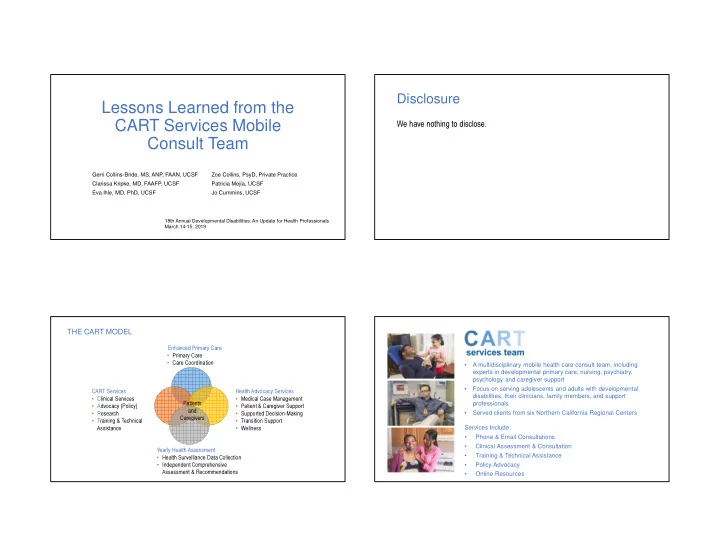
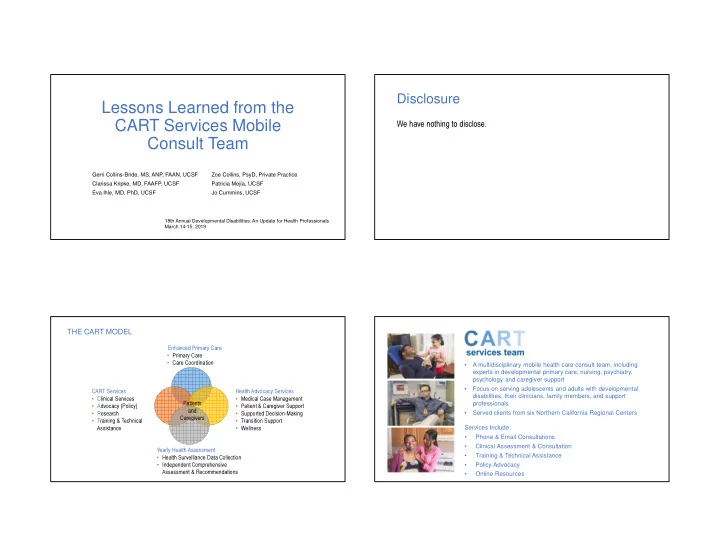
Disclosure Lessons Learned from the CART Services Mobile We have nothing to disclose. Consult Team Gerri Collins-Bride, MS, ANP, FAAN, UCSF Zoe Collins, PsyD, Private Practice Clarissa Kripke, MD, FAAFP, UCSF Patricia Mejía, UCSF Eva Ihle, MD, PhD, UCSF Jo Cummins, UCSF 18th Annual Developmental Disabilities: An Update for Health Professionals March 14-15, 2019 THE CART MODEL Enhanced Primary Care • Primary Care • Care Coordination • A multidisciplinary mobile health care consult team, including experts in developmental primary care, nursing, psychiatry, psychology and caregiver support • Focus on serving adolescents and adults with developmental CART Services Health Advocacy Services disabilities, their clinicians, family members, and support • Clinical Services • Medical Case Management professionals • Advocacy (Policy) Patients • Patient & Caregiver Support • Research and • Supported Decision-Making • Served clients from six Northern California Regional Centers Caregivers • Training & Technical • Transition Support Services Include: • Wellness Assistance • Phone & Email Consultations • Clinical Assessment & Consultation Yearly Health Assessment • Training & Technical Assistance • Health Surveillance Data Collection • Independent Comprehensive • Policy Advocacy • Online Resources Assessment & Recommendations
SERVICES BY COUNTY COMPREHENSIVE CONSULTS BY PRIMARY TOPIC Review of Recent Hospitalizations: 5% Comprehensive Consult Diagnosis: 11% Focused Consult Training/Resource Decline in Function Dissemination or Status: 34% Placement: 11% Medical Review of Recurring Symptoms: 17% Behavior: 22% COMPREHENSIVE CONSULTS: BY HOURS TRAINING TOPICS • Care of People with Developmental Disabilities ACTIVITY AVG. HOURS • Health Advocacy: Ensuring Quality Health Outcomes for People with Developmental Overall Average Consult Time 56 Disabilities • Pre-Consult Prep Work: including record review 12 Respectful End of Life & Goals of Care Conversations: Ethical Principles and Practical Tips In-person Consult 4 • Sensory Processing Differences: How to Recognize, Accommodate and Appreciate Travel 10 Them • Supported Health Care Decision-Making Report Writing 21 • Understanding Aggression and Self-Injury in Autism and Other Developmental Post-Consult Follow Up 2.5 Disabilities
WEBSITE BRAIN-BASED CHANGES IN BEHAVIOR https://odpc.ucsf.edu/ BEHAVIORAL OUTBURSTS DECLINE IN FUNCTION • Advice from Self-advocates Defined as withdrawal, PMR, poor appetite Defined as increased aggression, agitation • Best practice recommendations DDX DDX • Clinical chart forms • Physiologic issue (illness) • Physiologic issue (pain, seizure) • Depression • Trauma and stressor-related disorder • Navigating systems • Catatonia (inhibited) • Catatonia (excited) • Tracking tools TRAUMA TRAUMA • Individuals with Intellectual or Developmental Disabilities (IDD) experience • Trauma-informed care, which includes steps aimed at