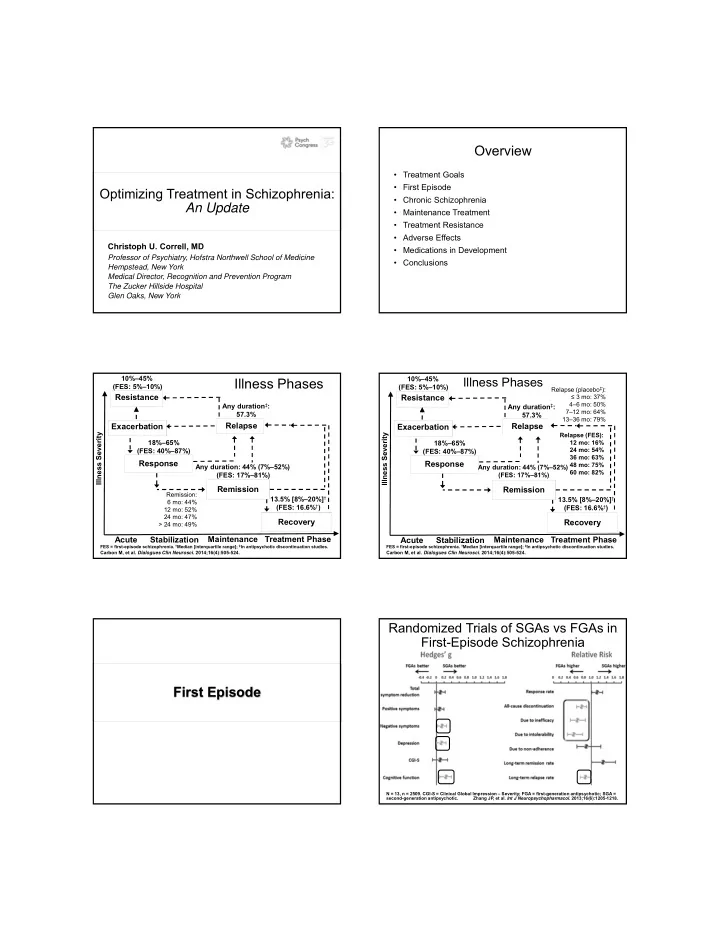
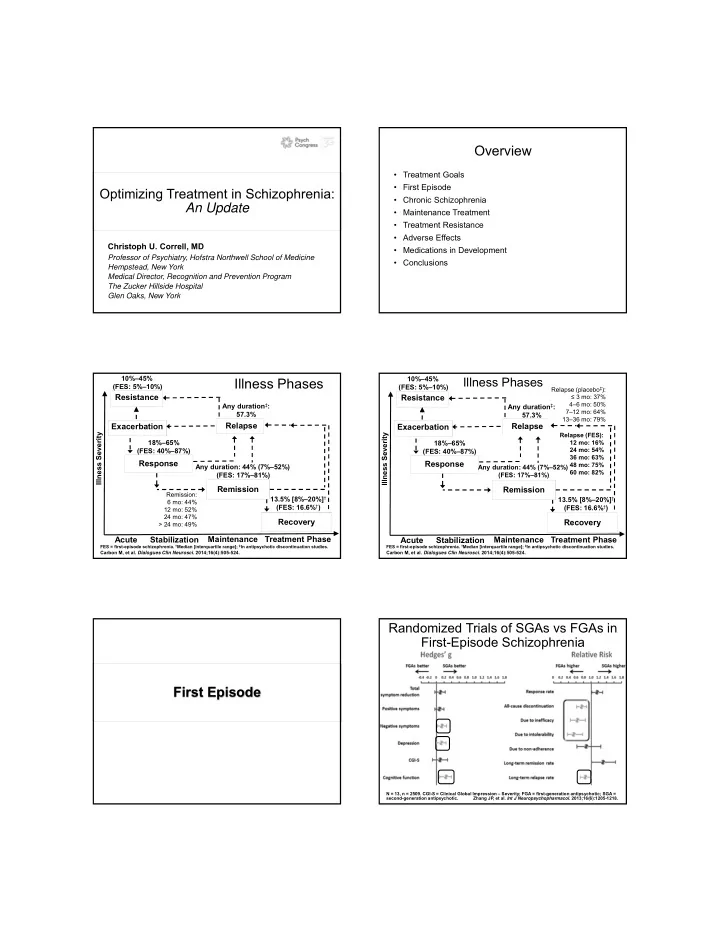
Overview • Treatment Goals • First Episode Optimizing Treatment in Schizophrenia: • Chronic Schizophrenia An Update • Maintenance Treatment • Treatment Resistance • Adverse Effects Christoph U. Correll, MD • Medications in Development Professor of Psychiatry, Hofstra Northwell School of Medicine • Conclusions Hempstead, New York Medical Director, Recognition and Prevention Program The Zucker Hillside Hospital Glen Oaks, New York 10%–45% 10%–45% Illness Phases Illness Phases (FES: 5%–10%) (FES: 5%–10%) Relapse (placebo ‡ ): Resistance Resistance ≤ 3 mo: 37% 4–6 mo: 50% Any duration ‡ : Any duration ‡ : 7–12 mo: 64% 57.3% 57.3% 13–36 mo: 79% Relapse Exacerbation Exacerbation Relapse Illness Severity Relapse (FES): Illness Severity 18%–65% 18%–65% 12 mo: 16% (FES: 40%–87%) 24 mo: 54% (FES: 40%–87%) 36 mo: 63% Response Response 48 mo: 75% Any duration: 44% (7%–52%) Any duration: 44% (7%–52%) 60 mo: 82% (FES: 17%–81%) (FES: 17%–81%) Remission Remission Remission: 13.5% [8%–20%] † 13.5% [8%–20%] † 6 mo: 44% (FES: 16.6% † ) (FES: 16.6% † ) 12 mo: 52% 24 mo: 47% Recovery Recovery > 24 mo: 49% Acute Stabilization Maintenance Treatment Phase Maintenance Treatment Phase Acute Stabilization FES = first-episode schizophrenia. † Median [interquartile range]; ‡ In antipsychotic discontinuation studies. FES = first-episode schizophrenia. † Median [interquartile range]; ‡ In antipsychotic discontinuation studies. Carbon M, et al. Dialogues Clin Neurosci . 2014;16(4):505-524. Carbon M, et al. Dialogues Clin Neurosci . 2014;16(4):505-524. Randomized Trials of SGAs vs FGAs in First-Episode Schizophrenia First Episode N = 13, n = 2509. CGI-S = Clinical Global Impression – Severity; FGA = first-generation antipsychotic; SGA = second-generation antipsychotic. Zhang JP, et al. Int J Neuropsychopharmacol . 2013;16(6):1205-1218.
Recovery after an Initial Schizophrenia Episode– A Randomized Comparison of Aripiprazole and Risperidone for the Early Treatment Program (RAISE-ETP) Acute Treatment of FES and Related Disorders: 3-Month Outcomes • First large scale, double-masked, randomized comparison of aripiprazole (5–30 mg/day) vs risperidone (1–6 mg/day) in FES • N = 404 (394 with cardiometabolic data) • 198 patients, 15–40 years old, with schizophrenia, schizophreniform disorder, • Age : 15–40 years schizoaffective disorder, or psychosis NOS • Diagnoses : Schizophreniform disorder, schizophrenia, • Antipsychotic