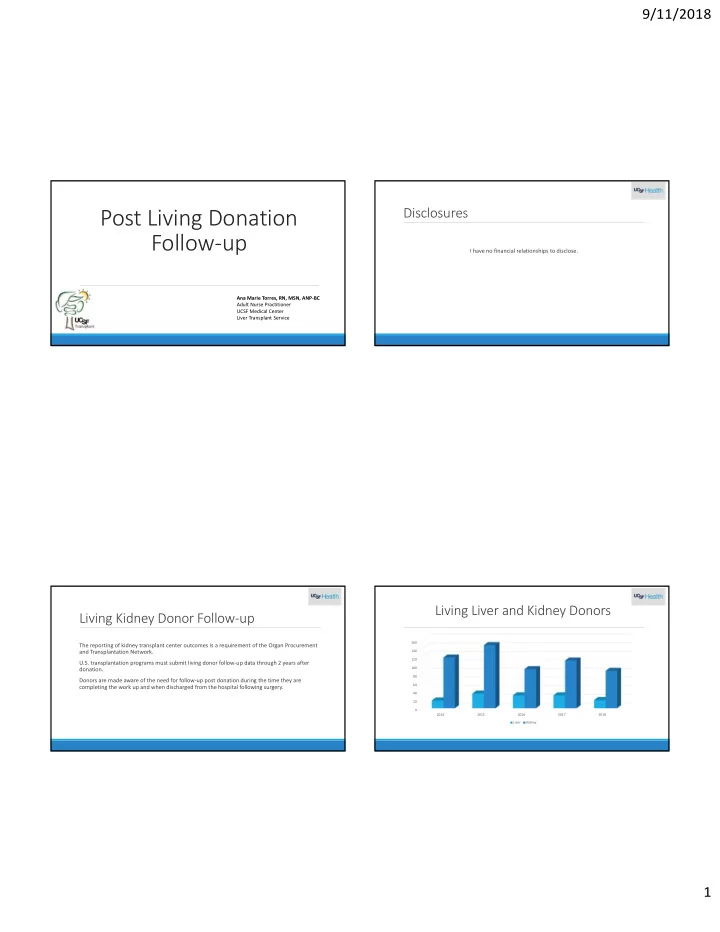
9/11/2018 Post Living Donation Disclosures Follow‐up I have no financial relationships to disclose. Ana Marie Torres, RN, MSN, ANP‐BC Adult Nurse Practitioner UCSF Medical Center Liver Transplant Service Living Liver and Kidney Donors Living Kidney Donor Follow‐up 160 The reporting of kidney transplant center outcomes is a requirement of the Organ Procurement and Transplantation Network. 140 120 U.S. transplantation programs must submit living donor follow‐up data through 2 years after donation. 100 80 Donors are made aware of the need for follow‐up post donation during the time they are 60 completing the work up and when discharged from the hospital following surgery. 40 20 0 2014 2015 2016 2017 2018 Liver Kidney 1
9/11/2018 Post Kidney Donor Follow‐up Post Liver Donor Follow‐up At UCSF, donors are asked to follow‐up with the transplant center one week after surgery and at At UCSF, the follow up for liver donors are seen in clinic one week, two weeks and two months, 6 months, one year and two years. six months and twelve months. The follow up includes: Blood work for serum creatinine The follow up includes: CBC, electrolytes and liver function tests. Urine sample for urine protein and urine creatinine ratio Abdominal ultrasound at two months Clinic visit A Health History Questionnaire Health History Questionnaire Living Donor Follow‐up Live Donor Follow‐up So what are the barriers to donor follow‐up? 2
9/11/2018 Post Living Donor Follow‐up Barriers Post Living Donor Follow Up Benefits Lack of reimbursement to transplant programs for donor follow‐up care Better understanding of the long term health outcomes of living donors Donors do not want to return to the transplant program for medical tests as time passes More information can be provided to prospective living donors about risks Lack of reimbursement to donors for costs associated with follow‐up Improved national trust in the process of living donation Cost of additional medical testing for living donors Improved health for living donors Living donors do not want to be contacted Reduced medical risks associated with kidney donation Donors’ contact information becomes outdated Reduced medical risks associated with liver donation Direct and indirect costs to donors Post Living Donor Follow‐up The Future of Post Living Donor Follow‐up The ASTS has been actively lobbying for a bill to be introduced in Congress that would provide lifetime Medicare coverage for living donors. Research in the field of living donor and kidney donation all agree that donor follow‐up is important. In August, 2018 the U.S. Department of Labor’s Wage and Hour Division issued a new opinion letter confirming living organ donors’ qualification for Family Medical Leave Act protections in Understanding the long‐term medical consequences of living donation remains deficient. response to a request form Congresswoman Jaime Herrera Beautler (R‐WA). The ASTS worked closely with the congresswoman’s office to ensure that living donors are protected in their jobs. Follow‐up needs to be longer than 2 years to better understand the long‐term health outcomes of living donors. (HTN, DM, cardiovascular disease, obesity) H.R. 1270 Living Donor Protection Act of 2017 prohibits discrimination based on an individual’s status as a living organ donor in the offering, issuance, cancellation , coverage, price, or any Providing donors with health insurance as an incentive for kidney donation could make it easier other condition of a life insurance policy, disability insurance policy, or long‐term care insurance to obtain medical follow‐up from their primary care physicians. policy. 3
9/11/2018 Living Donor Follow‐up Summary References Waterman, Amy D., Dew, Mary Amanda, Davis, Connie L., McCabe, Melanie, Wainwright, Jennifer L., Forland, Cynthia I., Bolton, Lee, & The disclosure of information regarding the quality of health care outcomes enforces the Cooper, Matthew. (2013). Living‐ Donor Follow‐Up Attitudes and Practices in U.S. Kidney and Liver Donor Programs. Transplantation, performance standards to improve the quality of care provided to donors. 95(6)883‐888. To understand the long‐term health outcomes of living donors. Newell, K.A., Formica, R.N., & Gill, J.S. (2016). Engaging Living Kidney Donors in a New Paradigm of Postdonation Care. American Journal of Transplantation, 16, 29‐32. The information on the health of donors is needed to care for individual donors and for the Wainwright, Jennifer L., Robinson, Amanda M., Wilk, Amber R. , Klassen, David K., Cherikh, Wida S., & Stewart, Darren E.(2018). Risk of education of potential donors so that they can make informed decisions about donating. ESRD in prior living kidney donors. American Journal of Transplant, 18, 1129‐1139. Donors directly help their recipients is indisputable. Brown, Robert S., Smith, Abigail R., Dew, Mary Amanda, Gillespie, Brenda W., Hill‐Callahan, Peg, &Ladner, Daniela P. (2014) Predictors of Donor Follow‐up After Living Donor Liver Transplantation. American Association for the Study of Liver Diseases, 20, 967‐976. Donors help society by reducing the economic and social costs of caring for patients with ESRD Murad, Sarwa Darwish, Fidler, Jeff L., Poterucha, John J., Sanchez, William, Jowsey, Sheila G., Nagorney, David, Rosen, Charles B., & and ESLD. Heimbch, Julie K. (2015). Longerm Clinical and Radiological Follow‐up of Living Liver Donors, 22, 934‐942. 4
Recommend
More recommend