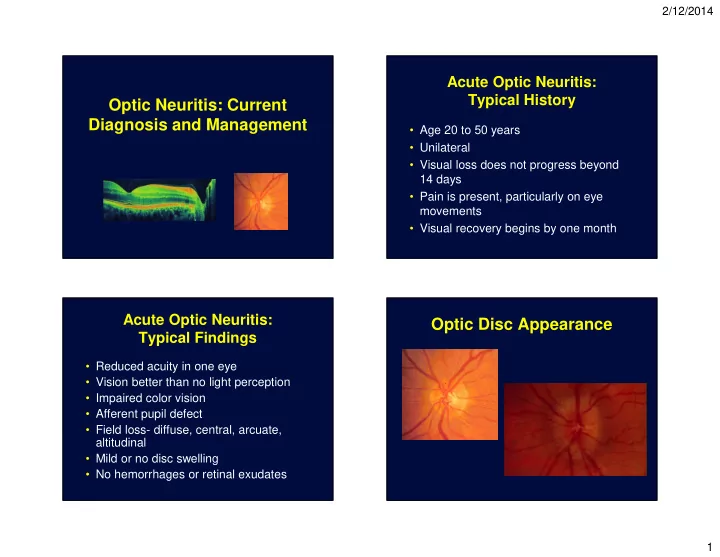
2/12/2014 Acute Optic Neuritis: Typical History Optic Neuritis: Current Diagnosis and Management • Age 20 to 50 years • Unilateral • Visual loss does not progress beyond 14 days • Pain is present, particularly on eye movements • Visual recovery begins by one month Acute Optic Neuritis: Optic Disc Appearance Typical Findings • Reduced acuity in one eye • Vision better than no light perception • Impaired color vision • Afferent pupil defect • Field loss- diffuse, central, arcuate, altitudinal • Mild or no disc swelling • No hemorrhages or retinal exudates 1
2/12/2014 Optic Neuritis-Clinical Course • 95% recover to 20/40 or better over several weeks • 50% have some permanent vision loss (contrast sensitivity, color vision, or visual field), particularly with baseline acuity of 20/50 or less Optic Neuritis: Treatment • Current treatment is IV steroids • Vision recovers faster (stops inflammation) • BUT, final vision no better than without steroids • Reduces short term risk of developing MS • No known treatment prevents permanent vision loss, unmet therapeutic need • Most high risk patients are placed on immunomodulatory therapy 2
2/12/2014 Differential Diagnosis (Step 2) Optic Neuritis: Risk of Multiple Sclerosis • Ischemic optic neuropathy (MS) With Normal MRI • Systemic disease • Neuro-retinitis • No pain 0% • Hereditary disorders • Severe disk edema 0% • Disc hemorrhage 0% • NMO • Macular exudate 0% • NLP vision 0% Arch Neurol , 2008. NLP = no light perception Ischemic Optic Neuropathy NEURITIS VS ISCHEMIA NEURITIS ISCHEMIA Age 30’s 60’s Pain 90% 10% Field central altitudinal Fundus retrobulbar – 2/3 swollen 3
2/12/2014 DIFFERENTIAL DIAGNOSIS (Step 2) INFLAMMATORY (Bilateral, vitreous cells, hemorrhages ) Syphilis Sarcoid Lyme Viral Neuroretinitis DIFFERENTIAL DIAGNOSIS(Step 2) HEREDITARY - Nutritional (Bilateral central-cecal scotomas) Leber’s B 1 , B 12 Toxic 4
2/12/2014 Optic Discs, VF and OCT NMO Prognosis: (5 to 10 yrs) Reasons to Distinguish It • 62% have legal blindness in one eye • 50% will need an assistive device Neurology 53:1107,1999 NMO: The Chances NMO Tidbits • Average RNFL thickness ♦ Bilateral- 50% present of NMO present NMO- 63 microns, typical- 88 microns with ON, 20% are bilateral vs 0.4% in Controls- 102 microns ON with MS • About 5% of optic neuritis patients are ♦ Severe acuity loss- < 20/200, about NMO positive 33% • Chronic relapsing idiopathic optic ♦ Recurrent ON- about 20% neuropathy (CRION). Tend to have progression between episodes JNO: 32:154;2012 Neurology 73:302, 2009 5
