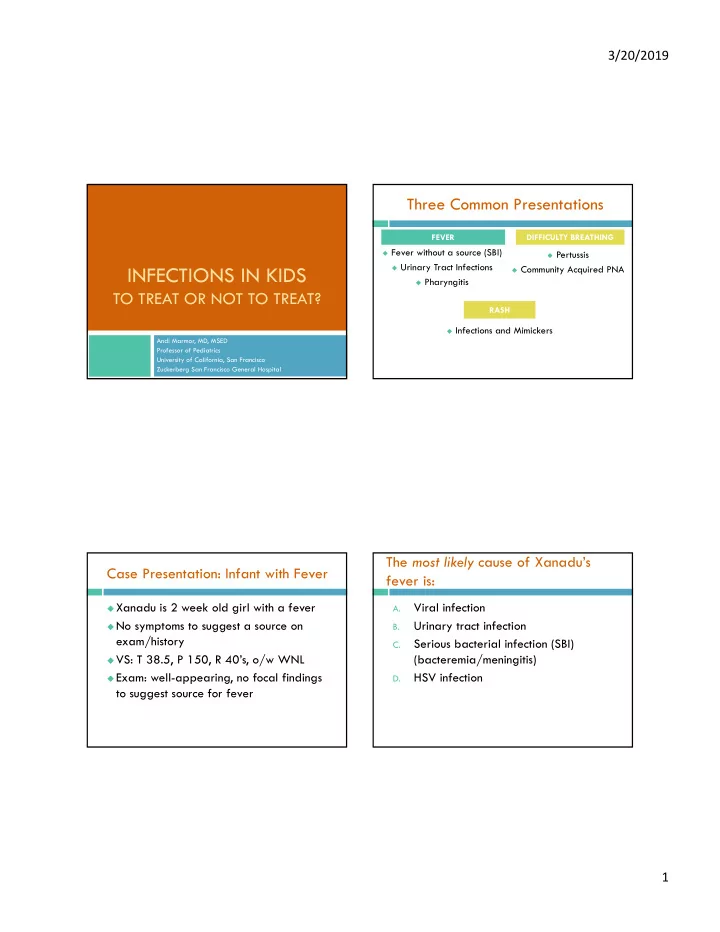
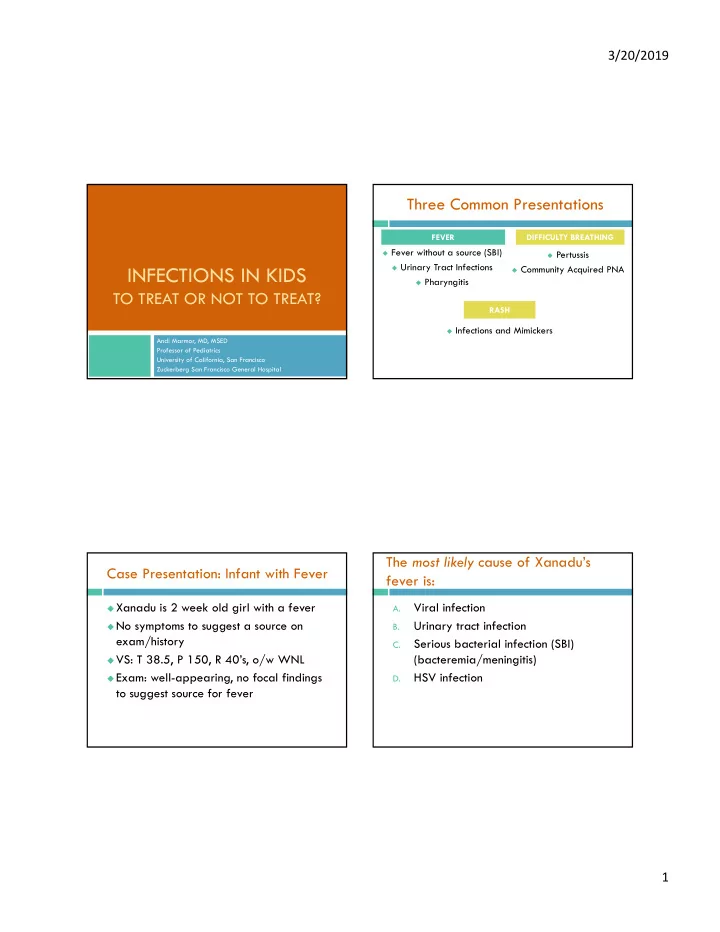
3/20/2019 Three Common Presentations FEVER DIFFICULTY BREATHING Fever without a source (SBI) Pertussis Urinary Tract Infections INFECTIONS IN KIDS Community Acquired PNA Pharyngitis TO TREAT OR NOT TO TREAT? RASH Infections and Mimickers Andi Marmor, MD, MSED Professor of Pediatrics University of California, San Francisco Zuckerberg San Francisco General Hospital The most likely cause of Xanadu’s Case Presentation: Infant with Fever fever is: Xanadu is 2 week old girl with a fever Viral infection A. No symptoms to suggest a source on Urinary tract infection B. exam/history Serious bacterial infection (SBI) C. VS: T 38.5, P 150, R 40’s, o/w WNL (bacteremia/meningitis) Exam: well-appearing, no focal findings HSV infection D. to suggest source for fever 1
3/20/2019 Everything you need to know about SBI in febrile infants - on ONE SLIDE 2-3% E.Coli>GBS>S. aureus >enterococcus, S pneumo 13-18% E. Coli THE FEBRILE INFANT <1% E.Coli/GBS S. pneumo Greenhow, 2014 Schwartz, 2009, Gomez 2010, Greenhow, 2014 Fever without a source (FWS): Fever without a source (FWS): Infants <30 days Infants <30 days Empiric antibiotics: amp/gent or Appearance and standard lab criteria do not reliably rule out UTI/SBI in this age group amp/cefotax Kupperman, 2019: validated prediction rule using GBS, E. Coli > Staph, enteric GNR’s >> UA, ANC and PCT (n=913) enterococcus, S. pneumo Neg UA, ANC< 4090/µL, PCT < 1.71ng/mL Cefotaxime: covers staph, better CSF 2 pts missed by rule, both UTI > 30d (sens 97.7, NPV 99.6) penetration, but broader Ampicillin: previously included to cover Option 1: for Listeria- now very rare Urine, blood, CSF -> admit, empiric abx Cefotaxime alone being considered in some Option 2: settings Urine, blood ->If UA neg, ANC <4090 and PCT < 1.71, DO NOT treat with gentamicin alone admit without abx or LP 2
3/20/2019 Approach to Infant with FWS FWS: Infants 30-90 days no Stabilize, obtain cultures, Infant well-appearing? start antibiotics UTI still the most common bacterial source, Start IV treatment yes for pyelo UA+ Obtain urine for UA other SBI less likely no and culture and Infant >30 days? yes Observe off abx UA- blood for culture, ANC and PCT, admit ANC<4090 and Viral source more reliable PCT<0.71? LP and start yes no empiric abx no Named viral syndromes or + rapid viral test UA+ Start treatment for UTI/pyelo Infant > 90 days? Obtain urine for UA - Consider obtaining blood and culture (flu, RSV) SBI unlikely culture if < 2 mo yes UA- RVT+ Consider testing for UTI Obtain rapid viral Supportive care and Close follow up follow up test if available Inflammatory markers (CBC/CRP/PCT) RVT- WBC > 15 or < 5 CRP > 20mg/L Obtain blood for culture helpful in select infants PCT > 0.5ng/mL and inflammatory markers Ceftriaxone Markers WNL Well appearing, neg UA AND no viral source Follow cultures for 48h Close follow up Case Continued Since Xanadu is less than 30 days, and has no source for her fever, you obtain a UA/urine cx and blood cultures and URINARY TRACT INFECTIONS perform an LP (“PYELONEPHRITIS”) Her UA is positive for LE and nitrites Now what do you do? 3
