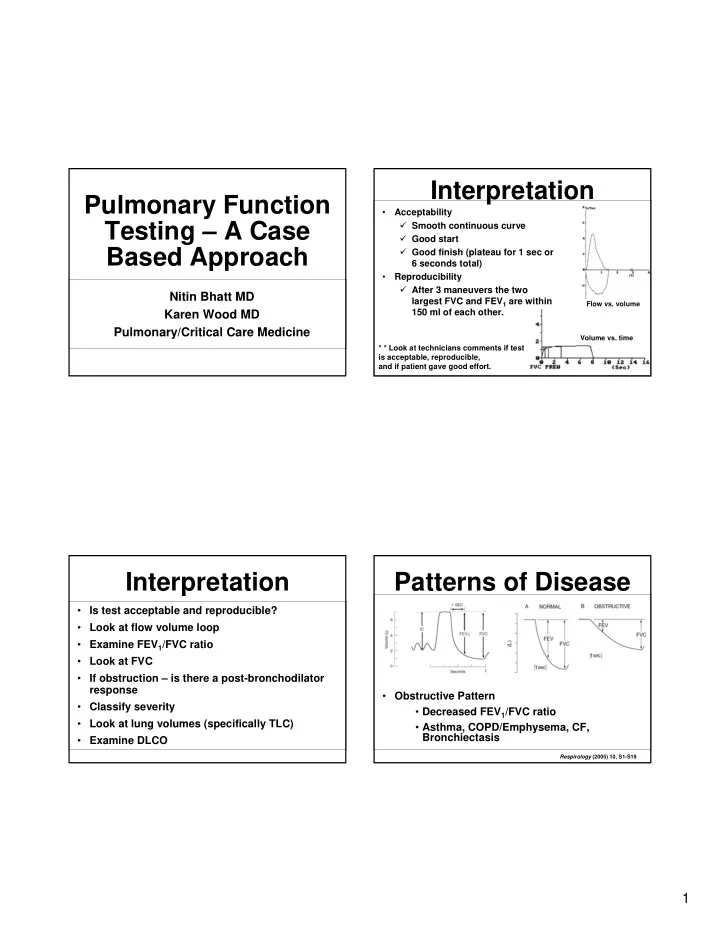
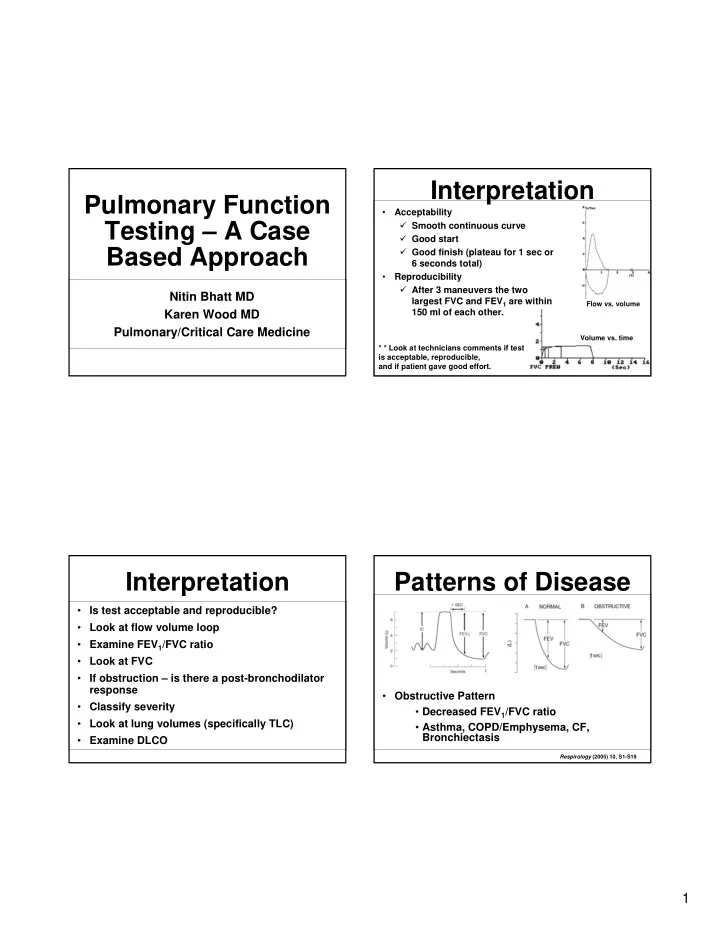
Interpretation Pulmonary Function • Acceptability Testing – A Case � Smooth continuous curve � Good start Based Approach � Good finish (plateau for 1 sec or 6 seconds total) • Reproducibility � After 3 maneuvers the two Nitin Bhatt MD largest FVC and FEV 1 are within Flow vs. volume Karen Wood MD 150 ml of each other. Pulmonary/Critical Care Medicine Volume vs. time * * Look at technicians comments if test is acceptable, reproducible, and if patient gave good effort. Interpretation Patterns of Disease • Is test acceptable and reproducible? • Look at flow volume loop • Examine FEV 1 /FVC ratio • Look at FVC • If obstruction – is there a post-bronchodilator response • Obstructive Pattern • Classify severity • Decreased FEV 1 /FVC ratio • Look at lung volumes (specifically TLC) • Asthma, COPD/Emphysema, CF, Bronchiectasis • Examine DLCO Respirology (2005) 10, S1-S19 1
Patterns of Disease Bronchodilator Challenge • Restrictive Pattern • Assess lung function at baseline � FEV 1 /FVC ratio preserved but values decreased • Administer bronchodilator through a spacer � Parenchymal disease • Re-assess lung function after 15 min • Idiopathic pulmonary fibrosis (IPF), • Positive bronchodilator response • Pneumoconiosis • Interstitial lung diseases • An increase in FEV1 and/or FVC by 12% of � Restrictive bellows control and by > 200 mL • Neuromuscular disease (ALS, MD) • In the lack of a bronchodilator response in the • Chest wall laboratory does not preclude a clinical response abnormalities to bronchodilator therapy (obesity, kyphoscoliosis) Respirology (2005) 10, S1-S19 Examine FEV 1 /FVC ratio Flow Volume Loop <70% >70% or or Obstruction Examine FVC LLN LLN nl Examine FVC nl Possible restriction – Normal test perform lung volumes Post Possible mixed bronchodilator disease – may need FEV 1 and FVC nl TLC lung volumes nl Restriction COPD Asthma Early glottic closure Variable effort Cough DLCO DLCO nl nl Extra- Parenchymal Chronic pulmonary emphysema bronchitis Pulmonary Vascular 2
Case 1 • Obstruction with bronchodilator response • Started on inhaled corticosteroid, as needed • 31 y/o female with 3 ½ month history of cough B2 agonist, and given peak flow meter. usually non-productive. Associated wheezing and • Return in 3 weeks revealed cough has almost mild dyspnea. Started after a viral illness. totally resolved, peak flow has increased from • No PMH, ROS negative. 460 to 600. • Lungs – scattered bilateral expiratory wheezes. • Dx – asthma • CXR - negative Case 2 59 yr old male 59 yr old male 3
hyperinflation hyperinflation hyperinflation Air trapping Air trapping Air trapping • Severe airflow obstruction with air trapping and hyperinflation. • Low DLCO • Dx - COPD Respirology (2005) 10, S1-S19 Case 3 Interpretative strategies for lung function tests. SERIES ‘‘ATS/ERS TASK FORCE: STANDARDISATION OF LUNGFUNCTION TESTING’’ Eur Respir J 2005 4