2/12/2014 Copper Deficiency Optic Neuropathy Step 3- Tests ♦ MRI head with gad (typical or atypical ON) ♦ LP: IgG index, OCB, cells, protein (atypical ON) ♦ NMO IgG (recurrent, bilateral or severe ON) ♦ Leber’s mutations (severe or bilateral ON) ♦ Serological studies-Atypical ON or systemic symptoms-ESR, ANA, ACE, RPR, Lyme, SSA, SSB, ANCA ♦ Retinal Tests-ERG, Fluorescein angiogram, CAR antibodies, OCT ♦ VER: Subclinical ON, can use low contrast Vision and ON as Ideal Models Comparison of Vision Tests • Axonal and neuronal * (1.9, 3.1) MS Patients: n=130 P <0.001 Disease Free Controls: n=90 loss common 2.5 • Odds ratio in Sensitive visual (1.5, 2.2) favor of MS 2.0 P <0.001 function tests (1.3, 1.9) vs. control (1.2, 1.8) P <0.001 P <0.001 status • (95% CI) for Structure-function 1.5 worse vision correlation can be scores RNFL = ganglion cell axons captured by OCT (non-myelinated) 1.0 High Contrast Low Contrast Contrast Color Vision Acuity ~100% Acuity 1.25% Sensitivity Pelli- D15-DS • Unique opportunity Robson to investigate non- * Low contrast acuity charts best distinguish MS patients vs. controls, accounting for age myelinated axons Balcer LJ, Baier ML, Cohen JA, et al. Neurology 2003;61:1367-1373. 6
2/12/2014 Worsening Vision by EDSS Progression Status Defining Visual Change • 2 lines (10 letters) = clinically meaningful change? Rosser et al. Invest Ophthalmol Vis Sci 2003. Balcer, et al. Neurology 2007. • 5-letter change more sensitive for high-contrast visual acuity Beck et al. Ophthalmology 2007. • Change by ≥ 7 letters is beyond test- retest variability for low-contrast acuity, correlates w/ QOL Balcer, Pelak et al. Mult Scler 2000. Galetta et al. Ectrims, 2010 Retinal Nerve Fiber Layer Importance of OCT in Optic Neuritis Imaging by Optical Coherence Tomography (OCT) • Allows structure-function correlations • Significant RNFL loss, acute, 99% by 6 months • Optic neuritis as a model RNFL for testing new therapies Petzold A et al. Lancet Neurology 2010. Henderson et al. Brain, 2010 Figure from Frohman, et al. Nat Clin Pract Neurol 2008;4:664-675. 7
2/12/2014 Quantifying Axonal Loss After OCT in Optic Neuritis Optic Neuritis with OCT • Patients (n=54) with ON, 74% had 20% RNFL loss • Thickness at ≥ 3 months = 78 ± 30 µm in affected eyes • Patients with acute ON (n=54) • RNFL <75 µm vs. ≥ 75 µm predicted visual outcome • Followed for a mean of 13 months • 74% developed significant RNFL thinning 40 50 60 70 80 90 100 110 (20%) in the affected eye 5 Visual Field Mean 0 -5 Deviation (dB) -10 • RNFL values significantly thinner in -15 -20 affected eyes (78 µm) vs. fellow eyes (100 -25 µm, P < 0.0001) -30 -35 Costello F et al. Ann Neurol 2006. Costello F et al. Ann Neurol 2006 Longitudinal Data: RNFL Thinning Relation to Low-Contrast Acuity, for All MS Eyes (n=593) Optic Neuritis History 0 RNFL change from baseline (microns) * Degree of RNFL thinning MS Eyes: n=180 MS ON eyes MS non-ON eyes Disease-free control eyes R N F L th ic k n e s s (m ic r o n s ) significantly greater compared to Disease Free Control Eyes: n=72 0 – 1-year interval 170 -2 n=201 150 P < 0.001 for ON vs. non ON eyes, P = 0.03 for MS non ON vs. controls 130 n=242, p=0.06 110 -4 90 n=109, p<0.001 * 70 -6 50 Overall Temporal Superior Nasal Inferior n=41, p<0.001 * average -8 2 lines low-contrast letter acuity = 7.6 µm RNFL, P < 0.001 0.5 - 1 year >1 - 2 years >2 - 3 years >3 years Follow-up interval, all MS eyes Fisher J et al. Ophthalmology 2006. Talman et al., Ann Neurol 2010. 8