3/20/2019 Risk of UTI in Infants with FWS Which infants <3 mo should we test for UTI? 20 20 Girls Girls 18 18 Uncirc Uncirc 16 16 Boys Boys 14 14 Circ Circ ALL infants < 3 mo, T>38 12 12 Boys Boys 10 10 8 8 Testing threshold ~2- 6 6 3% 4 4 2 2 0 0 0 1 m 3m 6m 12m 18m 0 1 m 3m 6m 12m 18m Which infants >3 mo* should we test for UTI? Who should we test for UTI? *T ≥ 39 for ≥ 48hrs 20 Girls All infants with FWS < 3 mo of age 18 Girls > 3 mo of age Uncirc 16 Boys FWS (>39) and < 24 months 14 Circ All Girls Boys > 3 mo of age 12 Boys 10 Circumcised: FWS (>39) and < 6 mo Circ boys <6 mo 8 Uncircumcised: FWS (>39) and < 12 mo Uncirc boys <12 mo 6 Additional Risk Factors: 4 Length of fever (> 2 days) 2 Testing threshold ~5% Race (non-black) 0 0 1 m 3m 6m 12m 18m 4
3/20/2019 Diagnostic Dilemmas Treatment Collection of urine Empiric treatment based on local E. Coli resistance By c atheter for: PO cephalexin safe, tasty, narrow spectrum Infants < 3 mo of age (high risk) IV if <2 mo, toxic or not tolerating PO Ill-appearing/getting antibiotics Consider bag collection for: Total course: 7-14 days (for pyelo) Low-risk infant (circ boy> 3 mo, girl/boy>1 year) Imaging after UTI If UA +, consider cath for culture Results: U/S in infants <3 mo, older kids if recurrent + UA: start empiric treatment, send for cx Voiding Cystourethrogram (VCUG) only if high Neg UA: UTI very unlikely, even in young infants grade VUR/obstruction on U/S Consider sending for culture in high risk neonate Roberts 2011; Pediatrics 128(3):595–610 What is Zaffre’s “modified Centor Case Continued score?” Xanadu’s 6 yo brother Zaffre also has a 1 A. fever, and is complaining of a sore throat 2 B. His temp is 38.9, he has tender cervical 3 C. LAN and no cough or runny nose 4 D. 5 E. www.accesspediatrics.com 5
3/20/2019 Modified Centor Score Modified Centor Score 1 point each: 1 point each: Exudate or swelling on tonsils Exudate or swelling on tonsils?? Tender/swollen ant cervical LN’s Tender/swollen ant cervical LN’s Temp > 38C Temp > 38C Cough absent Cough absent Age 3-14 Age 3-14 ____________ ____________ Max score = 5 Score = 4-5 What does this mean? Case Presentation: 3 yo with cough What is Zaffre’s prior probability of a + Amaranth is a 3 yo who presents with 2 GAS culture? weeks of cough, keeps her awake, and occasional post-tussive vomiting ~25% A. She has a PMH of bronchiolitis (6 mo) and ~50% B. is up to date for age on vaccinations ~75% C. VS: T 38.2, P 130, RR 42, O2 sat 95% ~90% D. Her mother wants to know if this could be “the whooping cough” 6
