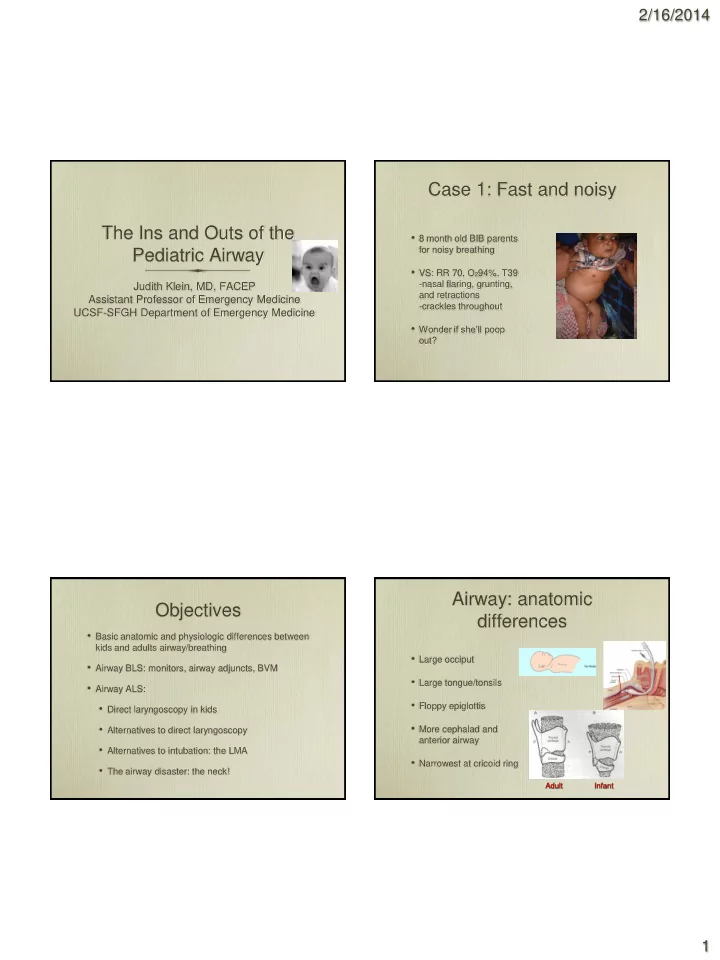
2/16/2014 Case 1: Fast and noisy The Ins and Outs of the • 8 month old BIB parents for noisy breathing Pediatric Airway • VS: RR 70, O 2 94%, T39 -nasal flaring, grunting, Judith Klein, MD, FACEP and retractions Assistant Professor of Emergency Medicine -crackles throughout UCSF-SFGH Department of Emergency Medicine • Wonder if she’ll poop out? Airway: anatomic Objectives differences • Basic anatomic and physiologic differences between kids and adults airway/breathing • Large occiput • Airway BLS: monitors, airway adjuncts, BVM • Large tongue/tonsils • Airway ALS: • Floppy epiglottis • Direct laryngoscopy in kids • More cephalad and • Alternatives to direct laryngoscopy anterior airway • Alternatives to intubation: the LMA • Narrowest at cricoid ring • The airway disaster: the neck! Adult Infant 1
2/16/2014 Conditions that can cause Anatomic differences airway problems • Secretions easily block airway • Genetic/congenital: - trisomy 21, Pierre-Robin • Increased aspiration risk • Infection • Flexible thoracic cage: - croup, epiglottitis, abscess retractions/paradoxical breathing • Rheumatologic • Immature respiratory - JRA muscles: tire easily • Burns/trauma • Obligate nasal breathers <6 months A/B Physiologic differences Physiologic differences • High metabolic rate high • Limited respiratory O2 consumption reserve • MV=RR x TV • Apnea time to 90% O 2 • TV limited by thorax size sat after pre- oxygenation: • MV more RR dependent -6 minutes adult/adolescent • RR with respiratory - 90 seconds if <6 months* compromise or with increased metabolic demand *Patel, et al. Can J Anesth 1994. 2
2/16/2014 Case 2: Let’s use the Airway BLS propofol • Monitors: -Basic: pulse ox, HR, BP • 2 year old with distal - ETco2 key to early radius fracture detection of hypoventilation • Propofol for reduction • (Re-)Positioning: -large occiput • O2 sat to 92%, sonorous -roll under shoulders respirations • Suction: • What now? -secretions/blood easily obstruct airway -nasal sxn in infants Case 3: Code 3 call-14 mo old Airway BLS asthma • Paramedic ringdown: 14 mo old severe asthma, declining RR and HR: Doc, should we • Jaw thrust-->airways adjunct: tube him? -NP: nares to tragus -OP: mouth to angle of jaw • OOH success with intubation: *< 3 yrs old: 56%! *3-8 yrs: • BVM: 61%! -bridge of nose to cleft of chin -2 person technique • No difference in survival or - lift face to mask: don’t push neuro outcome ETT or BVM mask onto face • 2010 ALS: BVM preferred over intubation if transport *Gausche, et al. JAMA 2000. time short 3
2/16/2014 Airway ALS: RSI or TED? (Tie Em He’s circling the toilet bowl.. Down) (? • RSI !: even in neonate (2x greater success, fewer complications) • In ED, pt sleepy, RR • Paralytic choice ? 14, O2 90%, minimal air movement -Succinylcholine: black box due to K, arrhythmias, card arrest • Asthma meds? vs -Rocuronium: longer acting but • Silastic therapy? reversal agent soon (Sugammadex-acts in 1-2 min)* • Working on the IV... • IO time *Puhringer, Anesthesiology 2008. Airway ALS: RSI Airway ALS: The tube • Atropine ? -bradycardia risk • Narrowest portion of -< 1 year old or if use airway below cricoid succinylcholine ring • Cricoid pressure ? • Who needs a cuff? -reduce gastric air/aspiration but also distort airway • Uncuffed under 6 - 2010 ALS: “safety and value not clear” so let up if needed years unless air leak control critical: • NC O2 during intubation?: -kid data scant but why not? 4