What’s normal? • Reference Populations • Comparable to the patient population with regards to: » Age •Reduced FEV1 and FVC •Reduced FEV1 and FVC suggest restriction by suggest restriction by » Height spirometry spirometry » Gender •No evidence of restriction by •No evidence of restriction by » Ethnicity lung volumes. lung volumes. • Spirometric reference values •Low FVC – pseudorestriction •Low FVC – pseudorestriction • Developed from National Health and Nutrition •If use SVC then the •If use SVC then the Examination Survey FEV1/VC ratio is 48%. FEV1/VC ratio is 48%. (NHANES III) Dx - Severe oxygen-dependent Dx - Severe oxygen-dependent • 7,429 asymptomatic, lifelong nonsmoking subjects chronic obstructive pulmonary disease chronic obstructive pulmonary disease • Included Caucasians, African-Americans, and Hispanic- Americans Case 4 Predicted 90 LLN 80 FEV1/FVC FN 70 FP 60 50 20 30 40 50 60 70 80 90 age • FEV1/FVC is inversely proportional to age and height. 5
Case 5 Case 5 • • 58 yoAAM smoker with cough • 40PY tobhistory • Lung age = 97 yo • Yearly history and • physical exam –c/o mild dyspnea Lung Age Case 6 • 54 yo WM with cough • Ht 71in, wt, 215 lbs • BMI=30 • Hgb=14.3 • No tobacco hx • Works as a welder, machinist in auto parts assembly BMJ 2008;336;598-600 6
2/23/06 • No evidence of obstruction by spirometry • Restriction by lung volumes • Low diffusing capacity Lung • Some desaturation with 6 transplant in minute walk 2004. • Chest CT: pulmonary fibrosis 5/03/06 Case 7 Lung Volumes: Gas Dilution • Helium Dilution • Inert tracer gas (He) of known initial concentration contained in a circuit of known volume (C 1 V 1 ) • Diluted by an unknown Compare to old PFTs Compare to old PFTs volume of gas from an additional source (patient) • Produced CO2 removed from system and absorbed oxygen replaced • Measure the new steady- state helium concentration (C2) • C 1 V 1 =C 2 V 2 Pulmonary Physiology, Levitsky, 2007 7
Case 8 Lung Volumes • Limitation of gas dilution • Assumes all areas of lung equally ventilated • Underestimates lung volumes in obstructive disease • Communicating gas volumes • Leaks Lung Volumes: Body Plethysmography • Based on Boyle’s Law: P 1 V 1 =P 2 V 2 • Patient seated within a body box and breathes through a mouthpiece to outside atmosphere via a shutter • Body box is a closed system and with inspiratory and expiratory efforts • Pressure changes within the lung, measured at the mouth • Resulting changes in the lung volume (thoracic gas volume) • Changes in the lung volume result in PFTS: Severe restriction opposite changes In the body box Reduced DLCO system pressure Dx: Kyphoscoliosis Pulmonary Physiology, Levitsky, 2007 8
