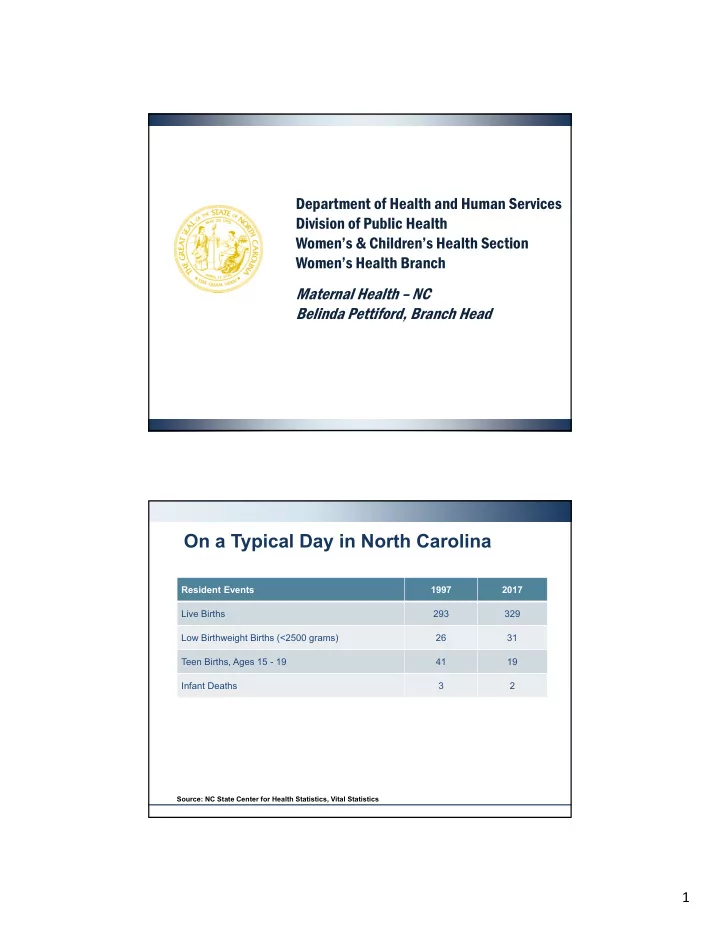
Department of Health and Human Services Division of Public Health Women’s & Children’s Health Section Women’s Health Branch Maternal Health – NC Belinda Pettiford, Branch Head On a Typical Day in North Carolina Resident Events 1997 2017 Live Births 293 329 Low Birthweight Births (<2500 grams) 26 31 Teen Births, Ages 15 - 19 41 19 Infant Deaths 3 2 Source: NC State Center for Health Statistics, Vital Statistics 1
Yearly Totals in North Carolina Resident Events 1997 2017 Live Births 106,949 120,099 % of Low Birthweight Births (<2500 grams) 8.8 9.4 % of Births to Women <18 years 5.5 1.5 Infant Death Rate 9.2 7.1 Source: NC State Center for Health Statistics, Vital Statistics Characteristics of NC Women Giving Birth Percent of women giving birth who ... 80 Had 1st Trimester PNC 71.2 71.3 70.3 70 69 68.6 68.2 67.8 60 Began pregnancy overweight or 53.2 51.8 obese 50.5 50 49.6 49.8 48.5 48 40 30 20 Smoked during pregnancy 10.9 10.6 10.3 9.8 10 9.3 8.9 8.7 0 2011 2012 2013 2014 2015 2016 2017 Source: NC State Center for Health Statistics, Vital Statistics 2
3
4
5
NC Percent of Unintended Pregnancies, 2016 NC Pregnancy Risk Assessment Monitoring System (PRAMS) Total 32.2 By Age <25 years 47.5 25 to 34 years 28.2 35+ years 19.8 By Race White, NH 25.6 Black, NH 45.3 Other, NH 33.4 Hispanic 34.1 Unintended Pregnancy Question: Thinking back to just before you got pregnant with your new baby how did you feel about becoming pregnant? Those who chose “I wanted to be pregnant later” or “I did not want to be pregnant then or at any time in the future” were classified UNINTENDED PREGNANCY. Source: NC State Center for Health Statistics, PRAMS NC Birth Rates for Teens Ages 15 to 17 and 18 to 19 2007 to 2017 Source: NC State Center for Health Statistics 6
Characteristics of NC Infants Percent of Babies Born … 35 by C-Section 30.6 30.4 30.3 30 29.5 29.3 29.4 29.4 25 20 15 Preterm (<37 weeks gestation) 12.1 10.4 10.5 10.2 11.5 9.9 9.8 10 9.4 9.2 9.2 9 8.8 8.8 8.9 at Low Birth Weight (<2500g) 5 at Very Low Birth Weight (<1500g) 1.8 1.7 1.7 1.7 1.7 1.6 1.7 0 2011 2012 2013 2014 2015 2016 2017 Source: NC State Center for Health Statistics, Vital Statistics NC Resident Infant Death Rates, 2007-2017 Racial Distribution Source: NC DHHS North Carolina State Center for Health Statistics 7
NC Infant Mortality Disparity Ratio* 1998-2017 3.50 3.00 2.50 2.00 1.50 1.00 0.50 0.00 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 Ratio 2.57 2.33 2.36 2.52 2.64 2.64 2.56 2.33 2.44 2.42 2.45 2.87 2.40 2.35 2.53 2.52 2.51 2.19 2.68 2.50 *Ratio of Non-Hispanic Black to Non-Hispanic White Infant Mortality Rates Source: North Carolina State Center for Health Statistics, 2017 Infant Mortality Report 8
Number of Pregnancy-Associated Deaths North Carolina Residents 1999 – 2014 35% of all pregnancy associated deaths 1999-2014 80 75 75 75 were pregnancy related 71 70 69 67 70 64 62 58 57 60 56 50 Total Deaths 47 50 38 40 36 30 20 10 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 SOURCE: NC DHHS State Center for Health Statistics, June 2018 NOTE: Data source for ascertainment of pregnancy associated cases are variable over this time period. The criteria for a “pregnancy related case” is not consistent over time. NC is part of a working group with CDC to develop a “best practice” protocol to standardize case ascertainment nationally 9