improving a sense of abuse, neglect, institutionalization, restraint and seclusion, abandonment, safety (emotional/physical), and trustworthiness (maintaining appropriate bullying and other forms of maltreatment at higher rates than the general boundaries and making tasks clear), were often missing from treatment population. plans/framework aimed at reducing behaviors. • “Trauma-informed care” refers to the ability of care providers to recognize the • Reframing the behaviors in the context of the whole person and taking into impact of past trauma on behavior, and appreciate the significance of trauma account trauma histories improves outcomes and reduces maladaptive histories for the populations they serve. behaviors. • Failure to recognize the role of trauma in the challenging behavior exhibited by some people with IDD, and incorporate trauma-informed practices into their treatment, can exacerbate past trauma or cause new trauma, compromising the ability to meet their potential.
CAREGIVER ASSESSMENTS - BACKGROUND CAREGIVER ASSESSMENTS - FINDINGS • Developed Assessment Tool • Average age of client: 37 - Overview of Concerns • Average age of caregiver: 60+ - Priorities • Primary Concerns: - Personal Needs - Transfer of Caregiving Responsibilities: who will replace me, population aging, - Review of Existing Supports & Services best interests of caregivers and clients not necessarily aligned • Report with Recommendations - Lack of Services: case management across systems, housing options, nursing • Caregiver had to request/consent to assessment care, respite, stable support service staff, caregiver resuming care • Assessment conducted in-person - Health of Caregiver: physical and emotional health • Assessment conducted in private – away from client and consultation team - Financial Concerns: inability to work outside of the home due to caregiving responsibilities; reliance on IHSS and other sources of income • Caregiver-to-caregiver dynamic LESSONS LEARNED • There are no shortcuts to seeing patients in their environment or team-based care • reason for the consult was different than what we found • can’t rely on other people’s observations Office of Developmental Primary Care • observing whole team and environment matters a lot 500 Parnassus Avenue, Box 0900 • Attitudes are a major health care access issue Tel: 415-476-4641 | Fax: 415-476-6051 email: odpc@fcm.ucsf.edu • Medical education is primarily an apprenticeship model—seeing patients with providers and discussing web: http://odpc.ucsf.edu their complex cases with them. • Family, Direct Support Professionals, and Service Providers are front line health professionals who need training, support, and oversight. It isn’t enough to focus exclusively on the needs of people living in higher level group homes because that isn’t where most people live. • Key challenges: access to skilled nursing outside of group homes, mental health services with expertise in DD, interagency collaboration
Recommend
More recommend