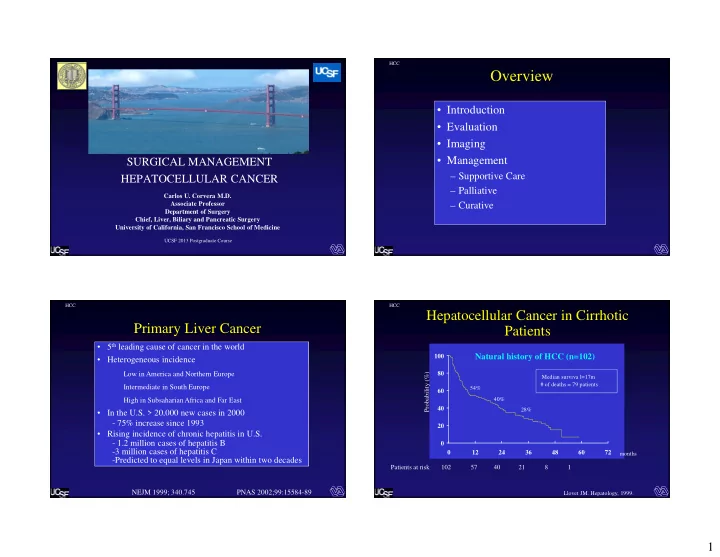
HCC Overview • Introduction • Evaluation • Imaging • Management SURGICAL MANAGEMENT – Supportive Care HEPATOCELLULAR CANCER – Palliative Carlos U. Corvera M.D. Associate Professor – Curative Department of Surgery Chief, Liver, Biliary and Pancreatic Surgery University of California, San Francisco School of Medicine UCSF 2013 Postgraduate Course HCC HCC Hepatocellular Cancer in Cirrhotic Primary Liver Cancer Patients • 5 th leading cause of cancer in the world Natural history of HCC (n=102) 100 • Heterogeneous incidence 80 Low in America and Northern Europe Probability (%) Median surviva l=17m # of deaths = 79 patients Intermediate in South Europe 60 54% 40% High in Subsaharian Africa and Far East 40 28% • In the U.S. > 20,000 new cases in 2000 - 75% increase since 1993 20 • Rising incidence of chronic hepatitis in U.S. 0 - 1.2 million cases of hepatitis B -3 million cases of hepatitis C 0 12 24 36 48 60 72 months -Predicted to equal levels in Japan within two decades Patients at risk 102 57 40 21 8 1 NEJM 1999; 340.745 PNAS 2002;99:15584-89 Llovet JM. Hepatology, 1999. 1
HCC HCC Imaging of the Liver HCC Carcinogenic Sequence GOALS OPTIONS Neoplasia Dysplasia • Ultrasound 3- 50 months – Contrast • Lesion characterization • Computed • Lesion detection • Solitary- encapsulated • Multifocal /multinodular, Tomography • Regenerative Nodule • Staging for potential Early HCC Bilobar (size criteria) – Multi Detector Technology resection • Dysplastic Nodule • Diffusely Infiltrative/ Invasive • Magnetic Resonance • Assessment of – Ultrafast Imaging therapeutic response – Diffusion Weighted – Eovist HCC HCC HCC Hepatocellular Carcinoma Duplex Ultrasound • Receives its blood supply from the hepatic artery and trans left consists of abnormal hepatocytes arranged in a trabecular, sinusoidal pattern • Expansive tumors: well differentiated and relatively slowly growing; usually well defined • Invasive tumors: poorly differentiated with aggressive growth patterns; usually ill defined • Invades vascular structures, more commonly the portal vein than the hepatic vein; arterioportal shunting is characteristic Left Hepatic Vein Tumor Involvement 2
HCC HCC Hepatocellular Carcinoma Portal Vein Thrombosis long Trans trans MHV Long RHV Trans IVC Long HCC HCC Multiphasic CT-Scan Computed Tomography Example 1 HCC Characteristics on CT Advances • Hyperdense enhancement • Spiral during arterial phase • Multidetector Spiral CT • Lesion become lower in i.e “ Washout ” • Major Advances Example 2 density during later phase – 3D Reformatting – CT Angiography 3
HCC HCC HCC MR Imaging MRI • Conventional Imaging – T1 (anatomy) – T2 (pathology) – Flow (MR angiography) • Others – Fat (lesion characterization) – Metabolites (spectroscopy) – Tissue oxygen consumption (fMRI) – Diffusion & perfusion (ischemia, necrosis) – Temperature (monitoring therapy) HCC HCC MR Imaging Management of HCC Gadolinium Portal Venous Pre-Gadolinium Gadolinium Arterial Multidisciplinary: Hepatologist, Oncologist, Diagnostic Radiologist, Interventional Radiologist and Surgeons • Supportive Care • Palliative Therapies – Transarterial embolization (TAE) or Chemoembolization (TACE) – Percutenous Ablative Procedures Delayed 1 min Delayed 5 min Coronal – Hormonal treatments/ Immunotherapy – Antiproliferative agents – Radiation Therapy: external and transarterial • Curative (Radical) Therapies – Surgical resection (5-40%) – Liver Transplantation (CLT/LDLT) – Ablative procedures : Percutaneous ethanol injection (PEI) /Radiofrequency 4
HCC HCC Ablation Tools Percutaneous Ethanol Injection (PEI) • Chemical – ETOH – Acetic Acid – Chemotherapy – Experimental protocols • Thermal – RF ablation – Cryoablation – Laser – Microwave •Need to be able to locate the lesion •Should be < 3cm HCC HCC Principles of Embolization Therapy PEI 6 months later “ sparing ” normal liver • Dual blood supply to liver facilitates preferential delivery of embolic/toxic agents to tumor • Access to hepatic artery allows for targeted regional therapy, minimal systemic effect 5
