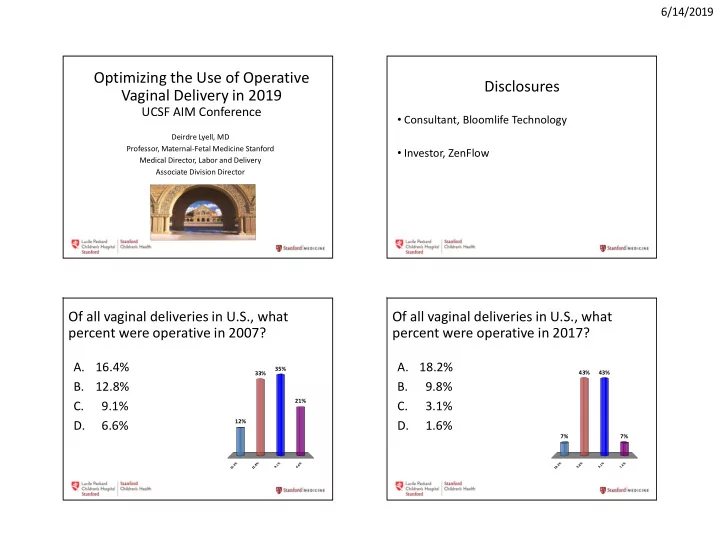
6/14/2019 Optimizing the Use of Operative Disclosures Vaginal Delivery in 2019 UCSF AIM Conference • Consultant, Bloomlife Technology Deirdre Lyell, MD Professor, Maternal-Fetal Medicine Stanford • Investor, ZenFlow Medical Director, Labor and Delivery Associate Division Director Of all vaginal deliveries in U.S., what Of all vaginal deliveries in U.S., what percent were operative in 2007? percent were operative in 2017? A. 16.4% A. 18.2% 35% 43% 43% 33% B. 12.8% B. 9.8% 21% C. 9.1% C. 3.1% 12% D. 6.6% D. 1.6% 7% 7% % % % % % % % % 4 8 1 6 2 8 1 6 . . . 6 2 9 . 6 . 8 9 . 3 . 1 . 1 1 1 1
6/14/2019 Perinatal/maternal outcomes not improved Objectives Repeat CD • Examine the rate of and reasons for cesarean deliveries in the U.S. Primary CD • Explore patterns of use of operative vaginal delivery throughout the U.S. and over time • Explore indications and outcomes of operative vaginal delivery VBAC Accreta: Accreta: 1/2,510 1/333-1/500 Caughey AB, et al. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014;210:17-93 Cesarean rates by state, 2010 Caughey AB, et al. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014;210:17-93 2
6/14/2019 Hospital Variation in Cesarean Rate Healthy People 2020 goals • 2009 data, 593 U.S. hospitals • 10% reduction in incidence of: • Nationwide Inpatient Sample • Primary cesareans: 26.5% to 23.9% • Repeat cesareans: 90.8% to 81.7% • Cesarean rates: 7.1% to 69.9% • Reductions are from 2007 cesarean rates • Low-risk women: 2.4% to 36.5% • Speculate: variation in practice patterns drives difference https://www.healthypeople.gov/2020/topics- objectives/topic/maternal-infant-and-child-health/objectives Kozhimannil et al, Health Affairs, March 2013 Indications for primary cesarean Incidence operative vaginal delivery (OVD) • Labor arrest: 34% • Decreasing: • Abnormal/indeterminate • 2007: 6.6% of vaginal deliveries FHT: 23% • 2013: 4.9% • Malpresentation: 17% • Merriam AA et al. Trends in operative vaginal delivery, • Multiple gestation: 7% 2005-2013. BJOG 2017;124(9):1365 • Suspected macrosomia: • 2017: 3.1% 4% • Forceps 0.5% • Maternal-fetal: 5% • Vacuum 2.6% • Preeclampsia: 3% • Martin et al., Births 2017, Natl Vital Stat Rep • Maternal request: 3% 2018;67(8):1 Obstetric Care Consensus No. 1: Safe Prevention of the Primary Cesarean Delivery. Obstetrics & Gynecology. 123(3):693-711, March 2014. . (Data from Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol 2011;118:29-38.) 3
6/14/2019 Change over time, forceps 2005-2013 Change over time, vacuum 2005-2013 2017: vacuum 2.6% 2017: forceps 0.5% Martin et al., Births 2017, Natl Vital Martin et al., Births 2017, Natl Vital Stat Rep 2018;67(8):1 Stat Rep 2018;67(8):1 Merriam AA et al. Trends in operative vaginal Merriam AA et al. Trends in operative vaginal delivery, 2005-2013. BJOG 2017;124(9):1365 delivery, 2005-2013. BJOG 2017;124(9):1365 Forceps: use by region 2007-2013 Regional variation Midwest: highest forceps rates • Does this matter? NE and West: lowest rates • Fundamental principle of quality control and assessment: unnecessary/unexplained variation in a process or product generally demonstrates poor quality Clark et al. Variation in the rates of operative delivery in the United States. Am J Obstet Gynecol. 2007;196(6):526 e1 Merriam AA et al. Trends in operative vaginal delivery, 2005-2013. BJOG 2017;124(9):1365 4
6/14/2019 Tremendous variability within regions Vacuum: use by region 2007-2013 Midwest: highest vacuum rates; South: lowest Merriam AA et al. Trends in operative vaginal delivery, 2005-2013. BJOG 2017;124(9):1365 Clark et al. Variation in the rates of operative delivery in the United States. Am J Obstet Gynecol. 2007;196(6):526 e1 If you practice obstetrics: in the last If you practice obstetrics: in the last year, month, have you performed, participated have you performed, participated in, or in, or supervised an operative vaginal supervised an operative vaginal delivery? delivery? 57% A. Yes A. Yes 91% 43% B. No B. No 9% s o e N Y s o e N Y 5
