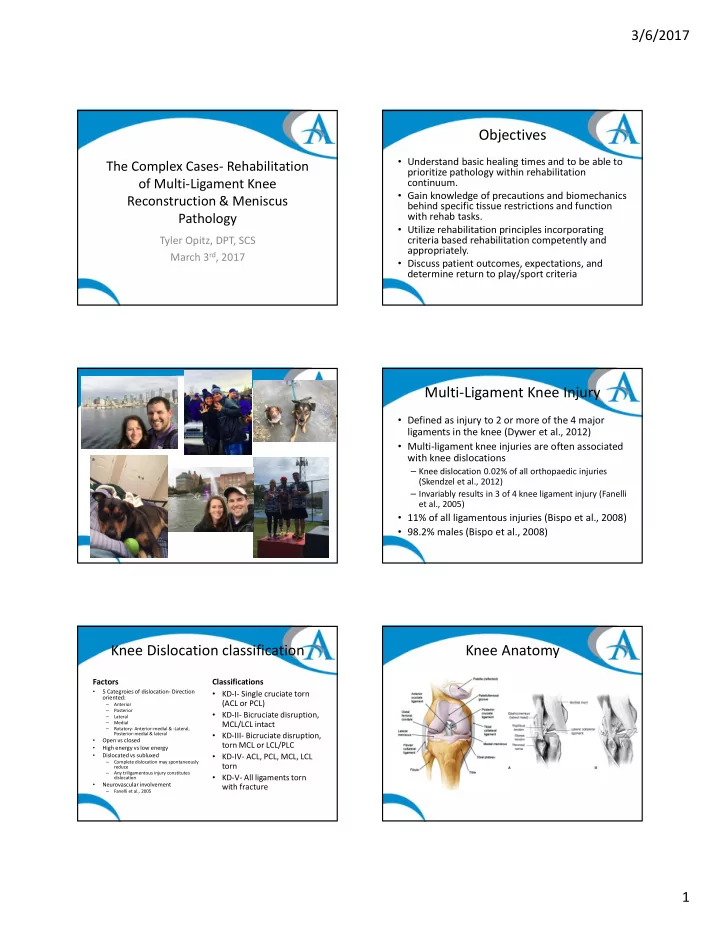
3/6/2017 Objectives • Understand basic healing times and to be able to The Complex Cases- Rehabilitation prioritize pathology within rehabilitation of Multi-Ligament Knee continuum. • Gain knowledge of precautions and biomechanics Reconstruction & Meniscus behind specific tissue restrictions and function with rehab tasks. Pathology • Utilize rehabilitation principles incorporating criteria based rehabilitation competently and Tyler Opitz, DPT, SCS appropriately. March 3 rd , 2017 • Discuss patient outcomes, expectations, and determine return to play/sport criteria Multi-Ligament Knee Injury • Defined as injury to 2 or more of the 4 major ligaments in the knee (Dywer et al., 2012) • Multi-ligament knee injuries are often associated with knee dislocations – Knee dislocation 0.02% of all orthopaedic injuries (Skendzel et al., 2012) – Invariably results in 3 of 4 knee ligament injury (Fanelli et al., 2005) • 11% of all ligamentous injuries (Bispo et al., 2008) • 98.2% males (Bispo et al., 2008) Knee Dislocation classification Knee Anatomy Factors Classifications 5 Categroies of dislocation- Direction • KD-I- Single cruciate torn • oriented: (ACL or PCL) Anterior – Posterior – • KD-II- Bicruciate disruption, Lateral – Medial MCL/LCL intact – Rotatory- Anterior-medial & -Lateral, – Posterior-medial & lateral • KD-III- Bicruciate disruption, Open vs closed • torn MCL or LCL/PLC High energy vs low energy • Dislocated vs subluxed • KD-IV- ACL, PCL, MCL, LCL • Complete dislocation may spontaneously – torn reduce Any triligamentous injury constitutes – • KD-V- All ligaments torn dislocation Neurovascular involvement with fracture • Fanelli et al., 2005 – 1
3/6/2017 Knee Anatomy MOI MOI Complications • Injuries to Popliteal artery, common fibular nerve. (Mills et al., 2004) – Popliteal injury 4.8%- 65% of time • High energy injuries increased incidence – Fibular nerve injury 20% of time (Robertson et al., 2006) Complications Regional Interdependence • Concept of Regional • New definition: • DVT Interdependence is the • Does not limit to • Compartment syndrome relationship of adjacent musculoskeletal system and distant segments – “the concept that a have on motion and patient’s primary stability of body parts of musculoskeletal seemingly unrelated symptom(s) may be directly or indirectly sections that can related or influenced by contribute to pathology impairments from various or have an effect on one body regions and another. (Wannier et al., 2007) systems regardless of proximity to the primary symptom(s).” (Sueki et al., 2013) 2
3/6/2017 Full and adjacent body segment Rehabilitation Considerations assessment 1. Diagnosis/pathology/surgical procedure 2. Severity of tissue damage/invasiveness 1. Involved structures- Ligaments, Menisci, nerve, vascular supply 2. Comorbidities with injury (compartment syndrome) 3. Pain level 4. Duration since injury 5. Tissue healing & quality 6. Patient stage of rehab 7. Current level of function and movement quality 8. Patient Goals 9. Outcomes expectations 10. Psychosocial factors Criteria Based Rehab Principles Car Analogy *PRECAUTIONS GUIDE PROGRESSIONS* • • If you have a flat tire, is Once tissue is at appropriate healing level for activity… • Be sure to fix the • Ability to perform PROGRESSIVE FUNCTIONAL rehab tasks in it because the tire is alignment and treat the • sequence determines progression NOT given amount of weeks bad or is it because the shocks. from surgery Example): Just because they are 12 weeks out DOES NOT alignment was off • mean they should advance to plyometrics if they can’t and/or the shocks bad perform a basic squat causing the tired to – Walking without crutches not based on being 4 weeks post op: • Full quad and hip muscle activation have abnormal wear. • Walk without deviations with 2 crutches -> 1 crutch with and without brace. • Does fixing the tire • Then can walk without brace and crutches solve the problem? Functional tasks are a byproduct of doing basic movement • patterns properly, NOT a product of TIME !!! Grzybowski