HCC HCC CT Scan Patient Selection for TAE or TACE NON-CONTRAST EARLY ARTERIAL Tumor • Unresectable disease – Multiple small tumors – Large >5 cm involving critical structures Tumor • Liver only/dominant disease • Adequate hepatic functional reserve Labs: T.bili< 2.0; Cr. < 1.5, Plts> 75 • Most are palliative procedures- HCC HCC Single Lesion Embolization Single Lesion Embolization Tumor Tumor Tumor Post-embolization Selective Left HA Celiac -- Scout Left HA Left HA 6
HCC HCC Multiple / Bilobar Disease Multiple / Bilobar Disease Left-sided tumors HCC HCC Patient Selection for Thermal Embolization Procedures Ablations --Complications-- • Non-operative potential --quality of life issues. • Occlusion of vessels to non-target organs • Unresectable – cystic artery � chemical cholecystitis • Anatomy – often not good for RFA either – right gastric artery � gastric or duodenal ulceration – GDA � Acute pancreatitis • Extending limits of resection – Biliary Necrosis (dilated intrahepatic ducts) • Tumor Characteristics: Size and Distribution • Catheter related vascular injuries – Hemorrhage – Number < 3 – Dissections – Aneurysms – Size < 3cm , < 5 cm – Puncture site hematoma • Liver Abscess • Assuming perfect accuracy should be as good as • Liver Decompensation resection • Post-Embolization Syndrome 7
Thermal Ablation – HCC HCC RFA/Microwave – Techniques Guidance • Percutaneous: CT scan/ US • Ultrasound • General anesthesia not always necessary • Less trauma/pain/recovery • Some tumors not anatomically feasible • No operative staging • Computed Tomography • Laparoscopic /Thoracoscopic • Minimally invasive surgery • Better staging • Able to move organs from heat source • Magnetic Resonance Imaging • Open • Optimal staging • ? Optimal probe placement • Able to combine with resection HCC HCC Laparoscopic Technique CT – Guidance Umbilical Vein 8
HCC HCC HCC HCC Preoperative MRI RFA/Microwave – Local failure • Increasing size • Tumor vascularity • Proximity to vascular structures • Surgical versus percutaneous technique 9
HCC HCC Post-RFA MRI Curative Therapies 6 months 14 months • Surgical Resection • Liver Transplantation • Ablative Therapies HCC HCC Two Problems Hepatic Resection in Cirrhotic Livers: “ …Partial hepatectomy for tumors occurring in The Early View •Chronic Liver Disease & HCC Tumor necessary to control hemorrhage. ” •Underlying cirrhosis limits cirrhotic livers should not be done unless it is aggressive treatments. •Surgery remains the only chance •Liver Tumor Survey-- 1974 for long-term survival. - Mortality rate was 58% in cirrhotic patients (n =26). •Majority of patients are not suitable for operation. Foster JM, Berman MM,. Solid Liver Tumor,1977;p. 62-104 10
HCC HCC Preoperative Interventions Preoperative Assessment of Liver Function Test Author Contraindication for Resection • Prevention of Variceal Bleeding Varices Child-Pugh Franco Score > 8 – Sclerotherapy Serum alanine Noun ALT > twofold upper limit of norm – Transjugular intrahepatic Indocyanine green Lau retention rate at 15 minutes > 15 % portosystemic shunt (TIPS) Makuuchi retention rate at 15 minutes > 10 % Fan retention rate at 15 minutes > 14 % • Arterial Embolization Wu retention rate at 15 minutes > 10 % – Diagnostic Angiogram Umbilical Vein Hasegawa retention rate at 15 minutes > 10 % – Reduces tumor bulk Hemming clearance < 5 mL/min/kg • Sequential Arterial and Portal Kanematsu retention rate at 15 minutes > 20 % Embolization ( double vascular Urea nitrogen synthesis Paquet < 6 g/day embolization). Portal Vein Pressure Bruix HVPG > 10mm Hg Ercolani G MEGX <25 ng/ml * Lidocaine (MEGX) test MEGX <25 ng/ml * Grazi, *alone not considered an absolute contraindication to resection HCC HCC Right Hepatic Artery Embolization 3 Weeks After Right Hepatic Arterial Embolization Sequential Arterial and Portal Embolization Replaced Right Hepatic Artery Post embolization 11
HCC HCC Right Portal Vein Embolization Right Portal Vein Embolization Sequential Arterial and Portal Embolization Occluded PV Occluded PV Occluded PV Occluded PV HCC HCC Repeat Right & Left Hepatic Arterial CT Scan Embolization 6 weeks after PVE, 9 & 3 weeks after TACE Recanulated Branch Left HA Branches from Replaced RHA 12
Recommend
More recommend