2/16/2014 What if he didn’t look so bad... Non-invasive ventilation • Indications: >1 yr, • Non-invasive ventilation? hypoxic, not in resp failure • CPAP or PPV - pneumonia, bronchiolitis, asthma • Face mask, nasal • Contraindications: AMS, mask* or helmet* vomiting, impaired gag, • Improve gas exchange advanced resp failure, and decrease work of HD instability breathing • Limited studies: Try it early Direct laryngoscopy? Maybe Case 4: Is he 5 or 15? not... • Alternatives to the ETT • 5 yo morbidly obese • LMA Classic fever/SOB x 2 days • LMA Proseal • VS: RR 40, O2 88% on NRB, HR 150 • LMA Supreme PE: tripoding, BS with crackles both bases, • LMA Fastrach: intubating(>10yrs) no wheeze • Combitube (>4 feet tall) • What next? • Alternatives to direct laryngoscopy • Lighted stylet (e.g. Trachlight) 5
2/16/2014 LMA: Love My Airway LMA • Classic : -basic model, reusable - • LMA Supreme: 90% 1st pass/99% overall -single use (lower in infants) -curved like fastrach for -complication rate <10% easy insertion (infants ) -gastric port • Proseal : 2nd generation • LMA Fastrach -reusable, gastric port, bite -intubating block ->30kg only -better seal than Classic -slightly lower 1st pass success Direct laryngoscopy: so retro! Airway video games • Stylets : slip tube over • Glidescope, Airtraq, Storz • Lighted stylet (e.g. Trachlight, • See around the corner: No need Tube Stat): for direct line of sight to see -good with secretions but not glottis/place tube edema/masses -look for light mid neck • Great for c-spine patients • Optical stylet (e.g Shikani, • Secretions/blood are a killer Levitan): -shapeable with fiberoptic • Tendency to focus on monitor scope - oral trauma secretions are the enemy -use w/ or w/o laryngoscope 6
2/16/2014 Do video games work Can’t intubate/Can’t ventilate!! better? • 200 kids 3 mo-17 yrs direct • 8 month old with laryngoscopy vs. respiratory distress Glidescope • Respiratory arrest! • Improved view but -BVM: unable to ventilate -Reposition/suction/oral • 97 vs 90% 1st pass airway still unable to success ventilate • Took longer (24 vs 36 • What next??? sec) Kim, et al, Br J Anesth 2008 When is it time to go to the Airway disaster plan neck? • BVM • Can’t intubate/can’t ventilate • Laryngoscopy • All attempts at oxygenation are failing • Child not waking up soon • LMA • Vitals deteriorating due to hypoxia • GO TO THE NECK 7
2/16/2014 Needle cricothyroidotomy Big guys vs. little guys • Extend neck with roll, adipose • Cricothyroid membrane: towards mandible, quick prep -13 x 12 mm (adult) vs • Any tracheal site below -2.5 x 3 mm (neonate)!! thyroid cartilage • Landmarks tough • 14G angiocath on 10cc • >8 years: surgical or syringe (or Ventilation Catheter < VBM, Germany > ) percutaneous approach • Insert until free flow air then • <8 years: needle/catheter advance catheter only Trans-tracheal ventilation Pediatric airway pitfalls • Jet ventilation • Failure to monitor properly and understand • Pseudo-jet ventilation: airway BLS -Cook tubing connects to angiocath and 15 l/min O2 • Failure to anticipate difficult airway and have -Macgyver: cut sideholes range of equipment available into oxygen tubing • Failure to practice alternative techniques • Bag ventilation: - 3.0 ETT adapter - • Prolonged attempts trauma/bleeding in airway 8.0 ETT adapter inserted in 3cc syringe barrel • Spending too long placing IV go to IO • Allow time for passive • Failure to move to the neck when all else fails exhalation-2:1 ratio 8
2/16/2014 9
Recommend
More recommend