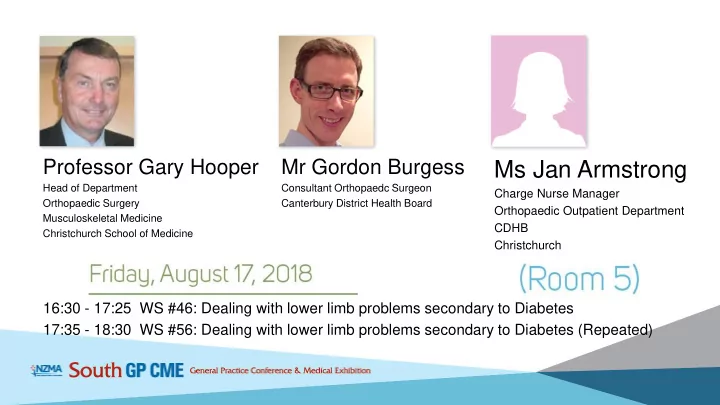
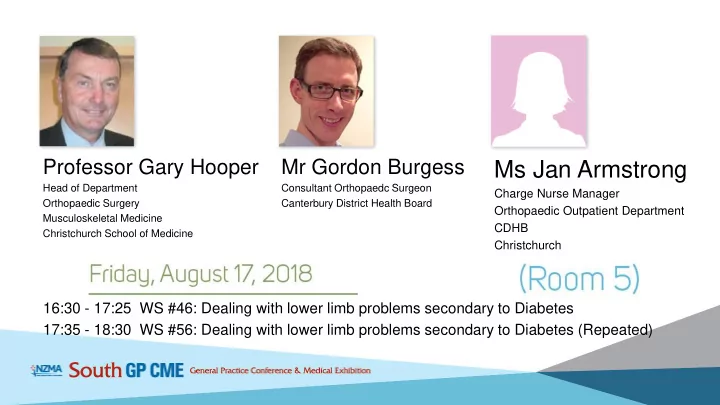
Professor Gary Hooper Mr Gordon Burgess Ms Jan Armstrong Head of Department Consultant Orthopaedc Surgeon Charge Nurse Manager Orthopaedic Surgery Canterbury District Health Board Orthopaedic Outpatient Department Musculoskeletal Medicine CDHB Christchurch School of Medicine Christchurch 16:30 - 17:25 WS #46: Dealing with lower limb problems secondary to Diabetes 17:35 - 18:30 WS #56: Dealing with lower limb problems secondary to Diabetes (Repeated)
Application of a Charcot Cast Jan Armstrong RGON, BA (Cant) Charge Nurse Manager Orthopaedic Outpatient Department CHRISTCHURCH HOSPITAL
A Case study J is a 38 year old who has had diabetes for 13 years. She has been known to our Service since 2014 She has had had 2 formal surgeries for her foot during this time, and some further admissions for infection flare ups over this period She has to wear steel-cap boots in her job, which involves standing a lot, she has had considerable time off work as we have tried casting her foot over these years to offload her ulcerated foot area to gain sufficient healing - to allow her to go back to work in custom-made boots. She is reluctant to have further surgery, as can’t afford more time off work.
J’s foot appearance prior to debridement by the Diabetic Podiatrist, just after it has come out of her cast. Patients wash their foot in a disposable basin between cast changes. They are provided with shower stools and plastic bags as necessary, to keep their cast dry
J’s foot with an absorbent dressing applied after debridement, which stays on for one week under the cast. A variety of dressings are used, including silver – depending on the condition of the wound, and the amount of exudate.
Note the high instep in J’s foot, which causes ongoing pressure issues when she is out of cast
Due to insensate feet often being present in Diabetics, we always enclose the whole foot in the cast, with padding between the toes. We have found with the whole foot in the cast wounds also seem to heal more quickly.
We need to offload the foot deformities and create a flat surface for the patient to weight-bear in their cast
We always use cotton liner and padding under these casts
The toes are always well protected with padding and foam so they do not develop pressure areas under the cast
Limbs become quite wasted with prolonged casting so we always protect all bony areas with felt over the top of the cast padding
Additional foam is placed around the top of the cast for comfort
A layer of semi-rigid synthetic (Softcast) is applied first under the hard synthetic layers, to avoid any swelling issues, and the likelihood of the cast being applied too tightly around the toe area.
Strips of Synthetic F/Glass are then applied during casting to reinforce the foot area which takes the greatest impact whilst the patient is walking on their cast
Patients have a large choice of plain or pattern synthetic casting product to choose from.
The assistant who is holding the patient’s foot in a neutral 90 degree position, is of equal importance to that of nurse applying the Charcot cast. The foot holding can be a challenge if the patient has a significant foot or ankle deformity, but being able to mobilise safely in comfort is crucial for all our patients.
A shoe is fitted, and J then waits for 20 minutes for the cast to set sufficiently for her to walk out of the Department. J will return weekly for changes of cast, until her wound has healed sufficiently to progress to some form of footwear.
For patients who do not have wounds, but are being treated in Charcot casts for Charcot arthropathy, come to the department every 2 or 3 weeks for changes of cast. A cast can take 30 – 45 minutes to apply depending on the complexity - whether patients have a wound or very deformed foot. The Diabetic Podiatrists attend all our clinics and debride any wounds and trim a patient’s nails before casts are re-applied We also have regular input from our Orthotic Service who take moulds of the patient’s foot to provide custom-made insoles to go into the patient shoe or Moonboot, which they wear once the casting period is complete. It is vital to have a multi-disciplinary approach to these complex patients, and skilled staff who are able to competently apply casts which do not cause pressure areas, and allow patients to remain mobile in their homes. Most importantly expert medical input from our Orthopaedic Surgeons with an understanding of the Charcot condition and the foot and ankle challenges is vital.
Staff get to know these patients well over their journey, and help provide support and encouragement, and always check with the patients if they had any issues with their previous cast! There is often a social and financial impact for these patients. Their condition is not ACC-related, and if the cast is applied on their right foot they are unable to drive, which can be socially isolating, and they may even lose their employment. Patients can potentially become quite depressed with their ongoing cast treatment over the months. We encourage the patients to speak to others attending the weekly clinics who are also on a similar journey. We are fortunate to have an 8 bedded Plaster Room, and so patients have an opportunity to engage with each other if they wish. Our greatest sense of achievement is when the patients whom we’ve casted for many weeks or months are successfully healed, and do not need to return for future input from our service.
Recommend
More recommend