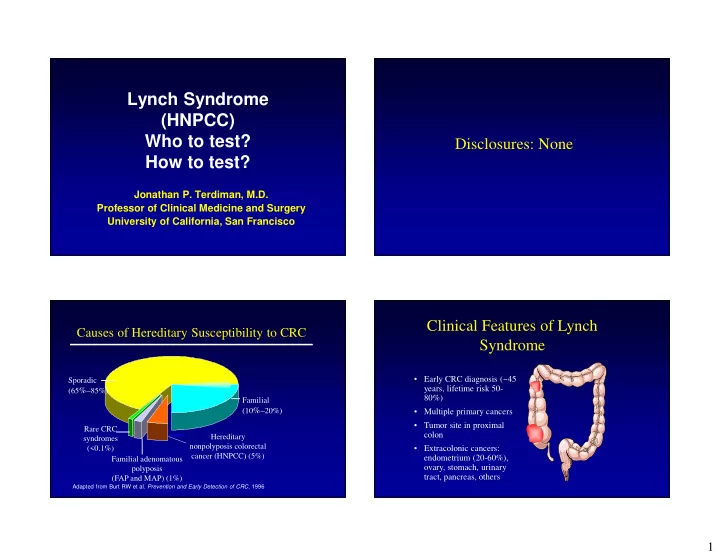
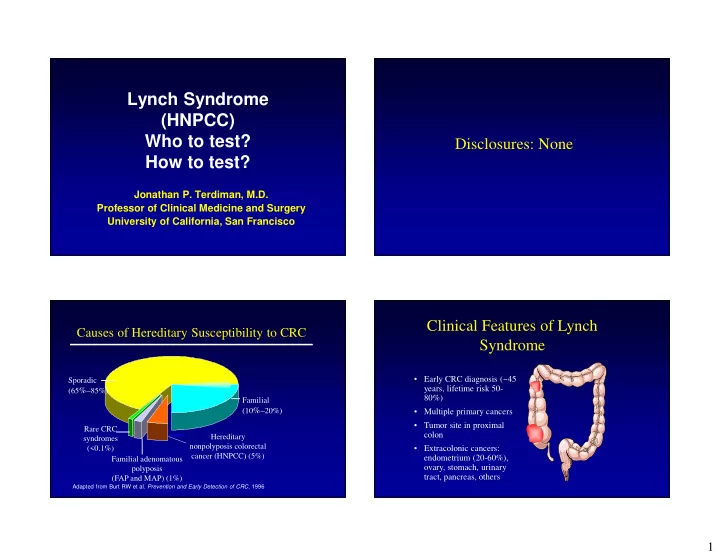
Lynch Syndrome (HNPCC) Who to test? Disclosures: None How to test? Jonathan P. Terdiman, M.D. Professor of Clinical Medicine and Surgery University of California, San Francisco Clinical Features of Lynch Causes of Hereditary Susceptibility to CRC Syndrome • Early CRC diagnosis (~45 Sporadic years, lifetime risk 50- (65 %– 85%) 80%) Familial (10 %– 20%) • Multiple primary cancers • Tumor site in proximal Rare CRC colon Hereditary syndromes nonpolyposis colorectal (<0.1%) • Extracolonic cancers: cancer (HNPCC) (5%) endometrium (20-60%), Familial adenomatous ovary, stomach, urinary polyposis tract, pancreas, others (FAP and MAP) (1%) Adapted from Burt RW et al. Prevention and Early Detection of CRC , 1996 1
Cumulative Proportion Free of CRC Lynch – Screening Recommendations Kidney / Ureteral cancer MRI Urogram +/- urine cytology (?) Stomach cancer EGD (Optional) Annual TVUS, CA-125 Ovarian cancer Annual TVUS / endometrial aspiration Endometrial cancer Colonoscopy every 1-2 years Colorectal cancer Annual H&P, ROS, education, counseling Birth 10 years 20 years 30 years 50 years Jarvinen HJ et al. , Gastro 2000; 118:829 Jama 2007;296:1507-17 Cumulative Incidence: Endometrial CA Aspirin Chemoprevention Burn J, et al. Lancet 2011;378:2081-87 Schmeler KM et al. , NEJM 2006; 354:261 2
Cumulative Incidence: Ovarian CA Lynch syndrome results from failure of mismatch repair (MMR) gene function T C G A C Normal Base pair DNA repair mismatch A G C T G T C T A C A G C T G T C T A C T C T A C Defective DNA repair (MMR+) A G A T G A G C T G = MSI-H Schmeler KM et al. , NEJM 2006; 354:261 MSI Testing Immunohistochemistry • Identify MMR proteins • Normally present • If protein is absent, gene is not being expressed (mutation or methylation) MLH1 MSH2 • Helps direct gene testing by predicting likely involved gene • If abnormal IHC (absent), MSI+ PMS2 MSH6 3
Contribution of Gene Mutations So, Who to Test and How? to Lynch Families MSH2 • First select by clinical criteria, or test all ~35% Unknown CRC patients? ~20% • Tumor MSI or IHC or combination? • When to do germline genetic test? • What if clinical suspicion high but lab MSH6 ~ 10% tests normal? MLH1 PMS2 (< ~35% 5%) Amsterdam II criteria Bethesda Guidelines • Individual with CRC dx <50 • 3 or more relatives with verified HNPCC- • Individual with synchronous or metachronous CRC, associated cancer in family or other HNPCC-associated tumors regardless of age • Two or more generations • Individual with CRC with MSI-H histology dx <60 • Individual with CRC with >1 FDR with an HNPCC- • One case a first-degree relative of the associated tumor, with one cancer dx <50 other two • Individual with CRC with >2 FDRs or SDRs with an • One CRC dx <50 HNPCC-associated tumor, regardless of age • FAP excluded Vasen HFA et al. Gastroenterology. 116:1453, 1999 Umar A, et al. JNCI. 2004;96(4):261-268. 4
