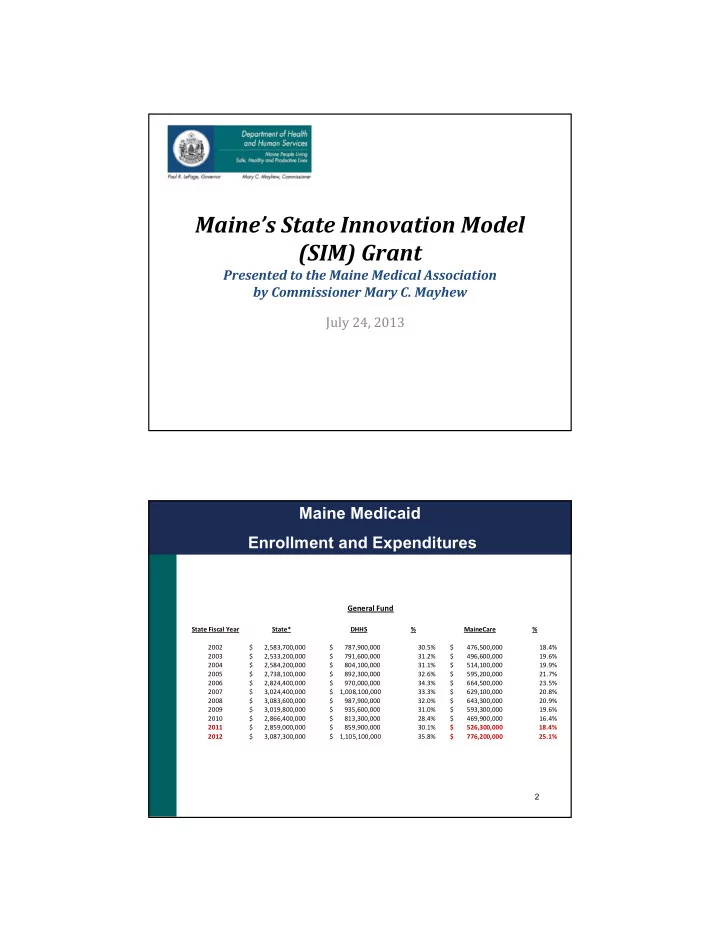
Maine’s State Innovation Model (SIM) Grant Presented to the Maine Medical Association by Commissioner Mary C. Mayhew July 24, 2013 Maine Medicaid Enrollment and Expenditures General Fund State Fiscal Year State* DHHS % MaineCare % 2002 $ 2,583,700,000 $ 787,900,000 30.5% $ 476,500,000 18.4% 2003 $ 2,533,200,000 $ 791,600,000 31.2% $ 496,600,000 19.6% 2004 $ 2,584,200,000 $ 804,100,000 31.1% $ 514,100,000 19.9% 2005 $ 2,738,100,000 $ 892,300,000 32.6% $ 595,200,000 21.7% 2006 $ 2,824,400,000 $ 970,000,000 34.3% $ 664,500,000 23.5% 2007 $ 3,024,400,000 $ 1,008,100,000 33.3% $ 629,100,000 20.8% 2008 $ 3,083,600,000 $ 987,900,000 32.0% $ 643,300,000 20.9% 2009 $ 3,019,800,000 $ 935,600,000 31.0% $ 593,300,000 19.6% 2010 $ 2,866,400,000 $ 813,300,000 28.4% $ 469,900,000 16.4% 2011 $ 2,859,000,000 $ 859,900,000 30.1% $ 526,300,000 18.4% 2012 $ 3,087,300,000 $ 1,105,100,000 35.8% $ 776,200,000 25.1% 2
What is the Purpose of The SIM Grant? “… to test whether new payment and service delivery models will produce superior results when implemented in the context of a state-sponsored State Health Care Innovation Plan. These plans must improve health, improve health care, and lower costs for a state’s citizens through a sustainable model of multi-payer payment and delivery reform, and must be dedicated to delivering the right care at the right time in the right setting.” 4
SIM: A High-Level View This grant will ultimately position Maine to assess the full impact associated with existing healthcare delivery test reform models by moving the test models to the next level through: • Enhanced care delivery capabilities • Greater access to high-value care information and data • Enhanced care delivery “actor” (provider and patient) training / support • Introduction of targeted incentives 5 Aligning SIM Strategies With the Triple Aim Goals of the “Triple Aim”: • Improving the individual experience of care; • Improving the health of populations; • Reducing the per capita costs of care for populations. 6
Building Off Current Initiatives The existing healthcare delivery test reform models include MaineCare’s: • Patient-Centered Medical Homes • Emergency Department initiative • Health Homes • Accountable Communities 7 Maine PCMH Pilot Community Care Teams Environment Transportation Housing Outpatient Workplace Care Mgt Services Family Food Systems High-need Med Mgt Specialists Individual Shopping Coaching Hospital Services Behav. Health & Sub Income Abuse Physical Therapy Heat Literac y Faith 8 Community
The Emergency Department Initiative • Identifying high-cost utilizers of hospital Emergency Departments and intensifying the efforts to manage their care • Providing services in the most appropriate, cost-effective manner • Establishing solid relationships with primary care providers and improving patient outcomes • Understanding the importance of social and non-medical barriers • Total savings of $4.15 million in SFY ‘12 and $4.2 million in SFY ’13 • 1,700 patients currently participating in the program 9 Maine Health Homes A Key to Sustainability Stage A (ongoing): • Health Home = Medical Home primary care practice + CCT • Currently have 150 enrolled practices and 10 CCTs • Payment weighted toward medical home • Eligible Members: • Two or more chronic conditions • One chronic condition and at risk for another Stage B (Fall Implementation): • Health Homes = CCT with behavioral health expertise + primary care practice • Payment weighted toward CCT • Eligible Members: • Adults with Serious Mental Illness • Children with Serious Emotional Disturbance 10