et al., 2015, Wahoff et al., 2014 Knee Symmetry Model Rehab Concepts • Increasing depth of squat increases SHEAR forces on • Goal is to restore limb symmetry between limbs knee joint • Utilizes subjective and objective measures to • Increased knee extension in closed chain increases determine when successful rehab has concluded. COMPRESSIVE loads on knee joint. (Biggs et al., 2009, Kinzer et al., 2010) • Protect lateral meniscus as has increased translation – Measures Include: with knee motion than medial meniscus • ROM • Bone tunneling has increased risk for stress fractures • Strength compared to healing of traditional fractures • Stability • Avoid loading maturing reconstructed ligaments even • Girth though patient function is improving. • Subjective questionnaire scores 3
3/6/2017 Joint Reaction Forces Rehabilitation Outline Phase I- Acute phase Phase IV- Advanced • • Intermediate phase Manage weight bearing • Decreased knee • Pain management Dynamic strength/ • • flexion proprioception Control swelling • Functional stability Basic ROM – Decreased • • Phase V- Controlled Phase II- Protective phase patellofemoral force • • Activity phase Basic strength – Increased force to hips • Progress ROM Initiate plyometrics • (J Biomech. 2007; 40(16): 3725- • Minimize atrophy 3721) • Initiate running if • Initiate WB and light proprioception appropriate Reinold, 2009 • Phase III- Intermediate phase/ Initiate components of • • Knee deviation increases joint • Progressive strengthening sport specific activities reaction forces and shear on phase cartilage, meniscus and ligamentous Phase VI- Return to • lading Dynamic flexibility activity phase play • Functional movement correction • Performance • Combine functional strength/stability • RTS • Position Resistance Supine/prone No Resistance- Pattern Assist Quadruped No resistance Kneeling Resistance- Pattern Assist Standing Resistance Plisky, 2013 Static Dynamic Double leg Single leg No resistance Resistance In BOS Out of BOS Lower level Higher level Don’t Be Intimidated by This! Post Op/Acute Goals • Minimize pain • Decrease swelling • Protect surgically repaired tissue • Achieve isometric muscle activation • Initiate PROM 4
3/6/2017 Phase I- Acute phase Articular Joints Therapy Minimize pain & swelling • – Patellar mobilizations – Calf & hamstring stretching – Cryotherapy, Compression, Elevation Waste Post op precautions • – Dressing change – Bathing/ADLs – Brace locked in extension Initiate PROM • – to protocol guidelines Limit atrophy • – Quad sets, Multi-angle isometrics – 4-way ankle Phase I- Acute phase Acute Phase • NWB x 5-6 weeks Therapy • 90 degree knee flexion Muscular activation • – BFDB/NMES desirable by week 6 – Glut sets • Minimize compressive – PCL involved-avoid hamstring activation and shear loads on Patient Education • repaired tissue – Pain management strategies – Use of pain pump • Surgery dependent* – Use of home NMES (Edson et al., 2013) – Weight bearing Surgical dependent • – Knee extended locked at 0° Manage expectations • x 3-5 weeks (Fanelli et al., – Rehab progression 2005) – Outcomes/Goals – Sensations in knee Criteria to progress to Phase II Phase II- Basic Strength Goals Rehab Guidelines • Perform active quad set with appropriate Full PROM (surgery Correct faulty individual • • VMO activation and SLR without lag dependent) by end of phase sequences in movement patterns Improve soft tissue flexibility • ROM to appropriate protocol guidelines • Achieve against gravity TRAIN THE HIP HINGE • • • Pain decreased by 50% at rest from highest strength in all LE movements Progress: • through full range rating in phase I Static before dynamic • Ability to sustain contraction through • Kneeling before standing movement • • Tissue healing appropriate for progression to Stable before unstable • Ambulate without AD with • Phase II Unweighted before weighted • symmetrical reciprocal gait by Control before speed • end of phase • Independent with initial HEP Eyes open before eyes closed • MINIMIZE FORCES TO • RECONSTRUCTED TISSUES 5
Recommend
More recommend