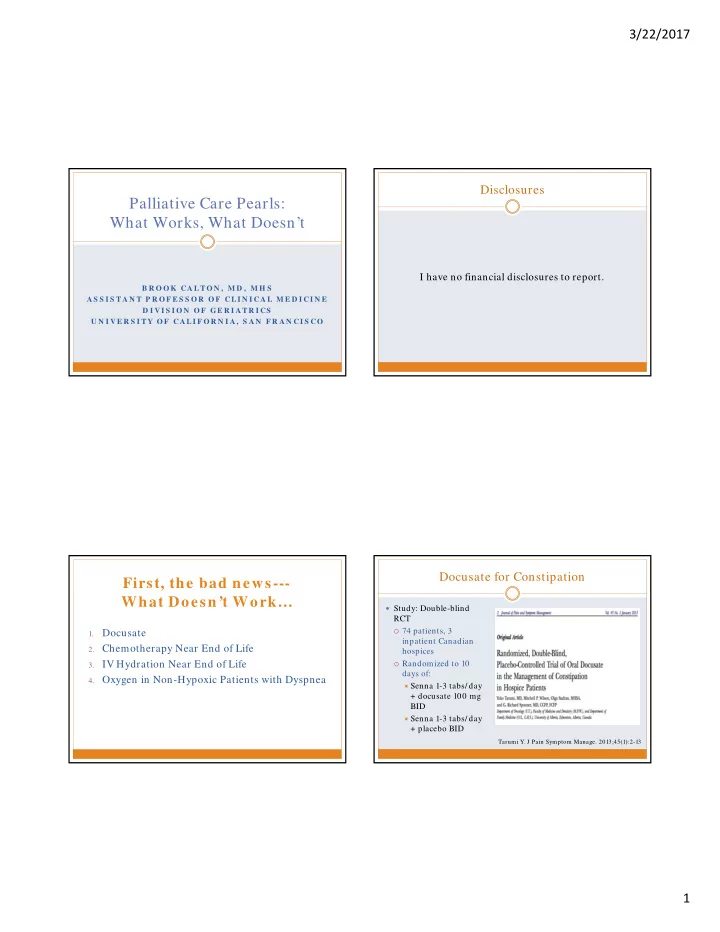
3/22/2017 Disclosures Palliative Care Pearls: What Works, What Doesn’t I have no financial disclosures to report. B R O O K CA L TO N , M D , M H S A S S I S TA N T P R O F E S S O R O F CL I N I CA L M E D I CI N E D I V I S I O N O F G E R I A TR I CS U N I V E R S I TY O F CA LI F O R N I A , S A N F R A N CI S CO Docusate for Constipation First, the bad news--- What Doesn’t Work… Study: Double-blind RCT 74 patients, 3 Docusate 1. inpatient Canadian 2. Chemotherapy Near End of Life hospices 3. IV Hydration Near End of Life Randomized to 10 days of: 4. Oxygen in Non-Hypoxic Patients with Dyspnea Senna 1-3 tabs/ day + docusate 100 mg BID Senna 1-3 tabs/ day + placebo BID Tarumi Y. J Pain Symptom Manage. 2013;45(1):2-13 1
3/22/2017 Study Results Take-Homes Docusate group had marginally larger volume of No appreciable benefit of adding stool p=0.06; stool consistency was slightly different between groups Docusate to Senna in hospice patients No differences in: Average # of bowel movements/ day What works for constipation: Patients’ perceptions of the difficulty or completeness of Always rx laxative with opioid defecation Start with senna, then add Miralax, Lactulose, etc Pain Percent of patients requiring additional bowel intervention Suppository or enema (avoid Fleets) if > 3-4 days (74% placebo; 69% docusate)] Consider Methylnatrexone for opioid-induced Additional issues: tastes horrible, pill burden constipation if above not working Chemotherapy near End of Life Study Results ½ of patients were on chemo at enrollment Goals of chemotherapy Median survival 4 months for patients with Patients with good functional status were more likely metastatic cancer: to receive chemo Live longer 1. Live better 2. Results: Study: Association of No difference in survival chemo in last 6 months Chemo associated with worse QoL for patients with better of life with caregiver- functional status at baseline reported quality of life in last week of life and Think twice about whether to support palliative survival Prigerson HG et al . Jama Oncol 2015; doi:10.1001/jamaoncol.2015.2378 Prigerson HG. Jama Oncol 2015; 1(6):778-784 chemotherapy for patients with metastatic cancer who are near the end of life. 2
3/22/2017 IV Hydration Near End of Life IV Hydration Near End of Life RCT of 129 hospice patients with cancer and mild- Significant controversy moderate dehydration Stopping to eat and drink at end of life is Intervention: normal 1L NS/ day over 4 hours x 4 days Associated with edema, effusions and ascites 100mL NS/ day over 4 hours x 4 days Does not reduce thirst Requires some sort of access/ line Bruera E. J Clin Oncol. 2013; 31, no. 1 111-118 Supplemental Oxygen for Study Results Dyspnea In Non-Hypoxic Patients Palliative oxygen therapy widely used for No stat sig difference in: Survival (21 vs 15 d) dyspnea Symptoms (fatigue, Potential benefits: placebo effect, family myoclonus, sedation, feels like “doing something” hallucinations) Quality of Life Potential burdens: ties patient down, social Both groups noted stigma, uncomfortable, nosebleeds, fire risk subjective improvement in dehydration symptoms Typically best to minimize IVF at end of life. 3
3/22/2017 Supplemental Oxygen Trial Study Results Study: No difference between supp O2 vs RA by NC in: Double-blind RCT Mean AM Breathlessness scores 239 outpatients in US, Australia and UK with life- Mean PM Breathlessness scores limiting illness, refractory dyspnea, and Quality of Life PaO2>55m Hg Randomized to RA or O2 at 2 LPM x 7 days Instructed to use O2 at least 15 hours/ day Compared with RA NC, oxygen by NC provides no benefit for dyspnea in patients who are not hypoxemic. Abernathy A. Lancet 2010;376(9743):784-93 What Works for Dyspnea And now, the good news--- (Other Things) That Work! Treat the underlying cause Pleural effusion, PE, pna, ascites Palliative Care Opioids Low dose, Safe even in COPD Skillful and Sensitive Communication Position Advance Care Planning Breathing training Fan and/ or fresh air Cold cloth to face Acupuncture in COPD Ekstrom M. Ann Am Thoracic Soc 2015; 12(7):1079-92 Bausewein C. Cochrane Database Syst Rev. 2008(2):CD005623 4
