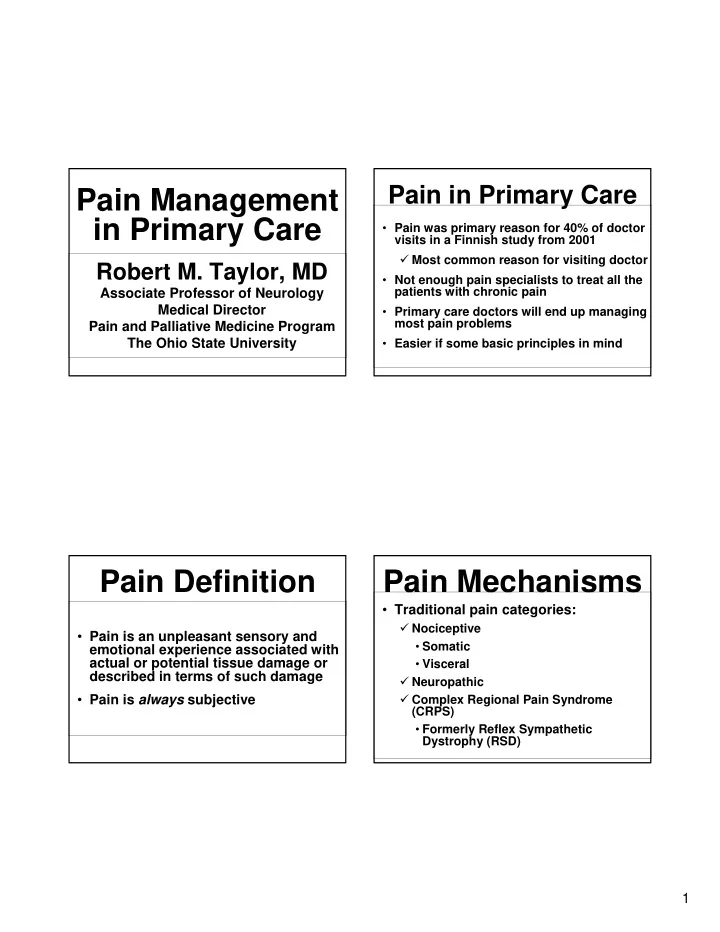
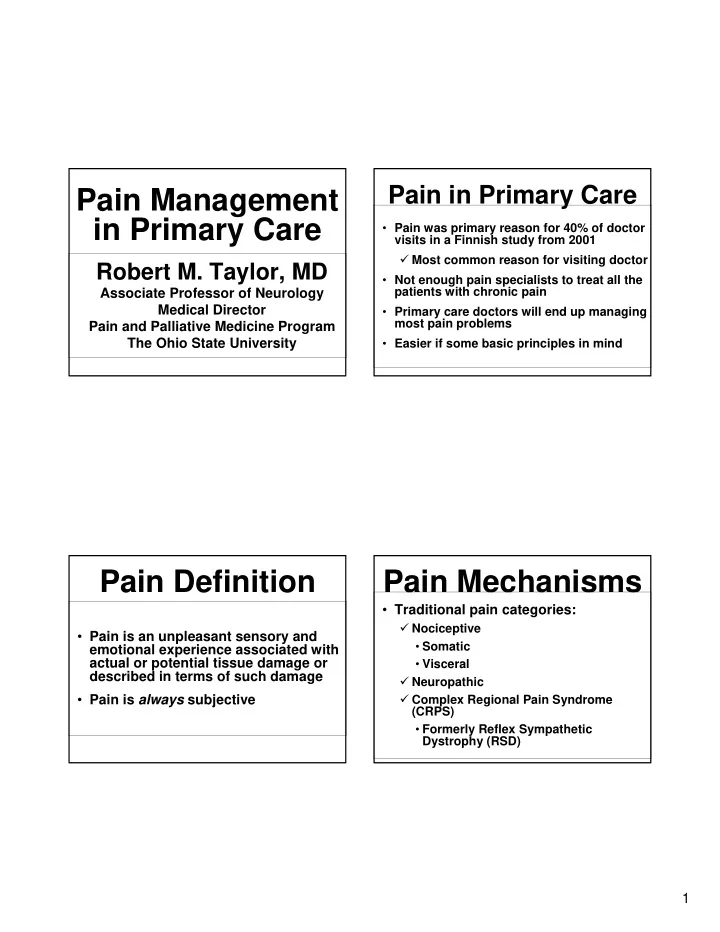
Pain in Primary Care Pain Management in Primary Care • Pain was primary reason for 40% of doctor visits in a Finnish study from 2001 � Most common reason for visiting doctor Robert M. Taylor, MD • Not enough pain specialists to treat all the patients with chronic pain Associate Professor of Neurology Medical Director • Primary care doctors will end up managing most pain problems Pain and Palliative Medicine Program The Ohio State University • Easier if some basic principles in mind Pain Definition Pain Mechanisms • Traditional pain categories: � Nociceptive • Pain is an unpleasant sensory and • Somatic emotional experience associated with actual or potential tissue damage or • Visceral described in terms of such damage � Neuropathic � Complex Regional Pain Syndrome • Pain is always subjective (CRPS) • Formerly Reflex Sympathetic Dystrophy (RSD) 1
Chronic Malignant Pain vs. Acute vs. Chronic Pain Chronic Non-malignant Pain • Acute pain • Pathophysiology is similar � Well-defined, temporal pattern of onset • Difference in longevity may be important � Associated with subjective and • Malignant pain associated with diminishing function due to disease progression objective physical signs and with hyperactivity of the autonomic nervous • Risks of long-term opiate therapy may be system more significant in benign pain � Usually self-limited � Emphasize non-pharmacological treatments � Responds to analgesic treatment and/or treatment of underlying disease � Emphasize enhancing function & QOL Chronic Non- Acute vs. Chronic Pain malignant Pain • Chronic pain � Pain that lasts for longer than 3-6 months • Evaluate pain etiology carefully • Or longer than normal healing process • Use non-pharmacolgical modalities � Nervous system dysregulation results in • Assess risk factors for addiction & abuse hypersensitivity to pain � Use non-opioids if possible • Spontaneous generation & perpetuation of pain • Emphasize improved function & QOL as • Adaptation of the autonomic nervous system primary goal of therapy, NOT pain relief • Lack of objective signs and symptoms � Consider using available tools to assess � Pain becomes a problem in itself � Involve family, work, etc. to monitor � Changes in personality, lifestyle, & function 2
Chronic Non- Understanding Addiction malignant Pain • Physical dependence • Use formal pain agreement for informed consent prior to prescribing opioids � Normal and expected phenomenon � Include consent for UDS � Due to decrease in endogenous • Initiate opioids as a therapeutic trial analogues � Discontinue (taper or detox) if ineffective or significant aberrant behaviors noted � Characteristic withdrawal syndrome � Consider referral for addiction evaluation & treatment � Usually not a serious problem • Monitor function & QOL as primary goal • If symptoms improve, drug can be weaned • Monitor UDS & OARRS reports Aberrant Drug-taking Behaviors Understanding Addiction Steven D. Passik, PhD • Probably more predictive • Probably