Cardiovascular leading cause of maternal mortality in NC # of NC Maternal Deaths from 2005-2014 1. Cardiomyopathy (37) + Cardiovascular (27) = 64 2. Infection (27) 3. Pulmonary Embolus (25) # of Maternal Deaths in 2014 1. Cardiomyopathy (3) + Cardiovascular (1) = 4 2. Cerebrovascular Disease (3) 3. Hemorrhage (2) 4. Suicide (2) SOURCE: NC DHHS State Center for Health Statistics, June 2018 Severe Maternal Morbidity (SMM) CY 2016 & 2017 Definition: “A woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy.” 1 Rate per Total Deliveries in NC Number 10,000 Hospitals = 222,113 deliveries Overall SMM 3,834 172 SMM excluding transfusions 1,702 76 1 Say et al., Best Pract Res Cl OB 2009 SOURCE: NC DHHS State Center for Health Statistics August 2018. Report based on Alliance for Innovation on Maternal Health (AIM) Project; http://safehealthcareforeverywoman.org/aim-data/ 10
Some Maternal Health Efforts − Preconception Health Strategic Plan − Perinatal Health Strategic Plan − Maternal Mortality Review Committee − Perinatal Systems of Care Task Force North Carolina Preconception Health Strategic Plan Priority Areas: • Pregnancy Intendedness • Obesity • Substance Abuse • Mental Health • Research • Policy Development • Access to Care 11
North Carolina Preconception Health Strategic Plan Supplement Priority Areas: Life Planning Mental Wellness Access to Services Expanded Priority Population Women AND Men 12
Influencers Life Planning W H AT D O E S Y O U R F U T U R E H O L D ? 13
Mental Wellness G E N E R AL F E E L I N G O F W E L L B E I N G Access to Services M AK E I T E AS Y F O R M E 14
North Carolina Preconception Health Strategic Plan Supplement 2014 CONTRIBUTING PARTNERS North Carolina Perinatal Health Strategic Plan Focus Areas: • Infant Mortality • Maternal Health • Maternal Morbidity • Health of Women & Men of Childbearing Age 15
Social Determinants of Social Determinants of Health (SDOH) Health (SDOH) Image Source: Healthy People 2020 website - https://www.healthypeople.gov/2020/topics-objectives/topic/social- determinants-of-health Life Course Approach Health potential Optimal Life Trajectory Life Trajectory Affected by Inequity Cumulative Pathways Early Programming 16
Health equity is more than t Health equity is more than the absence he absence of healt of health dispar disparit ities ies Health equity is every individual having access to the resources resour ces and oppor opportunit tunities es that promote good health. The Perinatal Health Strategic Plan Goals Goals : • Improving Health Care for Women and Men • Strengthening Families & Communities • Addressing Social & Economic Inequities 17
Goal 1 – Improve Health Care for Women and Men Point 1. Provide interconception care to women with prior adverse pregnancy outcomes Point 2. Increase access to preconception care Point 3. Improve the quality of prenatal care Point 4. Expand healthcare access over the life course Goal 2 – Strengthen families and communities Point 5. Strengthen father involvement in families Point 6. Enhance coordination and integration of family support services Point 7. Support coordination and cooperation to promote reproductive health within communities Point 8. Invest in community building and urban renewal 18
Goal 3 – Addressing social and economic inequities Point 9. Close the education gap Point 10. Reduce poverty among families Point 11. Support working mothers and families Point 12. Undo racism The Perinatal Health Strategic Plan Team 19
Work Groups: - Data and Evaluation - Communications - Community & Consumer - Policy Align and Amplify efforts • Early Childhood Action Plan − Focus ages 0-8 − Healthy Babies goal – Babies across NC from all backgrounds will have a healthy start 20
Few Other Efforts…. • Maternal Mortality Review Committee − Pregnancy associated deaths − Pregnancy related deaths − Legislation – December 1, 2015 − Nine member committee along with Specialty Consultants • Perinatal Systems of Care Task Force − Partnership with NC IOM − Session Law 2018-93 Please join us…. 21
Recommend
More recommend