2/12/2014 Retinal Neuronal Atrophy in MS Eyes Low-Contrast Acuity Reflects Axonal Loss Over Time Ganglion cell dropout Inner nuclear layer RNFL thinning from baseline (microns) Neuron dropout No visual loss Loss of 7 or more letters All MS eyes 0 79% of MS patient eyeballs (N=80) had -2 n = 493 GCL dropout and 40% n = 560 had INL (amacrine and bipolar cell) atrophy -4 -6 n = 67, p<0.001 vs. no visual loss Low-contrast letter acuity, 2.5% Green A et al. Brain 2010. Talman L et al. Ann Neurol 2010. MS vs. Controls Spectral-Domain OCT Ganglion Cell Layer RNFL • High resolution Thickness in microns (4-6 µ m) • Segmentation of retinal layers Above courtesy of James Fujimoto, Ph.D. Tan O, …Schuman JS..., et al. Ophthalmology 2009. P values are from GEE models accounting for age and inter-eye correlations 9
2/12/2014 Implications 100 • Subclinical injury is common in MS 80 r = 0.31, P=0.0006 • OCT and LCA are important outcome 60 measures for clinical trials in MS 40 r = 0.49, P<0.0001 • In practice, used to detect subtle atrophy, 20 longitudinal changes and macular 0 changes 60 70 80 90 100 Thickness of GCL+IPL (microns) • Correlates with QOL and MRI measures NEI-VFQ-25 Composite (best QOL = 100 points) Low-Contrast 2.5% (number of letters identified correctly) 95% Confidence Interval on Fitted Line • Unmet therapeutic need for neuroprotective therapy in MS 24 Y.O. WOMAN EXAMINATION Acuity: NLP O.D ♦ Decreased vision over 7 days 20/20 O.S. ♦ No pain upon eye movement Pupil: Right amaurotic Motility: Full 10
2/12/2014 EXAMINATION -MW ♦ Slit lamp exam showed 1+ vitreous cells OD ♦ Tension applanations were 16 OU ♦ Fundus exam revealed the following: LABORATORY ♦ nl lytes, CBC, LFTs ♦ RPR (-), ESR 40, PPD (-), anergy (+) ♦ ANA 1:320, nl complements ♦ (-) anti- dsDNA, -smith, -RNA, -Ro, -La ♦ ACE 53.18 (10-50) ♦ LP:2W 0R protein:29 glucose:59 ♦ nl CXR 11
2/12/2014 COURSE -MW ♦ Conjunctival and lacrimal biopsies showed non-specific chronic inflammation without granulomas ♦ Gallium scan was normal ♦ She was started on steroids and had no improvement ♦ She underwent biopsy of right optic nerve 12
2/12/2014 OPTIC NERVE IN SARCOID ♦ Occurs in 1-5% of pts with systemic disease ♦ Five categories – Primary granuloma of the optic nerve – Papillitis – Retrobulbar optic neuritis – Papilledema secondary to increased ICP – Optic atrophy 20 Y.O. MAN ♦ Decreased vision O.U. ♦ Visual acuity 20/200 O.U. ♦ Fields: centrocecal scotomas 13
2/12/2014 30 Y.O. MAN ♦ Sudden visual loss O.D. ♦ No pain on eye movement Central Serous Chorio- retinopathy OS - OD 14
2/12/2014 72 Y.O. WOMAN EXAMINATION (August 1996) (August 1996) ♦ Progressive visual loss right eye ♦ Acuities: 20/100+ OD, 20/50+ OS ♦ Right periorbital ache ♦ Pupils: sluggish, no APD ♦ No neurologic or constitutional symptoms ♦ Color: no control OU 15
Recommend
More recommend