less predictive • Addiction � � Selling prescription drugs Aggressive complaining about need for higher � Prescription forgery doses � Psychological/behavioral phenomenon � Stealing or borrowing � Drug hoarding during another patient’s drugs periods of reduced � Compulsive use causing physical, � Injecting oral formulation symptoms � � psychological, or social harm to the Obtaining prescription Requesting specific drugs drugs from non-medical � patient Acquisition of similar sources drugs from other medical � Concurrent abuse of sources � Continued use despite such harm related illicit drugs � Unsanctioned dose � Multiple unsanctioned escalation 1-2 times � Compulsive actions to acquire the drug dose escalations � Unapproved use of the � Recurrent prescription drug to treat another � Rare in terminally ill patients losses symptom � Reporting psychic effects • Often note increased level of functioning not intended by the clinician 3
Pain Assessment Understanding Addiction Mnemonic • “Pseudo-addiction” • P – provoking, palliating factors � Prevalence uncertain & controversial • Q – quality of pain � Occurs in patients • R – radiation (from where to where) • Whose symptoms are under-treated • Who fear medication will be arbitrarily • S – severity withheld � May exhibit aberrant behaviors • T – temporal course • Hoarding, hostility, manipulation, lying, etc. � Long term, including onset & short term Intensity of Pain • Pain is not measurable, hence we must rely of patients subjective descriptions Pain Assessment • Several rating scales of intensity are available, utilizing numbers, colors, faces � Mild, moderate, severe, excruciating • Can suggest objective standard 4
WHO Pain Ladder Summary 3 Severe • Evaluation of the patient with pain should include: Morphine � Determination of the clinical characteristics of Hydromorphone 2 Moderate the pain by careful history and exam Methadone • Define etiology if possible Fentanyl Acetaminophen + � Determination of the mechanism of the pain Codeine Oxycodone 1 Mild • Nociceptive, neuropathic, or CRPS Acetaminophen + ± Acetaminophen Oxycodone � Classification as either acute or chronic pain ± NSAIDs Acetaminophen ± NSAIDs • Malignant vs. non-malignant chronic pain ± Adjuvants NSAIDs ± Adjuvants ± Adjuvants WHO Ladder Concepts • By the mouth Pharmacologic • By the clock • By the ladder Treatment of Pain • For the individual • Attention to detail Note: Adjuvants may 1) enhance analgesia, 2) treat concurrent symptoms, or 3) provide independent analgesia for specific types of pain 5
Clearance Sensitivity to Opioids Considerations • 90-95% of opioids cleared in urine • Type of Pain Opioid Responsiveness • Dehydration, renal failure, severe hepatic failure may cause decreased clearance Nociceptive • Morphine has an active metabolite (M-6-G) that - Somatic + + + may accumulate in patients with renal - Visceral + + insufficiency Neuropathic + � Consider an alternate opioid in patients with renal failure, (e.g. oxycodone, hydromorphone, fentanyl) Opioid Pharmacology Opioid Adverse Effects • Conjugated in liver Uncommon • Excreted via kidney (90%–95%) Common Bad dreams / hallucinations • First-order kinetics **Constipation** Dysphoria / delirium • Cmax after Dry mouth Myoclonus / seizures � po ≈ 1 h Nausea / vomiting Pruritus / urticaria � SC, IM ≈ 30 min Sedation Respiratory depression � IV ≈ 10-15 min Sweats Urinary retention • Half-life at steady state Opioid-induced neurotoxicity � po / pr / SC / IM / IV ≈ 3-4 h 6