Maine’s Accountable Communities: The Basic Components • Providers will work together and propose an alternative contract to share in any savings achieved • The amount of shared savings will depend on achieving quality benchmarks • Open to any willing and qualified providers statewide (through application process) • Accountable Communities are not limited by geographical area • Members retain choice of providers • Alignment with aspects of other emerging ACOs is desired • Flexible design encourages innovation 11 Benefits for Providers Patient Accountability • Resources for shared decision-making • Assistance with patient incentives, benefit design Data Analytics • EHR for behavioral health organizations • Connection to Health Information Exchange • Resources for other data analytic needs Transformation Support • Leadership training • Practice transformation learning collaborative • ACO learning collaborative Payment Reform • Greater consistency and alignment across payers/ initiatives • Potential for performance-based shared savings payments 12
Outcome-Based Reimbursement Models • apitated populations • hared savings • Benefits For Patients Ability to Compare Based on Quality and Cost Data Coordinated Care Doctors and medical staff coordinate with other medical providers to make sure everyone is ‘on the same page’ Chronic Care Management Access to care managers to make connections to non-medical resources Tools for better self-management Community health navigators Specialized Support Adults and children with developmental disabilities will be linked to doctors and caregivers who have been trained to meet their needs Physical and Mental Health Integration 13 The Future State Of HealthCare Delivery System Change and Positive Outcomes Regardless of Payor Source High Quality, Affordable Care Supported by: • Public Reporting • Pay for Quality • Total Cost of Care Benchmarks Engaged Patients Supported through: • Review of Performance Measures • Shared decision-making • Access to personal health data/information 14 lobal payments
The Future State Of HealthCare Delivery Data-Informed Care • Access to ‘real time’ clinical data • Timely claims data • Public health data Improved Population Health Management through: • Patient-Centered Medical Homes • Health Homes • Accountable Care 15 Keys to Our Success • Ability to run and provide transparent, accurate and reliable member attribution, cost and quality metrics • Provider partnership with DHHS in initiatives • Outreach to potential providers in most rural areas • Community-based approaches that go beyond a medical model to encompass behavioral health and social supports • Facilitation of provider use of Electronic Health Records, Health Information Exchange and other secure data sharing methods 16
For More Information Mary. C. Mayhew, Commissioner Maine Department of Health and Human Services Mary.C.Mayhew@maine.gov (207) 287-4223 17
Recommend
More recommend