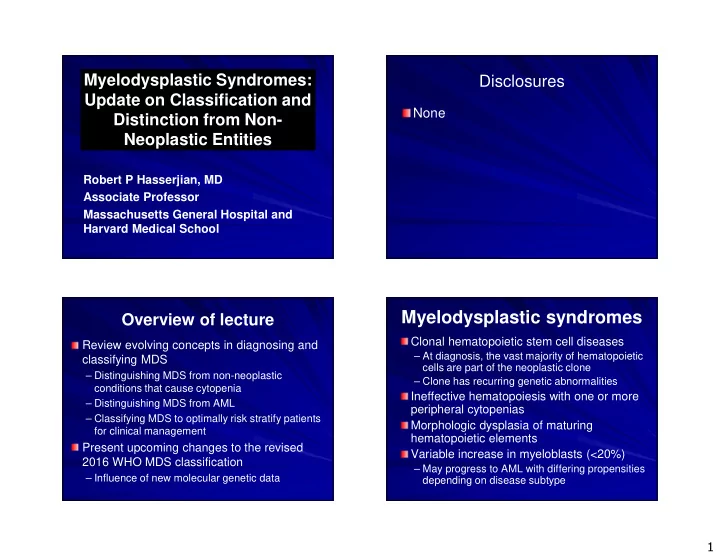
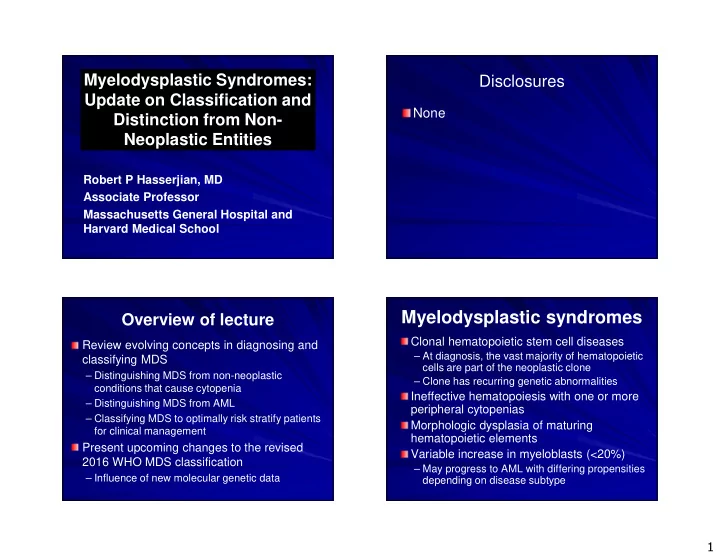
Myelodysplastic Syndromes: Disclosures Update on Classification and None Distinction from Non- Neoplastic Entities Robert P Hasserjian, MD Associate Professor Massachusetts General Hospital and Harvard Medical School Myelodysplastic syndromes Overview of lecture Clonal hematopoietic stem cell diseases Review evolving concepts in diagnosing and – At diagnosis, the vast majority of hematopoietic classifying MDS cells are part of the neoplastic clone – Distinguishing MDS from non-neoplastic – Clone has recurring genetic abnormalities conditions that cause cytopenia Ineffective hematopoiesis with one or more – Distinguishing MDS from AML peripheral cytopenias – Classifying MDS to optimally risk stratify patients Morphologic dysplasia of maturing for clinical management hematopoietic elements Present upcoming changes to the revised Variable increase in myeloblasts (<20%) 2016 WHO MDS classification – May progress to AML with differing propensities – Influence of new molecular genetic data depending on disease subtype 1
Ineffective hematopoiesis Effective hematopoiesis Indolent “ low-grade ” subtypes The spectrum of MDS Intact maturation Intact maturation MDS/MPN MDS MPN – Low blast counts – Typically low risk of progression to AML – Morbidity and mortality due to cytopenias and/or complications of � Cytopenias � Elevated counts transfusion � Dysplastic morphology � Non-dysplastic morphology � Altered cell function � Normal cell function Aggressive subtypes � No organomegaly � Often splenomegaly – Higher blast counts, genetic instability – Often rapidly progress to AML “High-grade” MDS “Low-grade” MDS Challenges in MDS diagnosis Low-grade High-grade Non-neoplastic causes of MDS AML cytopenia --Other neoplasms --Inherited --Extrinsic factors Risk-adapted therapy � according to Should the patient Does the patient have a prognosis � � receive induction or neoplasm? other intensive Should the patient be chemotherapy with a � treated for MDS or goal of remission? should another diagnosis be sought? 2
Ingredients of MDS diagnosis and Involvement of the pathologist classification (2008 WHO) in diagnosing MDS Unexplained If present, MDS-specific cytopenias are a sine cytogenetic abnormalities Patient comes to qua non of MDS provide proof of clonality clinical attention Hematologist evaluates the patient due to cytopenia --Identifiable secondary cause of Prognostic Prognostic cytopenia? --Would the patient be treated if MDS is diagnosed? Clinical information Peripheral blood and Bone marrow marrow morphology biopsy and aspirate are performed Flow cytometry Dysplasia and blasts Cytogenetics Dysplasia is a sine qua non of MDS Molecular genetics Both are prognostic Architectural disorganization in MDS Maintained architecture in reactive MDS: Low power morphologic marrow hyperplasia (AIHA) abnormalities Hypercellular marrow (80% of cases) Disorganization of hematopoiesis – Immature myeloid elements occur away from bone trabeculae – Erythroid elements fail to form well- defined clusters Often many small, hypolobated megakaryocytes 3