Opioid-Induced Opioid Constipation Neurotoxicity (OIN) • Common to all opioids • Neuropsychiatric syndrome � Effects on CNS, spinal cord, myenteric plexus • Cognitive dysfunction � Easier to prevent than treat • Delirium � Diet usually insufficient • Hallucinations � Bulk forming agents not recommended • Myoclonus/seizures • Hyperalgesia/allodynia - generalized OIN: Treatment Opioid Constipation • Opioid rotation • Stimulant laxative � Senna, bisacodyl, glycerine, casanthranol, etc � Reduce opioid dose (?) • Combine with a stool softener • Hydration � Senna + docusate sodium • Benzodiazepines • Osmotic laxative for refractory cases • Ketamine, psychostimulants � MOM, lactulose, sorbitol, Miralax • Non-opioid therapy 7
Opioid Naïve Patients Equianalgesic Dosing PO/SL Name IV/SQ/IM • Start at a low dose & titrate to pain relief 30 Morphine 10 30 Oxycodone N/A • Opioid doses can be titrated up by 30%- 30 Hydrocodone N/A 100% or more each day for severe pain 7 Hydromorphone 1.5 N/A Fentanyl 0.1 • Until an effective baseline dose can be 300 Meperidine * 100 established, it is best to avoid sustained release or transdermal systems since they cannot be rapidly and accurately titrated. Fentanyl Patch 100 μ g/hr roughly equals Morphine 200 mg po/24hr *DO NOT USE Routine Oral Dosing Routine Oral Dosing Immediate Release Extended Release Formulations Formulations • For adults >60kg, in moderate to severe pain, start with oral morphine 5 mg • Improves compliance, adherence equivalent • May want to start lower for elderly, • Dose q 8, 12, or 24 h (product specific) e. g. 2.5 mg oral equivalent � Don’t crush or chew tablets • Hydrocodone, morphine, hydromorphone, oxycodone oral dosing • May adjust dose every 2–4 days � Dose q 3 to 4 h � Once steady state reached � Adjust dose daily for severe pain 8
Alternate Routes Breakthrough dosing • Use immediate-release opioids • Transmucosal � 5%–15% of 24 hour dose • Feeding tubes � Maximum time interval based on half-life � Minimum time interval based on C max • Rectal ≈ q 1 h • po / pr • Transdermal ≈ q 30 min • SC, IM • Parenteral ≈ q 10–15 min • IV • Intraspinal • Do NOT use extended-release opioids Treating Pain – Ideal Changing Opioids • Use equianalgesic tables, do not guess ! Over Medication � Analogous to changing from IV to oral antibiotics - be precise! Ideal Breakthrough Medication Around- the-Clock • Incomplete cross-tolerance Medication � Start with 50%–75% of published equianalgesic dose • More if uncontrolled pain, less if Persistent Pain adverse effects � Provide adequate breakthrough dosing e m T i 9
Recommend
More recommend