Case 9 Case 10 • 76yo WM with progressive SOB and cough • 50PY tob hx • Mild obstruction by spirometry • Mild restriction by lung volumes • Severely reduced DLCO • Increased ERV Case 11 • Mixed obstruction and restriction pattern • Decreased DLCO • 24yo WM admitted with SOB/DOE, wheezing, • Dx: emphysema + inspiratory stridor pulmonary fibrosis • No PMHx, medications • PSHx sig for exp lap 6 months prior after MVA • 2 PY Tob hx, occ EtOH • Dx with asthma but no improvement with meds 9
Flow-Volume Loop • Normal spirometry • Decreased peak flow 50% • Consistent with asthma • No obstruction • Tech notes: Patient with stridor during spirometry Pulmonary Physiology, Levitsky, 2007 Case 12: Fixed airway obstruction • • Post-intubation tracheal stenosis/stricture • 46 F with recent dx of asthma 10
Calibrate Machine • Frequent checks with 3 liter syringe • Biological control – no more than 5% variation in FVC and FEV1 per week. • No use of short acting bronchodilators for 4 hours prior to testing. • Long acting β agonists or aminophylline should be held for 12 hours. Interpretative strategies for lung function tests. SERIES ‘‘ATS/ERS TASK FORCE: STANDARDISATION OF LUNGFUNCTION TESTING’’ Eur Respir J 2005 11
Case 13 Echocardiogram: • The right ventricular systolic pressure is calculated at 49 mmHg. There is evidence of moderate pulmonary • 26yo AAF with • Right Ventricle: The right ventricle is slightly progressive dilated. The right ventricular global systolic SOB/DOE function is mildly reduced. • Ht 61in, wt 100 lbs • BMI=19 • Hgb=11.3 • 7 PY tob hx Diffusing Capacity • Normal spirometry • Capacity of the lungs to exchange • Normal lung gas across the alveolar-capillary interface volumes • Most common technique based on • Low diffusing CO uptake • Function of capacity • Flow delivery of CO to • Significant alveoli • Mixing and diffusion of CO desaturation with to airways and alveoli normal walk • Transfer of CO across gas/liquid interface distance • Mixing and diffusion of CO • DDx: in the lung parenchyma/capillary • Pulm HTN plasma • Diffusion across RBC • Early ILD membrane • Chemical reaction with Hgb Swiss Med Wkly 2009;139(27–28):375–386 Respir Care 2003;48(8):777–782. 12
Case 16 Case 15 • 26 yo WF with dyspnea • PMHx of cystinosis • 26 yo WF with dyspnea • PFTS: • Restriction • Reduced DLCO but normal when adjusted for lung volumes • No desaturation when walking • Reduced maximum inspiratory pressure • Dx: Dyspnea secondary to muscle weakness 13
Case 17 • 55yo WM with long standing asthma • PFTS: � Obstruction by spirometry � Increased RV c/w air trapping � Increased DLCO • Asthma • Obesity • Polycythemia, cardiac shunts, alveolar hemorrhage 14
Recommend
More recommend