CD61 Megakaryocyte dysplasia ‘ Pawnball ‘ ‘ ‘ ’ ’ ’ ’ •Small size Micromegakaryocytes •Hypo/mononucleation •Separated nuclear lobes Myeloid lineage Erythroid lineage dysplasia dysplasia ‘ ‘ ‘ ‘ Pince-nez ’ ’ ’ ’ •Bilobed pseudo Pelger-Huet nucleus Normal poly •Nuclear hypersegmentation or other abnormal nuclear shape •Megaloblastoid change (nuclear:cytoplasmic asynchrony) •Cytoplasmic hypogranulation or •Cytoplasmic vacuolization uneven granulation •Bi- or multi-nucleation •Nuclear budding and nuclear irregularities, pyknosis 4
Neoplastic versus ‘ ‘ reactive ’ ‘ ‘ ’ ’ ’ Problems with using morphologic dysplasia to diagnose MDS dysplasia 10% threshold to call a lineage dysplastic No distinction between different dysplastic Normal stem cell Abnormal stem cell Normal stem cell morphologies Dysplasia is not always reproducible among pathologists Normal Abnormal microenvironment microenvironment Dysplasia is not specific for MDS – Significant dysplasia present in bone marrow of normal volunteers – Dysplastic changes are even more frequent in Normal Dysplastic progeny progeny patients with non-neoplastic cytopenias Font P Ann Hematol 2013;92:19, Parmentier S Haematologica 2012;97:723, Matsuda A Leukemia 2007;21;678, Della Porta MG Leukemia 2014;29:66 Situations to think twice before diagnosing MDS History of drugs/toxins Not MDS – Recent (<6 months) chemotherapy – Heavy alcohol intake ‘ Stress erythropoiesis ’ due to hemoglobinopathies or MDS Metabolic deficiencies: B12, folate, copper acquired/congenital hemolytic anemias Infections, especially HIV and Hepatitis C Autoimmune diseases Concurrent neoplasms – Infiltrating marrow, espcially hairy cell leukemia and myeloma – Rarely paraneoplastic dysplasia from remote solid tumor Beware of making the diagnosis in young patients! Castello A et al. Haematologica 1992;77:392 5
Can we do better than ≥ 10%? Morphologic diagnosis of MDS remains subjective 9% false positive Morphologic dysplasia Younger patients – ↑ Lineages involved Co-morbid conditions – ↑ Number of dysplastic forms Paucity of clinical history – ↑ Severity of dysplasia 5% false positive Severity and persistence of cytopenia(s)(>6 months) Unexplained ↑ MCV 11% false positive Della Porta MG Leukemia 2014;29:66 What if its not clearly MDS, but Morphologic evaluation of there’s no specific diagnosis? dysplasia in the 2016 update � A common occurrence in the workup of the Dysplasia threshold will be kept at 