qua non as TVA � 50% coexist SSA/P, HP or TA/TVA Bettington, Hum Path, 2015; Hafezi-Bakhtiari S, Histopath, 2015; Chetty, J Clin Path, 2015 and 2016 4
5/28/2016 Tubulovillous Adenoma (TVA) What is This Polyp? A. TSA B. SSA/P C. SSA/P with dysplasia D. TVA 73% 23% 2% 1% A. B. C. D. What is This Polyp? What is This Polyp? A. TSA A. TSA B. SSA/P B. SSA/P C. HP C. HP D. Prolapse polyp D. Prolapse polyp 86% 73% 24% 12% 1% 1% 1% 0% A. B. C. D. A. B. C. D. 5
5/28/2016 What is This Polyp? A. TSA SSA/P Differential and Mimics B. SSA/P C. SSA/P with dysplasia D. Prolapse polyp 60% • Other serrated polyps (HP, TSA, mixed polyps) 21% • Prolapse, SRUS 15% • Inflammatory polyp 4% • Serrated crypts and stromal polyp A. B. C. D. Differential Diagnostic Features Differential Diagnostic Features - HP vs. SSA/P � Problems with SSA/P and TSA and clues � Surface cytologic dysplasia (TSA) � Surface may be similar � Villiform architecture (TSA) � Base of crypts with � Ectopic crypts (TSA) serration, dilatation and � Problems with TSA and TVA and clues transverse architecture � Degree of dysplasia (lower in TSA) (SSA/P) � Uniform eosinophilic cytoplasm (TSA) � Mitotic figures upper � Ectopic crypts (TSA) crypts (SSA/P) 6
5/28/2016 Practical Immunohistochemistry for What is This Polyp? Differential Diagnosis � Ki67 A. TSA � MUC6 B. SSA/P � Annexin A10 C. SSA/P with dysplasia � Maspin D. HP with prolapse � Hes1 change � MLH1 � Many others 86% � I do not use IHC � H&E levels, colleagues 12% 2% 0% A. B. C. D. Rectal polyps- Hyperplastic Polyp and/or Rectal Prolapse Prolapse Change Many rectal polyps misdiagnosed as SSA/P; BRAF does not help in differential Huang, Hum Pathol, 2013 7
5/28/2016 Rectal Prolapse TA with Prolapse Inflammatory Polyp Serrated Polyp? 31 32 8
5/28/2016 Ulcerative Colitis with Adenocarcinoma Stromal Polyp Neuromatous polyp (Schwann cell hamartoma) S-100 33 Mucosal Perineurioma Associated with SSA/P � Benign nerve sheath tumor � Associated with serrated polyp 70-80% � EMA weak, Claudin-1 � S100, SMA negative Hornick, Am J Surg Pathol, 2005; Pai, Am J Surg Pathol, 2011; Doyle, Surg Pathol Clin, 2013 35 36 9
5/28/2016 What is This Polyp? Mixed Serrated Polyps- Cytologic Dysplasia Arising in SSA/P � Progression in SSA/P A. TSA � TA or TSA-like B. SSA/P � Loss of MLH1 protein by C. SSA/P with IHC (MMR gene) likely dysplasia due to methylation of MLH1 promoter D. TA 62% 31% 5% 3% Sheridan, Am J Clin Pathol, 2006 A. B. C. D. SSA/P with Dysplasia SSA/P with Dysplasia TA-like TSA-like 10
5/28/2016 What is This Polyp? What is This Polyp? A. TSA A. TA B. SSA/P B. SSA/P C. SSA/P with C. SSA/P with dysplasia dysplasia D. TA D. TA and SSA/P 74% 54% 46% 16% 10% 0% 0% 0% A. B. C. D. A. B. C. D. Clinical and Endoscopic Features of Risk of Colorectal Cancer Colorectal Serrated Polyps Many None/few Number of polyps WHO Prevalence Endoscopy Distribution Malignant Potential Small Size of polyps Large HP Very common Sessile/flat Mostly distal Very low smooth SSA Common Sessile/flat Mostly proximal mucous cap HP Type of polyps SSA Type of polyps Type of polyps SSAd Without D Low With D Significant Site of polyps Right Left TSA Rare Sessile/ Mostly distal Low/Significant pedunculated Cancer risk Lower Higher Lieberman, Gastroenterol, 2012 Modified from Rex, Am J Gastroenterol, 2012 11
5/28/2016 Proposed Endoscopic Surveillance SSA/P- Pitfalls and Misconceptions Histology Size Number Location Interval (yrs) � Not associated with Lynch HP <10mm Any number Rectosigmoid 10 � Do not do mismatch repair stains HP ≤ 5mm ≤ 3 Proximal Sigmoid 10 � Lynch usually has TA not SSA HP Any ≥ 4 Proximal Sigmoid 5 � SSA/P may not have > risk than TA HP >5mm ≥ 1 Proximal Sigmoid 5 � SSA/P with dysplasia may progress fast and need increased surveillance SSA/P or TSA <10mm <3 Any 5 SSA/P or TSA ≥ 10mm 1 Any 3 � Sporadic SSA/P not same risk as SSA/P in Serrated Polyposis Syndrome SSA/P or TSA <10mm ≥ 3 Any 3 SSA/P ≥ 10mm ≥ 2 Any 1-3 SSA/P w/dysplasia Any Any 1-3 Proximal HP >10mm considered SSA by clinicians Rex, Am J Gastroenterol, 2012 46 Would IHC for MMRP be Useful to Classify this Polyp? A. No, it is an H&E diagnosis B. Yes, to distinguish polyp type C. Yes, to confirm dysplasia D. Yes, to confirm LS 97% 1% 1% 0% A. B. C. D. 12
5/28/2016 Link Between SSA and Microsatellite Unstable (MSI) Cancers � Serrated pathway to CRC � Many series/case reports � Epidemiology and H&E � CRC arises in SSA/P � Molecular link to CpG island methylation (CIMP), BRAF mutation and MSI cancers Iino, J Clin Pathol 52,1999; Wynter, Gut 53, 2004; Goldstein, Am J Clin Pathol 119, 2003; Jass, Am J Clin Pathol 119, 2003; Goldstein, Am J Clin Pathol 125, 2006; Sheridan, Am J Clin Pathol 126, 2006 MLH1 Lost with Progression Colorectal Cancer (Simplified) 15% 85% CIN MSI (Chromosome Instability) (Microsatellite Instability) 1% 80+% Dysplasia 2-3% 13% FAP Sporadic Sporadic Lynch Sx SPS? Germline Acquired Epigenetic silencing of Germline mutation Mutation APC, p53, MLH1 by MMR genes, 40-50y. APC, 20y. DCC, K-ras, MLH1 hypermethylation of its LOH…, promoter region, >80y. MSH2 60-70y. MSH6 SSA Adenocarcinoma PMS2 13
Recommend
More recommend