treatment ≤ 2 weeks lifetime • 12-week RCT yielded no difference in: schizoaffective disorder, psychotic disorder NOS, acute – Positive symptom response rate (ARI = 62.8% vs RIS = 56.8%, P = .61) psychotic disorder – Time to response (8.0 vs 8.2 weeks) • < 6 months antipsychotic treatment – Change in total ( P = .32) or positive symptoms ( P = .96) or CGI-S ( P = .57) • Cluster randomized assignment of 34 centers to – Body weight gain integrated care (NAVIGATE) or community care • Superiority of risperidone (mean dose: 3.2 mg/day) for – Less akathisia ( P = .03), but only early on in the trial (weeks 1–4) • Treatment and follow-up for ≥ 2 years • Superiority of aripiprazole (mean dose: 14.8 mg/day) for • Primary outcome : Quality of life – Negative symptoms: Avolition-apathy ( P = .03) • Secondary outcomes : Service utilization, cost, – Depressed mood ( P = .02) – Total cholesterol ( P = .003), LDL-cholesterol ( P < .01), fasting glucose ( P = subjective well-being, relapses, hospitalization, recovery, .03) cardiometabolic health – Prolactin levels ( P < .0001). ARI = aripiprazole; RIS = risperidone; LDL = low-density lipoprotein; NOS = not otherwise specified; RCT = randomized controlled trial. Robinson DG, et al. Schizophr Bull . 2015;41(6):1227-1236. Kane JM, et al. J Clin Psychiatry . 2015;76(3):240-246. Demographics NAVIGATE Adjusted for Cluster Design Team-based NAVIGATE Community Care P value Shared decision making Age and Gender Strength and resiliency focus Age (mean) 23.5 23.2 Psychoeducational teaching skills Males (%) 77.6 66.2 .05 Motivational enhancement teaching skills Race Collaboration with natural supports White (%) 65.9 49.9 African American (%) 25.4 44.1 4 components Other (%) 8.7 6.0 1. Psychopharmacology – COMPASS Role Functioning 2. Individual Resiliency Training (IRT) In school (%) 14.9 25.5 .03 3. Family psychoeducation Working (%) 12.6 16.6 4. Supported employment/education Prior Hospitalization (%) 76.2 81.6 .05 Kane JM, et al. J Clin Psychiatry . 2015;76(3):240-246. Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372. NAVIGATE Participants Stayed in Treatment Longer Quality of Life Scale Fitted Model Time to Last Mental Health Visit ( P = .009) Group by Time Interaction ( P = .015) DUP by Time Interaction ( P = .003) DUP = duration of untreated psychosis; QLS = Quality of Life Scale. Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372. Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372.