10% for cytopenic patient! all lineages, but will note that 30% or 40% � 60-80% of cytopenic patients undergoing BM exam level for megakaryocytes may be more � Anemia of chronic inflammation – Often increased iron in marrow histiocytes specific � Reactive causes which may or may not become – Emphasis on micromegakaryocytes as a evident later highly specific morphologic finding for MDS – Test of time: transient causes often resolve Emphasis on morphologic overlap with � Early MDS cases which are not well-developed non-MDS mimics (always a potential enough for definitive diagnosis – Test of time: cytopenia is refractory or worsens pitfall!) – OK to hedge on initial marrow in these situations Hasserjian RP Arch Pathol Lab Med 2008;132:587 Matsuda A Leukemia 2007;21;678, Della Porta MG Leukemia 2014;29:66 6
Idiopathic cytopenia of Can we develop a more objective way to diagnose MDS? undetermined significance � ICUS designation proposed for patients Genetic abnormalities with prolonged, unexplained cytopenia(s) – Karyotype abnormalities who do not fulfill MDS diagnostic criteria – Sub-karyotypic acquired genetic – Insufficient dysplasia and normal karyotype alterations � These patients should be followed Microdeletions (SNP array) – Some will eventually be diagnosed with MDS Mutations (next-generation sequencing) – In others, another cause for cytopenia will Flow cytometry abnormalities emerge – Hematopoiesis in most MDS cases is – Some remain with persistent, stable cytopenia and no identifiable cause phenotypically abnormal Wimazal F Leuk Res 2007; 31:727, Valent P Leuk Res 2012;36:1 Utility of MDS flow cytometry MDS-defining cytogenetic assessment abnormalities (WHO) � Accumulating evidence 84.8% CD34 PerCP-Cy5-5-A 10 5 Unbalanced Primary MDS Therapy-related MDS 5 suggests that abnormal 10 10 4 -A -7 or del(7q) 10% 50% 4 C 10 P flow cytometry patterns 13 A MDS -5 or del(5q) 10% 40% 10 3 3 10 CD i(17q) or t(17p) 3-5% predict MDS with good 10 2 2 10 -13 or del(13q) 3% -10 2 2 -10 del(11q) 3% 10 3 10 4 10 5 sensitivity/specificity -10 2 2 3 4 5 -10 10 10 10 CD7 FITC-A CD16 FITC-A del(12p) or t(12p) 3% del(9q) 1-2% � Only considered as idic(X)(q13) 1-2% CD34 PerCP-Cy5-5-A 10 5 10 5 5.39% “supportive” of MDS, PC-A Normal 10 4 10 4 Balanced CD13 A not sufficient for making 10 3 10 3 t(11;16)(q23;p13.3) 3% 10 2 t(3;21)(q26.2;q22.1) 2% 10 2 a primary MDS -10 2 -10 2 t(1;3)(p36.3;q21.2) 1% 10 3 10 4 10 5 -10 2 -10 2 10 3 10 4 10 5 t(2;11)(p21;q23) 1% diagnosis by WHO CD7 FITC-A CD16 FIT C-A inv(3)(q21q26.2) 1% Cytogenetic abnormality in Courtesy of Dr S Wang, MD Anderson Cancer Center 2008/2016 t(6;9)(p23;q34) 1% 50% of MDS cases Tang G Leuk Res . 2012;36:974-81, Kern W Haematologica 2013;98:201-7, Malcovati L Blood 2013;122:2943-64 7
Recommend
More recommend