3/20/2019 Pertussis Epidemiology Tdap Acellular pertussis PERTUSSIS Phases of Pertussis Pertussis: Clinical Diagnosis Cough lasting >2 weeks + 1of the following: PHASE TIME COURSE DESCRIPTION Apnea* Neonates/young Infants Catarrhal 1-2 weeks Mild fever, cough, rhinorrhea Paroxysms of coughing Paroxysmal 1-6 weeks Older infants/children: Older children Inspiratory “whoop” Paroxysms, whoop, post-tussive emesis Post-tussive vomiting ( least specific ) Young infants: apnea, cyanosis, bradycardia, poor feeding *May occur without cough Convalescent Weeks-Months Improvement in severity and frequency of coughing episodes Slide courtesy of Ellen Laves, MD cdc.gov/pertussis 7
3/20/2019 Pertussis: Treatment Pertussis: Laboratory Confirmation Major benefits: Lab confirmation ONLY in those with Prevent severe disease* in those at risk signs/symptoms consistent with pertussis Prevent spread to high risk (HR) patient Posterior NP specimen (not pharynx/ant NP) Empiric treatment: high suspicion and/or HR PCR for pertussis Infants <1 year (< 3mo, preemie at highest risk) False positives may occur Pregnant women near term Unimmunized or underimmunized Culture + for B. Pertussis Test and treat if +: Most SPECIFIC test HR but low clinical suspicion Most sensitive in first 3 weeks Patient LR but has HR contacts cdc.gov/pertussis *Only treatment BEFORE paroxyms may shorten course What is the RECOMMENDED next Case Continued step? Amaranth’s vaccination status and non- Obtain a PA and lateral CXR A. specific clinical symptoms make pertussis Obtain a blood culture and CBC B. less likely Obtain a sputum culture C. However, her RR (42) and O2 sat (95%) Start PO amoxicillin and discharge with make you concerned for pneumonia D. close follow up Well-appearing, in minimal resp distress aside from tachypnea Start IV cefuroxime and admit E. Decreased breath sounds with crackles over the LLL 8
3/20/2019 Pediatric CAP: Diagnosis Bradley JS, et al. Clin Infect Dis. 2011 Clinical Symptoms of acute illness (ie: fever) + resp distress (tachypnea*, retractions, hypoxia) AND PEDIATRIC COMMUNITY Focal lung findings on exam OR on CXR Imaging ACQUIRED PNEUMONIA Chest x-ray NOT recommended routinely in outpatients Does not distinguish between pathogens (viral, atypical, etc) *MOST SENSITIVE sign Pediatric CAP: Causes Pediatric CAP: Labs Bradley JS, et al. Clin Infect Dis. 2011 Bradley JS, et al. Clin Infect Dis. 2011 Based on age, severity, local resistance Routine lab testing NOT recommended Blood cultures: 2 MO TO 5 YRS: OVER 5 YEARS: Clinically worsening or hosp with mod/severe disease Viral testing (flu, RSV) Viral is most common M. pneumoniae , C. IF no evidence of bacterial co-infection pneumoniae > S. < 2 yrs: S. pneumoniae , C. CBC/CRP pneumoniae Trachomatis Not recommended 2-5 yrs S. pneumoniae, M. Testing for Mycoplasma pneumoniae, S. pneumo pneumoniae , H influenzae, If available, may guide antibiotic selection C. pneumoniae 9
Recommend
More recommend