% With Any Work or School Days / Month PANSS Total Score Change over 2 Years (Group by time interaction: P = .044) Group by Time Interaction : P = .016 DUP by Time Interaction: P = .043 Median DUP = 74 weeks. Months PANSS = Positive and Negative Syndrome Scale. Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372. Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372. First-Episode Schizophrenia: Time to First Psychiatric Hospitalization (Difference between treatments, P = .75) Key Points • First-episode patients are generally more treatment responsive • They require lower doses (~ 50%) • They are more sensitive to side effects • Relapse is very common • While acute efficacy might be similar with FGAs and SGAs, relapse and treatment discontinuation seem to be higher with FGAs • Multidisciplinary interventions focusing on engagement, treatment continuation, relapse prevention, physical health, and functional recovery are paramount Kane JM, et al. Am J Psychiatry . 2016;173(4):362-372. Multiple Treatments Meta-Analysis Aim • Create hierarchy for 15 antipsychotic drugs Multi-episode / Chronic • Efficacy and major side effects • Direct and indirect comparisons • Includes some treatments without a European Union license for schizophrenia (sertindole, iloperidone, zotepine, ziprasidone, asenapine) Data set • 212 RCTs Network of comparisons for efficacy • Acute schizophrenia • 43,049 participants • Mean illness duration : 12.4 years • Mean age : 38.4 years Leucht S, et al. Lancet . 2013;382(9896):951-962.
Magnitude PANSS Total Change on Placebo over Forrest Plot: Efficacy of Antipsychotics vs Placebo Time in Trials of Acute Schizophrenia The differences in efficacy between non-clozapine, first- line antipsychotics were small: Standardized mean differences: 0.0–0.33, median = 0.11 Antipsychotics differed substantially in side effects: Standardized mean differences: 0.11– 1.52, median = 0.34 (body weight) and 0.49 (prolactin) 1, 2, or 3 asterisks: Significant separation from placebo; **Significant separation from agents with 1 asterisk; ***Significant separation from all other agents; a: Only superior to lurasidone and iloperidone; b: Only superior to iloperidone; SMD +/- 95% CIs. Leucht S, et al. Lancet . 2013;382(9896):951-962. Alphs L, et al. Int J Neuropsychopharmacol . 2012;15(7):1003-1014. What is the Importance of Relapse Prevention? Maintenance 1. Harrison G, et al. Br J Psychiatry . 2001;178:506-517. 2. Herings RM, et al. Pharmacoepidemiol Drug Saf . 12(5):423-424. 3. Lieberman JA, et al. Neuropsychopharmacology . 1996;14(Suppl 3):13S-21S. 4. Lieberman JA, et al. Psychiatr Serv . 2008;59(5):487-496. 5. Kane JM. J Clin Psychiatry . 2007;68 Suppl 14:27-30. Antipsychotics vs Placebo for Clinical Predictors of Poor Outcomes in Relapse Prevention in Schizophrenia the Long-Term Course of FES* *Based on longitudinal first-episode samples. Depot antipsychotics reduced relapse (RR 0.31, 95% CI 0.21–0.41) more than oral drugs (0.46, 0.37–0.57; P = .03). In a meta- Carbon M, et al. Dialogues Clin Neurosci . 2014;16(4):505-524. regression, drug-placebo advantages decreased with study length. Leucht S, et al. Lancet . 2012;379(9831):2063-2071.
Recommend
More recommend