Warning: Family Histories can be Diagnostic Models for Lynch Deceiving • Family size is getting smaller • Wider use of colonoscopy likely to prevent many colon cancers • MSH6/PMS2 may have lower cancer risks • Population-based case ascertainment may be associated with lower cancer risks JAMA Sept 2006 Columbus-Area Lynch Study The Columbus Area Lynch Study Flow MSI unselected newly diagnosed patients Colorectal cancer Columbus OH Total accrued N = 1600 Testing completed N = 1566 No further MSI stable MSI-H and L action MSI negative MSI positive (high & low) IHC 4 proteins N =1259 (80.4%) Methylation MLH1 N = 307 (19.6%) promoter/BRAF Sequence MLH1, MSH2, MSH6 Mutation analysis of Immunohistochemistry selected patients for Mutation analysis by Methylation of MLH1 promoter PMS2 based on IHC sequencing MLH1, MSH2, MSH6 and deletion analysis by MLPA Mutation positive Mutation negative or Mutation result not yet polymorphism found N = 44* 2.7% (1/35) interpretable N =209 13.4% Germline mutations N =55 3.5% Hampel et al. NEJM 2005;352:1851-60.; Unpublished 5
Recommended Approach in 2013 Summary of Findings MLH1 & PMS2 MSH2& MSH6, All Present 80% Absent or • 1 out of 35 colon cancer patients has Lynch 15% MSH6 or PMS2 syndrome Absent - 5% • 50% of CRC patients with LS are diagnosed CRC dx <45; OR CRC dx <60; CRC dx >60 CRC dx >45 & No & No OR over age 50 FDR with CRC; suggestive personal or OR Family or history, family • 24% of CRC patient with LS do not meet personal history Multiple primaries BRAF + history of Lynch cancer any family history criteria BRAF (-) • IHC easier logistically, cheaper, predicts the mutated MMR gene when screening cancer Refer to Clinical Refer to Clinical Stop Stop patients Cancer Genetics Cancer Genetics Conclusions • Important to identify Lynch Syndrome – Different outcomes for probands and relatives with more intensive surveillance – Lynch = hereditary defective mismatch repair • Best method for detection? – UNIVERSAL TUMOR TESTING OF CRC CASES AND ENDOMETRIAL CANCER TOO – GERMLINE TESTING FOR THOSE WITH POSITIVE TUMORS – GERMLINE TESTING OF NON AFFECTED RELATIVES ONCE MUTATION FOUND IN PROBAND – COMPREHENSIVE CANCER FAMILY HISTORY STILL IMPORTANT TO DETECT LYNCH IN NON CRC CANCER PATIENTS AND NON LYNCH CANCER FAMILIES Ladabaum et al , Ann Intern Med 2011;155:69 6
UCSF - 2013 • Universal Testing • Testing Protocol – MSI and 4 protein IHC – If MLH1 is absent, we do BRAF testing • Reflex genetics referral for “positives” based on this screening procedure • 278 colon cancers tested – 45/278 (16%) with abnormal results – 13/45 with BRAF mutations found- so no Lynch – 13/45 refused further genetic work-up – 19/45 underwent genetic counseling and testing for Lynch • Mutations: MSH2 in 7, MLH1 in 5, MSH6 in 1, no mutation found in 3 and pending in 3 • So 12 (4%) of entire population with confirmed Lynch 7
Recommend
More recommend