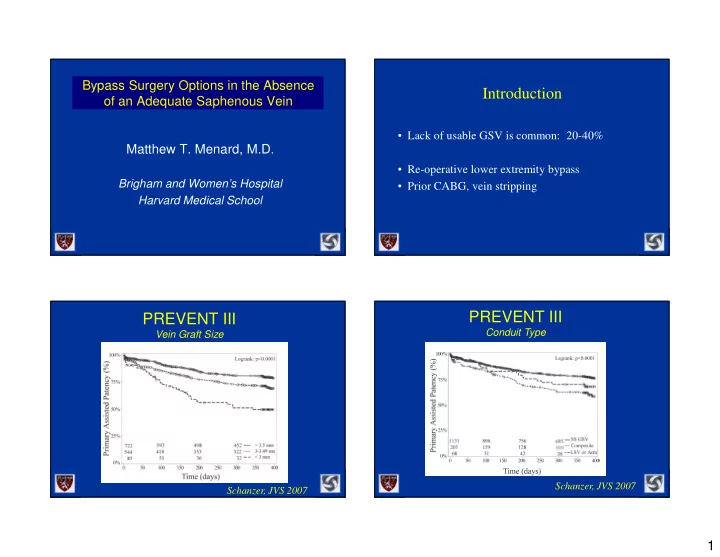
Bypass Surgery Options in the Absence Introduction of an Adequate Saphenous Vein • Lack of usable GSV is common: 20-40% Matthew T. Menard, M.D . • Re-operative lower extremity bypass Brigham and Women’s Hospital • Prior CABG, vein stripping Harvard Medical School PREVENT III PREVENT III Conduit Type Vein Graft Size Schanzer, JVS 2007 Schanzer, JVS 2007 1
PREVENT III General Strategies High vs Low Risk Conduit • Perform the best, most durable procedure possible. • Use the best available autogenous vein. Schanzer, JVS 2007 Options Re-operative Survey: Challenges • Contralateral Greater Saphenous Vein • Arm Vein • Vascular bad actors: Intimal hyperplasia, • Lesser Saphenous Vein sclerotic veins, hypercoagulable states, etc • Scarring • Cryopreserved vein • More advanced disease. • Prosthetic grafts • Endovascular/hybrid 2
CLV Harvest and Fate of the Contralateral GSV Contralateral Limb • Only 16% needed intervention in contra leg • 12% bypass • 4% amputation JVS 2002 3
Infrainguinal Bypass in the Absence of GSV: Arm Vein Lesser Saphenous Vein Disadvantages: Advantages: • Same operative field. • Can be tenuous quality • Can be qualitatively similar to GSV. » Antecubital scarring » Focal phlebitis, sclerosis Disadvantages: » Short vein segments. • Tedious exposure. • Unreliable quality. • Tedious harvest of basilic/brachial vein • Short vein segments. • Prone to twisting Composite Vein Grafts: Demographics (Chew 1998) • 154 patients • Limb salvage in 90% • Redo: 48% 4
Number of Segments Patency of Composite Grafts 110 100 90 LS 79% + 5% % Cumulative Patency 80 SP 65% + 5% 70 3 Seg 60 50 PP 44% + 5% 23% 2 Seg 40 75% 30 20 10 4 Seg 0 0 10 20 30 40 50 60 70 2% Time (months) Composite Vein Grafts Chew, JVS, 2001 5
Patency Rates Prosthetic Grafts 90 Cumulative Patency (%) 80 70 Primary Patency Rate 60 50 Primary Assisted Patency Rate 40 30 Secondary Patency Rate 20 10 0 1 4 7 10 13 16 19 22 Months P=ns, Log-rank test Summary of meta-analysis data since 1981 Distaflo Grafts carbon lined engineered cuffs 6
Distaflo Grafts 7
Propaten: Thromboresistant lumenal graft surface Linton patch Heparin Bonded PTFE • Italian, 7 center, retrospective review • 425 bypass for CLI (101 AK, 324 BK) • 36 month results: PP 61%, SP 70% • No diff AK vs BK Pulli et al, JVS, 2010;51:1167 8
Miller cuff St. Mary’s boot Tyrell MR, Wolfe JHN; Br J Surg 1991 Tyrell MR, Wolfe JHN; Br J Surg 1991 9
Tyrell MR, Wolfe JHN; Br J Surg 1991 Tyrell MR, Wolfe JHN; Br J Surg 1991 Tyrell MR, Wolfe JHN; Br J Surg 1991 Tyrell MR, Wolfe JHN; Br J Surg 1991 10
Dardik H, et al J Vasc Surg 1996 Taylor patch Secondary Patency Alternative Vein Prosthetic 100 90 80 70 % Patency 68.8% 60 68.4% 50 P=0.488 40 30 20 Number at risk 10 33 25 21 AV 17 12 10 0 52 34 25 Pros 14 9 8 0 12 24 36 48 60 Months 11
Summary • Do the best operation/procedure you can • Use the best vein available. • Prosthetic is reasonable option, and is better than bad vein • Need for appropriate creativity in hybrid era 12
Recommend
More recommend