6/14/2019 Forceps in California, 2008-2012 Risks OVD vs. unplanned cesarean • 1,557,039 vaginal births, 276 hospitals • Published incidence of risk varies widely • Forceps: 0.3% of vaginal births • Dependent on indication, operator experience, • 21% (59 hospitals): no forceps station, head position, instrument • 80% hospitals: <5/year • OVD from mid-pelvic station (0 to +1), OT or OP • Largest volume hospital (a teaching hospital): positions, vs. low (>+2) or outlet (scalp visible) almost 14% of state volume OVD: • higher failure (increased cesarean) • 16 highest volume hospitals: 5.8% of all • higher complications (increased neonatal injury) hospitals, 50% of all forceps deliveries • requires greater skill • Blumenfeld Y et al., unpublished data OVD and birth injury Risks OVD vs. unplanned cesarean • Forceps: 1.1% • Intracerebral hemorrhage (ICH): vacuum vs.: • Forceps: OR 1.2 (95% CI 0.7-2.2) • Vacuum: 0.8% • Cesarean during labor: OR 0.9 (95% CI 0.6-1.4) • Two data sets: 1989-93, 1995-98 • Spontaneous delivery: lowest rate of IVH • Abnormal labor is likely the risk factor Demissie K, et al. BMJ, 2004 Jul 3;329(7456):24-9 Effects of Mode of Delivery in Nulliparous Women on Neonatal Intracranial Hemorrhage. Towner D, Gilbert WM. Et al. N Engl J Med, 341 (1999), pp. 1709-1714 • No significant change in birth injury over time • Seizure, IVH, subdural hemorrhage: forceps vs.: • 2005 forceps: 2.0/1000. 2005 vacuum: 2.0/1000 • Vacuum: OR 0.60 (95% CI 0.40-0.90) • 2013 forceps: 3.6/1000. 2013 vacuum: 2.9/1000 • Cesarean: OR 0.68 (95% CI 0.48-0.97) • Limitations of a large dataset? • FAVD associated with less adverse neonatal neurologic outcome • 1995-2003 dataset, NY Merriam AA et al. Trends in operative vaginal delivery, 2005-2013. BJOG 2017;124(9):1365 Werner EF et al. Obstet Gynecol, 118 (2011), pp. 1239-1246 6
6/14/2019 Modified by Modified by operator skill operator skill Forceps: -more 3 rd /4 th degree Vacuum: tears -less vaginal birth -vaginal trauma success -birth injuries, seizures -cephalohematoma Vacuum: Forceps: -fewer perineal -greater vaginal tears birth success Indications Operative Vaginal Delivery “Operative vaginal delivery in the second stage of labor by experienced and well-trained physicians • Prolonged second stage should be considered a safe, acceptable • Suspicion of immediate or potential fetal alternative to cesarean delivery. Training in, and ongoing maintenance of, practical skills related to compromise operative vaginal delivery should be encouraged.” • Shortening the second stage for maternal benefit ACOG Practice Bulletin No. 154 Summary: Operative Vaginal Delivery. Committee on Practice Bulletins—Obstetrics Obstet Gynecol. Caughey AB, et al. Safe prevention of the primary cesarean 2015;126(5):1118 delivery. Am J Obstet Gynecol 2014;210:17-9 7
6/14/2019 Prerequisites for Operative Vaginal Delivery Contraindications • Complete dilation • Ruptured membranes • Unengaged fetal head • Engaged fetal head • Unknown position of the fetal head • Known head position • Suspected bone mineralization disorder (e.g. osteogenesis imperfecta) • Estimated fetal weight performed • Bleeding disorder (e.g. alloimmune thrombocytopenia, • Adequate anesthesia hemophilia or von Willebrand disease) • Maternal bladder emptied • Lack of provider experience • Informed consent • Inability to perform emergency cesarean delivery • Willingness to abandon procedure; back up plan in place ACOG Practice Bulletin No. 154 Summary: Operative Vaginal Delivery. Committee on Practice Bulletins—Obstetrics Obstet Gynecol. 2015;126(5):1118 Cautions against Other care • Routine episiotomy: • Midline: increased risk of rectal/anal sphincter injury • Alert neonatal care providers: observation for potential • Mediolateral: poor healing and prolonged discomfort complications from OVD • Sequential use of forceps/vacuum • Document station and position at time of forceps/vacuum application (ACOG performance • OVD if provider feels chance of success is low measure) • Ongoing attempt if no appropriate descent • Document time of vacuum application, duration, pulls, • High forceps pop offs • Vacuum < 34 weeks • Vacuum “pop-offs” 8
6/14/2019 Optimizing the Use of Operative Vaginal Delivery in 2019 UCSF AIM Conference Deirdre Lyell, MD Professor, Maternal-Fetal Medicine Stanford Medical Director, Labor and Delivery Associate Division Director 9
Recommend
More recommend