3/22/2017 Palliative Care Old Paradigms of Palliative Care Engagement Specialized medical care for patients with serious illness and their families Focuses on providing relief from the symptoms and stress of a serious illness Team-based approach No prognostic or treatment limitations Hospice is a type of palliative care A Medicare Benefit (Part A) For patients with prognosis less than six months who have chosen to forgo life-prolonging interventions Can be offered at home, SNF, or other residential facility Palliative Care Benefits Current Paradigm of Palliative Care Engagement Quality Im proves Reduction in symptom burden Improved quality of life Longer length of life Increased family satisfaction Better family bereavement outcomes Care matched to patient centered goals Costs Decrease Hospital costs decrease Need for hospitalization/ ICU decreases Condition appropriate for palliative care may or may NOT progress to death 5
3/22/2017 Study Results Early Palliative Care Intervention Baseline characteristics did Study: not differ between groups Non-blinded, RCT (single site) Intervention group: Ambulatory patients with Better QOL scores newly diagnosed metastatic Less depression NSCLC More documentation of Immediate PC + onc vs onc resuscitation preferences Primary outcome: change in Less aggressive care at the QOL at 12 weeks end of life Lived two months longer Temel J. N Engl J Med 2010;363:733-42 Yet, patients and families report… Skillful and Sensitive Communication Not enough: Patients and families want their providers to: Contact with physician 78% Bring up end of life issues Emotional support (pt): 51% Be available and willing to talk AND listen Info re: dying process: 50% Provide timely and clear information Emotional support (family): 38% Encourage questions Help with pain/ dyspnea: 19% Patients tend to want: Prognostic information And a lack of: For bad news to be delivered sensitively Coordination Control over the timing of conversation Access Anticipatory Guidance Active participation in decision-making, but desire recommendations Butow Support Care Cancer 2002 Assurance Gold Intern Med J 2009 Steinhauser J Pain and SxMgmt 2001 Teno et al. JAMA 2004;291:88-93 . Wenrich Arch Int Med 2001 6
3/22/2017 In general… Audience Poll The biggest barrier for me in having conversations about We spend a lot of time talking serious illness/ end-of-life with my patients is: But sometimes, not enough 1. Knowledge (of how to have the conversation) We interrupt a lot 2. Time We miss emotional cues 3. Money (I can’t or don’t know how to bill) We lack education and confidence 4. Personal Discomfort - Fear of Taking Away Hope or Damaging the Relationship Tulsky Ann Int Med 1998 Anderson JGIM 2011 Marvel JAMA 1999 5. None, this stuff is easy Levinson JAMA 2000 Ury Acad Med 2005 Unique Opportunity in Primary Care Key Communication Tools Systematic review of 126 articles: 77 directly addressed Asking for Permission primary care, 26 addressed specific populations, 23 addressed general topics Strengths Weaknesses • Continuity • Deficits in knowledge, • Duration skills, and attitudes • Trust • Discomfort with • Ability to coordinate prognostication across settings • Lack of clarity about the • Unique ability to have appropriate timing and these in an iterative initiation of manner conversations Lakin J. JAMA Int Med 2016; 176(9):1380-1387 7
3/22/2017 Key Communication Tools Improving Communication Ask for Permission VitalTalk Respond to Emotion (www.vitaltalk.org) N ame “It sounds like you’re frustrated.” U nderstand “It must be hard going through this alone.” R espect “I am so impressed by your commitment to your mother.” S upport “I’ll be with you through all this.” E xplore “Tell me more.” Practice: “ I feel like life is spiraling out of control” Utilize Silence “Say something empathic and then just shut up.” Improving Communication (cont.) Readings Hashim MJ. Patient-Centered Communication: Basic Skills. Am Fam Physician.2017 Jan 1;95(1):29-34. Ngo-Metzger Q, August KJ, Srinivasan M, Liao S, Meyskens FL Jr. End-of-Lifecare: guidelines for patient-centered communication. Am Fam Physician. 2008 Jan15;77(2):167-74. Eprognosis (ucsf.eprognosis.edu) 8
Recommend
More recommend